|
Outpatient facilities have become an essential part of the healthcare industry. They offer a range of services, including diagnostic testing, surgery, and rehabilitation, to patients who don't require overnight hospitalization. As these facilities are often independent clinics or hospitals, the billing process can be complicated due to varying payer requirements and regulatory compliance rules. The billing process is a critical aspect of healthcare administration that involves several steps to ensure proper reimbursement and accurate documentation. In this article, we'll explore the billing process for outpatient facilities and provide a detailed overview of the various reimbursement systems used.
Patient Registration: The first step in the billing process is patient registration, where the patient demographic information, insurance details, and other necessary information are collected. This information is used to verify insurance coverage and establish financial responsibility. During the registration process, patients are required to provide their insurance card and identification, and the information gathered is used to create a medical record for the patient. Accurate patient registration is critical to ensure that the billing process proceeds smoothly and efficiently. Coding and Documentation: Coding and documentation are critical steps in the billing process. Medical coders and billers review the medical record to identify the procedures and services provided to the patient. The medical record includes a description of the services provided, including diagnosis, procedures, and treatments. Medical coders use various coding systems, including Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS), and International Classification of Diseases (ICD-10-CM), to assign codes to the services provided. These codes are used to indicate the services provided, which are then used to bill the insurance company. Charge Capture: Charge capture is the process of capturing the charges associated with the services provided to the patient. The charges are based on the codes assigned to the services provided. Charge capture systems are used to automate the process of capturing charges, which reduces the likelihood of errors and improves the accuracy of the billing process. Charge capture systems can be integrated with electronic health record (EHR) systems to streamline the billing process. Claims Submission: Once the charges have been captured, the claims are submitted to the insurance company for payment. Claims can be submitted electronically or on paper, depending on the insurance company's requirements. Electronic claims submission is becoming more common due to its speed and accuracy. Claims submitted electronically are typically processed faster than paper claims. The claims submitted to the insurance company include the codes for the services provided, along with any supporting documentation. Reimbursement: The insurance company reviews the claims submitted and determines the amount of reimbursement. Reimbursement can be based on several factors, including the type of service provided, the geographic location, and the fee schedule of the insurance company. Reimbursement can also be affected by any contractual agreements between the healthcare provider and the insurance company. Once the insurance company has determined the amount of reimbursement, they will send payment to the healthcare provider. Appeals and Denials: Sometimes, claims are denied or only partially reimbursed. In these cases, the healthcare provider can appeal the decision or request additional information to support the claim. Appeals can be submitted electronically or on paper, depending on the insurance company's requirements. Denials can be caused by various factors, including coding errors, lack of medical necessity, or incomplete documentation. It's essential to identify the reason for the denial and address the issue before resubmitting the claim. Conclusion: Billing for outpatient facilities can be complex, requiring a detailed understanding of the billing process, coding systems, and reimbursement rules. The steps involved in the billing process include patient
0 Comments
Osteoarthritis is the most common form of arthritis in the knee. It is a degenerative, "wear-and-tear" type of arthritis that occurs most often in people 50 years of age and older, although it may occur in younger people, too. In osteoarthritis, the cartilage in the knee joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful bone spurs. Osteoarthritis usually develops slowly and the pain it causes worsens over time. I know it can be hard to determine if your patient's injection would need a prior authorization or precertificaton. It is always best that we verify our patients' coverage, benefits and eligibility. PRIOR AUTHORIZATION, PRECERTIFICATION & BILLING PROCESS - HYALURONAN ACID & VISCO THERAPIES FOR OSTEOARTHRITIS OF THE KNEE CPT CODES: 20605, 20606, 20610, 20611 HCPCS CODES: J7318, J7323, J7328, J3490, J7320, J7321, J7322, J7324, J7325, J7326, J7327, J7329, J7331, J7332 Let's look at a commonly published clinical policy and guideline for these visco and hyaluronan acid therapies. Pay attention to everything on this post because these can all be very helpful for your billing and in order to maximize reimbursement. Conservative Treatment: Physical therapy or pharmacotherapy/NSAIDs (e.g., non-steroidal anti-inflammatory drugs [NSAIDs], acetaminophen and/or topical capsaicin cream) Understanding Indications and Dosing: Intra-articular injections of sodium hyaluronate are proven and medically necessary when all of the following are met: 1. Diagnosis of knee osteoarthritis 2. Member has not responded adequately to conservative therapy which may include physical therapy or pharmacotherapy or injection of intra-articular steroids or member is unable to tolerate conservative therapy because of adverse side effects 3. The member reports pain which interferes with functional activities. --- ambulation, prolonged standing 4. The pain is attributed to degenerative joint disease/primary osteoarthritis of the knee. 5. There are no contraindications to the injections --- active joint infection, bleeding disorder 6. Dosing is in accordance with the US FDA approved labeling as follows. --- Durolane: Approved as a single injection --- Euflexxa: Approved for 3 injections --- Gel-One: Approved as a single injection --- Gelsyn-3: Approved for 3 injections --- GenVisc 850: Approved for 3-5 injections --- Hyalgan: Approved for 5 injections --- Hymovis: Approved for 2 injections --- Monovisc: Approved as a single injection --- Orthovisc: Approved for 3-4 injections --- Supartz: Approved for 3-5 injections --- Synojoynt: Approved for 3 injections --- Synvisc One: Approved as a single injection --- Synvisc: Approved for 3 injections --- Triluron: Approved for 3 injections --- TriVisc: Approved for 3 injections --- Visco-3: Approved for 3 injections Learn how to properly bill and report these HCPCS codes for maximized reimbursement. READ HERE! Common Criteria and Utilization Limitations: Initial Determination: --- therapy has not resulted in functional improvement after at least 3 months Reauthorization/Continuation --- At least 6 months have passed since the prior course of treatment for the respective joint Intra-articular injections of sodium hyaluronate are unproven and not medically necessary for treating any other indication due to insufficient evidence of efficacy including, but not limited to the following: ----- Hip osteoarthritis ----- Temporomandibular joint osteoarthritis ----- Temporomandibular joint disc displacement Hyaluronic acid gel preparations to improve the skin's appearance, contour and/or reduce depressions due to acne, scars, injury or wrinkles are considered cosmetic and are not covered. Contraindications: 1. Do not administer to patients with known hypersensitivity (allergy) to hyaluronate preparations or allergies to avian or avian-derived products (including eggs, feathers, or poultry). This contraindication does not apply to Orthovisc. 1. Do not administer to patients with known hypersensitivity (allergy) to gram positive bacterial proteins. This contraindication applies to Orthovisc only. 1. Do not inject sodium hyaluronate into the knees of patients with infections or skin diseases in the area of the injection site or joint. Imaging Requirements: (MRI, CT, XRAY, U/S):X-ray, CT, or MRI reports), Color Doppler ultrasound (CDUS) and synovitis scores Pain Relief: Knee Osteoarthritis (OA) --- single 6 ml IA injection of hylan G-F 20 provided better pain relief over 26 weeks Sodium Hyaluronate Product Therapy Using Preferred Products (Durolane, Euflexxa, and Gelsyn-3) >>Medical notes documenting all of the following: --- Current prescription --- diagnosis of OA of the knee --- Conservative treatment tried for at least 3 months including response --- Signs and symptoms --- Current functional limitations --- Complete report(s) of diagnostic imaging (X-ray, CT, or MRI reports) --- Previous sodium hyaluronate treatment provided including the brand name of the drug, course of treatment, and response --- Dose, frequency, interval since previous sodium hyaluronate treatment --- Physician treatment plan Medical Necessity Cross-over: M17.0 -- Bilateral primary osteoarthritis of knee M17.10 -- Unilateral primary osteoarthritis, unspecified knee M17.11 -- Unilateral primary osteoarthritis, right knee M17.12 -- Unilateral primary osteoarthritis, left knee M17.2 -- Bilateral post-traumatic osteoarthritis of knee M17.30 -- Unilateral post-traumatic osteoarthritis, unspecified knee M17.31 -- Unilateral post-traumatic osteoarthritis, right knee M17.32 -- Unilateral post-traumatic osteoarthritis, left knee M17.4 -- Other bilateral secondary osteoarthritis of knee M17.5 -- Other unilateral secondary osteoarthritis of knee M17.9 -- Osteoarthritis of knee, unspecified Learn how to Bill for HYALURONAN ACID & VISCO THERAPIES FOR OSTEOARTHRITIS OF THE KNEE References: Clinical Policies of Commercial Payers and Medicare from published in the public domains. CPT Codes are a trademark and owned by the American Medical Association. ICD-10 Code book of 2022. Categories All Archives July 2024 Effective November 1, 2021 United Healthcare will require you to request Prior Authorization for the following services for Interventional Pain Management. This is effective November 1, 2021. Notice that mostly are for your Cervical & Thoracic regions. Notice that it is also required for your Genicular Nerve Block (but NOT for the Genicular Nerve RFA) and SI (but for the RFA). Codes that require Prior Authorization from UHC:United Healthcare Pain Management Injection Requiring Prior Authorization Effective November 1, 2021 CPT Code Description 62292 INJECTION PX CHEMONUCLEOLYSIS 1/MLT LUMBAR 64620 DSTRJ NEUROLYTIC AGENT INTERCOSTAL NERVE G0260 INJ PROC SI JNT;ANES STEROID&TX AGT&ARTHROGRPH 62320 NJX DX/THER SBST INTRLMNR CRV/THRC W/O IMG GDN 62322 NJX DX/THER SBST INTRLMNR LMBR/SAC W/O IMG GDN 62324 NJX DX/THER SBST INTRLMNR CRV/THRC W/O IMG GDN 62325 NJX DX/THER SBST INTRLMNR CRV/THRC W/IMG GDN 62326 NJX DX/THER SBST INTRLMNR LMBR/SAC W/O IMG GDN 62327 NJX DX/THER SBST INTRLMNR LMBR/SAC W/IMG GDN 62350 IMPLANT SPINAL CANAL CATHETER 62351 IMPLANT SPINAL CANAL CATHETER 62360 INSERT SPINE INFUSION DEVICE 62361 IMPLTJ/RPLCMT FS NON-PRGRBL PUMP 64451 INJECTION AA&/STRD NERVES NRVTG SI JOINT W/IMG 64454 INJECTION AA&/STRD GENICULAR NRV BRANCHES W/IMG 64480 NJX AA&/STRD TFRML EPI CERVICAL/THORACIC EA ADDL 64484 NJX AA&/STRD TFRML EPI LUMBAR/SACRAL EA ADDL 64491 NJX DX/THER AGT PVRT FACET JT CRV/THRC 2ND LEVEL 64492 NJX DX/THER AGT PVRT FACET JT CRV/THRC 3+ LEVEL 64494 NJX DX/THER AGT PVRT FACET JT LMBR/SAC 2ND LEVEL 64495 NJX DX/THER AGT PVRT FACET JT LMBR/SAC 3+ LEVEL 64520 INJECTION ANES LMBR/THRC PARAVERTBRL SYMPATHETIC 64634 DSTR NROLYTC AGNT PARVERTEB FCT ADDL CRVCL/THORA 64636 DSTR NROLYTC AGNT PARVERTEB FCT ADDL LMBR/SACRAL 64640 DSTRJ NEUROLYTIC AGENT OTHER PERIPHERAL NERVE Read more about this update here: https://www.uhcprovider.com/content/dam/provider/docs/public/resources/network-bulletin/pain-inject-management-nb-appendix-auwww.uhcprovider.com/content/dam/provider/docs/public/resources/network-bulletin/pain-inject-management-nb-appendix-august-2021.pdfgust-2021.pdf Today is October 8, 2021. Have you not noticed your claims are being rejected by your practice management clearinghouse as "Invalid ICD-10 Code"? ICD-10 Pain Management Code M54.5 Deleted Effective October 1, 2021! Yes?! Well, it is because the ICD-10 code M54.5 for Low Back Pain is now deleted effective all date of service from October 1, 2021! So make sure you are aware of this and correct your claims by choosing the billable and appropriate ICD-10 code that will describe your deleted code M54.5. Belo are some potential code replacements that you can use beginning October 1, 2021
New Codes you can potentially use: Remember that when changes like this happens, this is not just for CMS Medicare claims but it applies to all commercial payers (at least the big insurance payers!). Read more about this updates and change by clicking here https://www.cms.gov/medicare/icd-10/2022-icd-10-cm How to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers  Many physician groups or even individual solo practice offices are not happy with their contracted rates or the way they are being reimbursed by the insurance payers? Is it time to negotiate? when is the best time to negotiate your contract? There is no better time than NOW! But there are important steps that you need to do before doing so. Negotiating your contract is not only by picking up the phone and calling the insurance payer's provider services department and asking them that you would like to negotiate your contracted fees. Unfortunately, it doesn't work that way! But there are important steps that you need to do before doing so. Negotiating your contract is not only by picking up the phone and calling the insurance payer's provider services department. It doesn't work that way! Here are my tips: How to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers
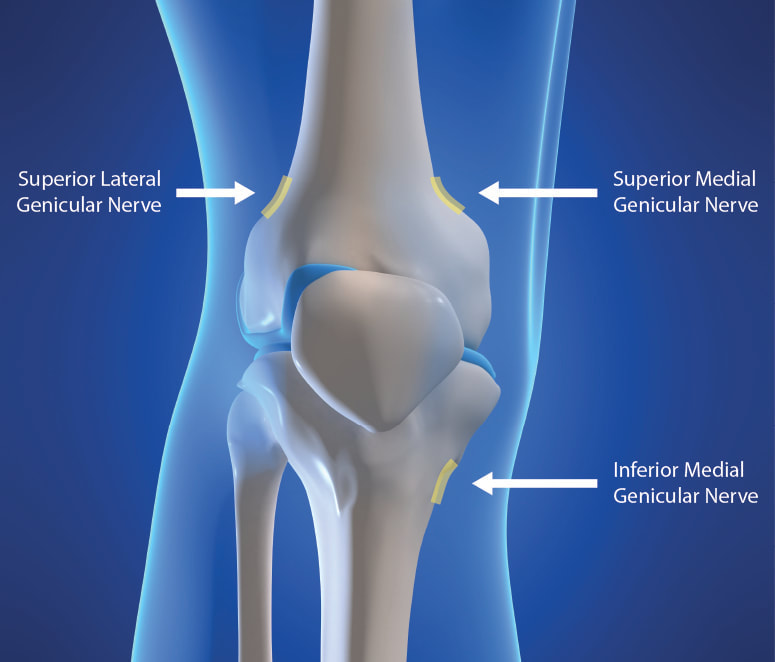
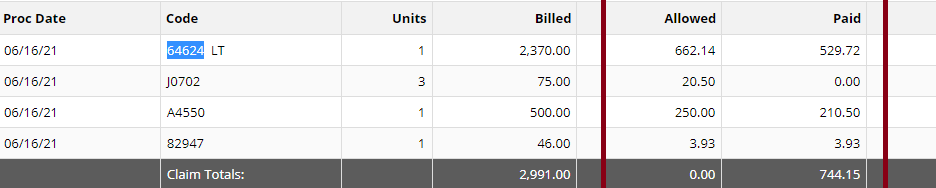
You need to present your reasoning why you think its time to negotiate your fees! All of the above, you can present it to the Insurance Payer through the Network Area Manager. Put them all together. Document everything! You can initiate the process by calling, and then by sending a formal letter of intent to renegotiate your contract rates or fee schedule. Don't forget to involve your billers and coders in this project! Let your patients leave feedback, reviews and about their experience in your practice! All these will surely help get you a better deal. It's a bit of a process but just be patient and work on it. Do you need help on how to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers? You should contact us today!Understanding the Genicular Nerves (image below)Do you remember the struggle when we didn't have the specific code for the Genicular Nerve Knee Block and for the ablation or the RFA? Prior to January 1, 2020, we used to code them using 64450 for the Peripheral Nerve Block and the you used the 64640 for the Ablation. Not only that, you need to know the nerves that were blocked or were RFA'ed. But Effective January 1, 2020, we have now a specific code for the Genicular Nerve Knee Block and the Genicular Nerve Knee Ablation. You can read more about that change in our blog. CLICK HERE. CPT 64454 Genicular Nerve Block Injection(s), anesthetic agent(s) and/or steroid; genicular nerve branches, including imaging guidance, when performed CPT 64624 Genicular Nerve Ablation or RFA Destruction by neurolytic agent, genicular nerve branches including imaging guidance, when performed Unfortunately many of our Pain and Orthopedic Physicians are still struggling getting reimbursed for these services even though we already have these specific codes in place since 2020. And why is that? There are common issues why: 1) Their billing staff are still using the old codes CPT 64450, CPT 64640 instead of the CPT Code 64454 and 64624 for the Genicular Nerve Block and Radiofrequency Ablation; 2) What I found is that, this is considered as Investigational and Experimental based on the following guideline when being reported: Genicular nerve blocks and genicular nerve ablation are considered investigational and not medically necessary for the treatment of chronic knee pain, including but not limited to any of the following:
But I have also read that there are two CMS Contractors who covers for this procedure based on Medical Necessity. See Group 1 Diagnosis Codes Cross Over: Group 1 DX Codes:
Read more about guidelines: National Government Services Inc Billing and Coding: Peripheral Nerve Blocks (A57452) First Coast Service Options, Inc Billing and Coding: Peripheral Nerve Blocks (A57788) More Guidelines from Payers which consider the procedure to be Investigational: Aetna Healthcare Anthem Blue Cross Blue Shield How do you handle Denial and Appeal for Genicular Nerve Ablation or Genicular Nerve Block? Here are my tips: Avoid the denials in the first place! by knowing your payers' guidelines; If the Provider says its Medically Necessary for the patient to receive the genicular nerve block or genicular nerve ablation, try getting a Predetermination based on Medical Necessity from your Payer! They will not allow you to submit Prior Authorization because for sure, it does not need Prior Authorization because its not a covered benefit based on their policy because the payer considers it "investigational" or "experimental"; Insist on reviewing Predetermination based on Medical Necessity instead! Already having denied claims? - pursue the claims by sending appeals, get your patient get involved with the appeals process. Be prepared with your medical documentation! How's the Patient's Pain Relief? Duration of Pain Relief? Improved ADL? - include that all in your documentation! Searched Keywords: GENICULAR NERVE BLOCK DENIAL AND APPEAL CPT BILLING CODE 64454 This is how it looks like when you get paid for Genicular Nerve Knee RFAgenicular-nerve-block-denial-and-appeal.html. Does this not look nice? HOW TO GET PAID FOR GENICULAR NERVE KNEE INJECTIONS Need help how to Appeal your claims? Contact Us today! Need help how to obtain Pre-determination before you render the Genicular Nerve Block to your patients? You should contact us today! NEW CPT Code 99072 and CPT Code 86413 DURING COVID19 PANDEMIC These 2 new CPT Codes 99072 and 86413 were published on September 8th 2020 and are effective immediately.  Let's describe these 2 new CPT Codes. CPT Code 99072 Additional supplies, materials, and clinical staff time over and above those usually included in an office visit or other non-facility service(s), when performed during a Public Health Emergency as defined by law, due to respiratory-transmitted infectious disease Take Note: This new code 99072 is reported only during a PHE (Public Health Emergency) and only for additional items required to support a safe in-person provision of evaluation, treatment, or procedural service(s). CPT Code 86413 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]) antibody, quantitative According to the AMA: "The first addition, CPT code 99072, was approved in response to sweeping measures adopted by medical practices and health care organizations to stem the spread of the novel coronavirus (SARS-CoV-2), while safely providing patients with access to high-quality care during in-person interactions with health care professionals. The additional supplies and clinical staff time to perform safety protocols described by code 99072 allow for the provision of evaluation, treatment or procedural services during a public health emergency in a setting where extra precautions are taken to ensure the safety of patients as well as health care professionals. The AMA/Specialty Society RVS Update Committee (RUC) worked with 50 national medical specialty societies and other organizations over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency and submitted recommendations today to the Centers for Medicare and Medicaid Services to inform payment of code 99072." "The second addition, CPT code 86413, was approved in response to the development of laboratory tests that provide quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) of SAR-CoV-2 antibodies provided by laboratory tests reported by other CPT codes. By measuring antibodies to SARS-CoV-2, the tests reported by 86413 can investigate a person’s adaptive immune response to the virus and help access the effectiveness of treatments used against the infection." Must be reported only once per in-person! (read more below) Code 99072 is to be reported only once per in-person patient encounter per provider identification number (PIN), regardless of the number of services rendered at that encounter. In the instance in which the noted clinical staff activities are performed by a physician or other qualified health care professional (eg, in practice environments without clinical staff or a shortage of available staff), the activity requirements of this code would be considered as having been met; however, the time spent should not be counted in any other time-based visit or service reported during the same encounter. CPT Guidelines, Q&A from the American Medical Association: Understanding PHE or Public Health Emergency in coordination with CPT Code 99072 Question: Code 99072 is stated as being applicable “during a PHE.” What information should be used to verify when a PHE is in effect? Answer: A PHE is in effect when declared by law by the officially designated relevant public health authority(ies). Understanding Patient Encounters Type for the determination of CPT Code 99072 Question: For what type of patient encounters or services should code 99072 be reported? Answer: Code 99072 may be reported with an in-person patient encounter for an office visit or other non-facility service, in which the implemented guidelines related to mitigating the transmission of the respiratory disease for which the PHE was declared are required. Use of this code is not dependent on a specific patient diagnosis. For a list of POS codes with facility/non-facility designations that are available in the Medicare Claims Processing Manual, visit https://www.cms.gov/Medicare/Coding/place-of-service-codes. Understanding Documentation Requirements when reporting CPT Code 99072 Question: What documentation is required to report code 99072? Answer: Given that code 99072 may only be reported during a PHE, one would not report this code in conjunction with an evaluation and management (E/M) service or procedure when a PHE is not in effect. Therefore, code 99072 is reported justifiably only when health and safety conditions applicable to a PHE require the type of supplies and additional clinical staff time explained in the code descriptor. Documentation requirements may vary among third-party payers and insurers; therefore, they should be contacted to determine their specifications. How about CPT Code 99072 with CPT Code 99070? Question: May code 99072 be reported with code 99070? Answer: Yes, code 99072 may be reported with code 99070 when the requirements for both codes have been met. Note that eligibility for payment, as well as coverage policy, is determined by each individual insurer or third-party payer. Reader's QUESTION - how much are you going to be reimbursed for these 2 new codes?  Reference sources: https://www.ama-assn.org/press-center/press-releases/ama-announces-new-cpt-codes-covid-19-advancements-expand https://www.ama-assn.org/system/files/2020-09/cpt-assistant-guide-coronavirus-september-2020.pdf CPT Assistant September 2020 Special Addition CPT is a trademark and owned by the American Medical Association. Understanding Shingrix Zoster Vaccine CPT Code 90750Key points to remember in properly billing and coding for Shingrix: Keypoints to remember!
CPT Code Shingrix 90750 What's the reimbursement? CPT Code Shingrix 90750 - What's the reimbursement? I called the manufacturing company of Shingrix at GSK or Global Smith Klein and contacted their Provider Reimbursement support at Phone: 1-855-636-8291. Unfortunately they told me they don't have a national average rate on how much you can get reimbursed per unit for the Shingrix shot. Understandably because it is based on Payer's reimbursement policy. I did some research some more research and found this: From Medicaid North Carolina: ICD-10-CM diagnosis code required for billing is Z23 - Encounter for immunization. Providers must bill with CPT code: 90750 - Zoster (shingles) vaccine, (HZV), recombinant, sub-unit, adjuvanted, for intramuscular injection. One Medicaid unit of coverage is 0.5 mL. The maximum reimbursement rate per unit is $144.20. Providers must bill 11-digit National Drug Codes (NDCs) and appropriate NDC units. The NDCs are 58160-0823-11 and 58160-0819-12. The NDC units should be reported as “UN1.” You can read the complete post here - https://medicaid.ncdhhs.gov/blog/2018/02/07/billing-guidelines-zoster-vaccine-recombinant-adjuvanted-suspension-intramuscular Conclusion: It is always best that your verify your patient's benefits and eligibility for the Shingrix - Zoster Vaccine. As with Medicare, they should be under the beneficiary's Part D benefits. I hope this post helps. Understanding the 2020 CPT codes 99421, 99422, 99423 Online Digital Evaluation and Management, E/M Services for Physicians and Non-Physicians Practitioners Your Billable Codes for Digital CPT Codes are as follows: CPT Code 99421 Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes CPT Code 99422 Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11– 20 minutes CPT Code 99423 Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes. These codes are for use when E/M services are performed, of a type that would be done face-to-face, through a HIPAA compliant secure platform. These are for patient-initiated communications, and may be billed by clinicians who may independently bill an E/M service. They may not be used for work done by clinical staff or for clinicians who do not have E/M services in their scope of practice. Report these services once during a 7-day period, for the cumulative time. According to CPT®: “The seven-day period begins with the physician’s or other qualified health care professional’s (QHP) initial, personal review of the patient-generated inquiry. Physician’s or other QHP’s cumulative service time includes review of the initial inquiry, review of patient records or data pertinent to assessment of the patient’s problem, personal physician or other QHP interaction with clinical staff focused on the patient’s problem, development of management plans, including physician or other QHP generation of prescriptions or ordering of tests, and subsequent communication with the patient through online, telephone, email, or other digitally supported communication, which does not otherwise represent separately reported E/M service.” So how about the Clinicians who may not independently bill for evaluation and management visits? Here are your codes: For Commercial Insurance Payers, use the following codes: CPT Code 98970 Qualified nonphysician health care professional online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5-10 minutes CPT Code 98971 Qualified nonphysician health care professional online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 11-20 minutes CPT Code 98972 Qualified nonphysician health care professional online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 minutes or more Reference: Per CPT, CPT© E/M services codes 98970—98972 that says: Per CPT; “For online digital E/M services provided by a qualified nonphysician health care professional who may not report the physician or other qualified health care professional E/M services (eg, speech-language pathologists, physical therapists, occupational therapists, social workers, dietitians), see 98970, 98971, 98972).” And how about for Medicare Beneficiaries?For Medicare Beneficiaries, they have a set of HCPCS Codes that we can use (CMS does not recognize CPT Codes 98970-98972) - continue reading below HCPCS Code G2061: Qualified non-physician healthcare professional online assessment and management, for an established patient, for up to seven days, cumulative time during the 7 days; 5–10 minutes HCPCS Code G2062: Qualified non-physician healthcare professional online assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 11–20 minutes HCPCS Code G2063: Qualified non-physician qualified healthcare professional assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 21 or more minutes. References: CPT 2020, CMS Guideline and Finial Ruling. Need more help? Contact us today! (732) 982-4800January 1, 2020 - we now have a new Pain Management Code CPT 64625 - SI Ablation Description of CPT Code 64625 Radiofrequency ablation, nerves innervating the sacroiliac joint, with imaging guidance (Fluoroscopic or Computed Tomography). Keypoints to REMEMBER!
Need help? Contact our office today!Let's decribe this code: CPT 76140 Consultation on x-ray examination made elsewhere, written report. (2D reformatting is no longer separately reported. To report 3D rendering, see 76376, 76377) So the question is, can a Provider bill for X-ray review using CPT Code 76140? Sharing to you coding clarification here. (Source are from CPT Assistant as published by the AMA). CPT is a trademark and owned by the American Medical Association. CPT Assistant October 1997
Using CPT Code 76140 76140 Consultation on x-ray examination made elsewhere, written report. You would use this code when a physician's opinion or advice regarding a specific film is requested by another physician and upon examination of the film, the consulting physician renders his or her consultation (ie, or his/her opinion or advice) to the requesting physician in the form of a written report. If a patient presents to an office for a new patient visit and brings to the physician his or her medical records, including x-rays, you should not report code 76140. Although the x-rays may have been taken elsewhere, the physician does not perform a consultation as intended by code 76140. Rather, the review or re-read of the x-rays would be considered part of the face-to-face E/M service provided to the patient. Again, the E/M codes include work done before, during, or after the E/M visit. Review of x-rays is part of the E/M service. Remember, 76140 represents a consultation, in which a physician only renders an opinion or gives advice regarding the film in the form of a written report. In general, when reporting 76140, the physician is not concurrently providing an E/M face-to-face service to the patient. When Medicare is a Primary Insurance for the patient, the patient's part responsibility (coinsurance/deductible) normally crosses over to its secondary insurance for secondary coverage (if Medicare has the secondary insurance on file or if its set up to cross over based on the patient's coordination of benefits).
As you will notice on your Remittance advise, "Claim Information forwarded to: (insurance company here) Meaning, Medicare will forward the information to the secondary insurance. If not, try to find out if there is a secondary insurance for the patient, then you need to send the paper claim (using the HCFA 1500 form for Office/Provider/Professional Claims) to the secondary and attach a copy of the Medicare EOB (explanation of benefits). If your Practice Software can bill secondary to Medicare electronically, then that's great! Send them by electronic. If your practice management software is capable of doing this by electronic submission with attached copy of the EOB - much better!After you submit the claim to the secondary insurance, the secondary insurance EOB will then tell you if there is a copay being applied towards the patient being a secondary insurance after Medicare.You will then obviously collect that copay based on your contract with the secondary insurance company (and this is also based on the patient's contract with his/her secondary insurance). Medicare patients are mostly aware of their responsibility after the secondary insurance picks up. Bottom line here: (1) Medicare must process (not deny or reject!) the claim first being the primary; (2) Secondary insurance must then process the claim with Medicare's claim information; (3) Then, if there is a copay being applied towards the patient's responsibility -- you have to bill your patient for that copay!But honestly, I do not collect secondary insurance copay not until the secondary insurance had processed the claim (after Medicare's allowance!). WHY? because it is possible that the patient may no longer have an active policy (at the time of service) with the secondary insurance, or maybe, there is no more copay because the patient had met his/her out of pocket limit. So to streamline this issue (of which not all offices are doing it) - you must always check benefits and eligibility for your patient's primary, secondary or even tertiary insurance coverage!It may be a lot of work too, but what I do is that, when I am billing the patient a copay (from the secondary insurance's determination and per the EOB) or even for their coinsurance! I do my best to attach a copy of the EOB on the statement. That way, the patient has a copy of the said EOB and he/she will understand why I am billing him/her. How do you describe CPT 99204? Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: a comprehensive examination; medical decision making of moderate complexity. Counseling and/ or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of moderate to high severity. Typically, 45 minutes are spent face-to-face with the patient and/or family. How do you report CPT 99205? - read below. Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 components: A comprehensive history; A comprehensive examination; Medical decision making of the complexity. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family needs. Usually, the presenting problems(s) are of moderate to high severity. Typically, 60 minutes are spent face-to-face with the patient and/or family CPT 99204 and or CPT 99205 Key Points:
Modifier 58 Staged or Related Procedure or Service During Postoperative Period by Same Physician  Guideline: The same physician planned, at time of original surgery/procedure, a return trip to operating or procedure room within 10 or 90 day post op days WHEN IT IS APPROPRIATE:
Physicians in same specialty, same group are to bill and are reimbursed as a single physician Key to Remember! Use modifier 78 (not 58!) for treatment problems unplanned requiring return trip to operating room If hardware removed in unplanned surgery return for a complication, (e.g. infection of the wound site or rejection of the hardware itself), modifier 78 appropriate It is NOT APPROPRIATE WHEN:
References:
CMS Medicare Website Coding Books Payers Websites UNDERSTANDING HOW TO USE MODIFIER 79  How to Use Modifier 79 How to Use Modifier 79 Per the Current Procedure Terminology® (CPT®) manual, the descriptor of modifier 79 is: • "Unrelated procedure or service by the same physician during the postoperative period." As indicated, this modifier is used to bill an unrelated procedure or service performed by the same physician during the postoperative period of a previous surgical procedure. When a patient has surgery performed, there is a postoperative period -- a period after the surgery has been performed when additional surgical care related to the initial surgery is considered already covered (and paid for) by the allowance provided for the initial surgery. The postoperative period can be zero or 10 days (minor surgical procedure) or 90 days (major surgical procedure). (Note that some surgeries are considered so minor that they have a zero day postoperative period, usually a very quick outpatient procedure.) Modifier 79 should be used when a surgical procedure is:
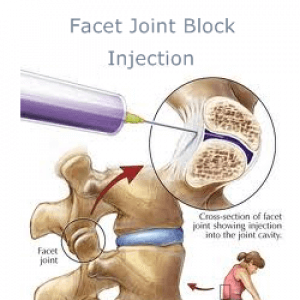
REMEMBER! When the 79 modifier is used, a new postoperative period for the second surgical procedure begins. Additionally, the remainder of the postoperative period of the original surgery is still applicable. References: Medicare CMS Website American Medical Association CPT Coding Books Payers Websites Still confused with Coding and reporting medial and lateral branch nerve blocks and understanding Pain Management procedures? Coding Billing for Medial and Lateral Nerve Blocks. According to the AMA, the code series for medial branch blocks and the facet joint injections are the same (i.e., CPT series 64490-64495), with reporting based on the number of facet joints injected, not the number of nerves injected. For example: If three (3) medial branch nerves are injected only two (2) facet joint injection codes would be reported despite the fact that three nerves were injected, since each facet joint is connected to two medial nerves. The lateral branch nerve is a peripheral nerve and would be reported with CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch, when a lateral branch nerve block is performed. Please note: CPT code 64450 should only be reported per nerve or branch and not per injection. CPT code 76942, Ultrasonic guidance for needle placement (e.g., biopsy, aspiration, injection, localization device), imaging supervision and interpretation, would be additionally reported when utilizing ultrasound guidance for certain nerve block procedures when it is not inherent in the primary procedure code. The Different kinds or types of NERVE BLOCKS and what are they targeting: NERVE BLOCKS: Brachial plexus block, elbow block, wrist block BODY AREAS: Shoulder, arm, hand, elbow, wrist) NERVE BLOCKS: Cervical epidural, thoracic epidural, lumbar epidural block BODY AREAS: Neck, back NERVE BLOCKS: Cervical plexus block, cervical paravertebral block BODY AREAS: Shoulder, upper neck NERVE BLOCKS: Maxillary nerve block BODY AREAS: Upper jaw NERVE BLOCKS: Ophthalmic nerve block BODY AREAS: Eyelids, scalp NERVE BLOCKS: Sphenopalatine nerve block BODY AREAS: Nose, palate NERVE BLOCKS: Subarachnoid block, Celiac plexus block BODY AREAS: Abdomen, pelvis NERVE BLOCKS: Supraorbital nerve block BODY AREAS: Forehead NERVE BLOCKS: Trigeminal nerve block BODY AREAS: Face CPT 64490, 64493, 64495, 64633 - Billing and Coding for Facet Nerve Block and Nerve Ablation RFA CPT CODE 64490 PARAVERTEBRAL FACET JOINT BILLING AND CODING WITH IMAGING GUIDANCEInjection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), cervical or thoracic; single level 64491 ----------- second level 64492 ----------- third and any additional level(s) level CPT CODE 64493Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), lumbar or sacral; single level 64494 ----------- second level 64495 ----------- third and any additional level(s) level FACET JOINT BILLING AND CODING WITH ULTRA-SOUND 0213T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; single level ....................................................................+ 0214T second level ....................................................................+ 0215T third and any additional level(s) 0216TInjection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, lumbar or sacral; single level ..................................................................+ 0217T second level ..................................................................+ 0218T third and any additional level(s) Billing and Coding for Radiofrequency Facet denervationCPT CODE 64633 Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); cervical or thoracic, single facet joint' +64634 cervical or thoracic, each additional facet joint (List separately in addition to code for primary procedure) CPT CODE 64635 Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); lumbar or sacral, single facet joint; +64636 lumbar or sacral, each additional facet joint (List separately in addition to code for primary procedure) Other Searched Keywords: Billing and Coding for RFA of Facet Joint Nerves Billing and Coding for Facet Joint AblationKey Points for CPT 64490, 64493, 64495, 64633 - Billing and Coding for Facet Nerve Block and Nerve Ablation RFA These codes are unilateral
 Let's look at these questions and answers: #1 Question "What are the appropriate code assignments when a patient receives 3 separate nerve blocks into the same lateral branch nerve? Would it be appropriate to report 3 units of this service?" The right CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch, would be appropriately reported only once in this case since all 3 nerve blocks were administered to the same nerve or branch. #2 Question "We are getting conflicting information regarding coding medial and lateral branch blocks S1, S2, and S3, Medial 64493, 64494, Lateral 64493, and 64494. Our Pain Center wants to use facet injection for the medial branch block and other peripheral nerve for the lateral branch block. Are we correct in reporting lateral branch nerve block(s) to the peripheral nerve CPT code?" Yes, you are correct. The lateral branches of the dorsal sacral nerve plexus are considered peripheral nerves. Therefore, for the four lateral branch block injections at S1, S2, S3, and S4, report 4 units of CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch. Report multiple units of the injection for the four lateral branch block injections performed, modifier 59 would not be appended in this case. # 3 Question "A patient was seen at our facility and underwent a left-sided L5 and S1, S2, S3, and S4 lateral branch nerve block for diagnostic purpose with C-arm fluoroscopy. What are the correct codes for a lateral nerve block?" So OK, ... based on the operative report a medial branch nerve block was performed at the L5 and a lateral branch nerve block was performed at the S1, S2, S3 and S4 Therefore, it would be appropriate to report CPT code 64493, Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapohphyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), lumbar or sacral, single level, for the L5 medial branch block. For the 4 lateral branch block injections at S1, S2, S3, and S4, report 4 units of CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch. From AMA's CPT Assistant: February 2011 page 4 (In September 2011 questions relating to this article were discussed.) Revisions made to certain pain medicine procedures in the CPT 2011 codebook include new procedure codes, and guidelines were created in the Nervous System section to clarify the reporting of these services. The following code sets are affected: • Introduction/Injection of Anesthetic Agent (Nerve Block), Diagnostic or Therapeutic (64400-64530) • Neurostimulators (Peripheral Nerve) (64550-64595) • Destruction by Neurolytic Agent (eg, Chemical, Thermal, Electrical or Radiofrequency) (64600-64681) Introduction/Injection of Anesthetic Agent (Nerve Block), Diagnostic or Therapeutic Revised Codes The following codes were revised for 2011: 64479Injection(s), anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance (fluoroscopy or CT); cervical or thoracic, single level 64480Injection(s), anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance (fluoroscopy or CT); cervical or thoracic, each additional level (List separately in addition to code for primary procedure) 64483Injection(s), anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance (fluoroscopy or CT); lumbar or sacral, single level 64484Injection(s), anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance (fluoroscopy or CT); lumbar or sacral, each additional level (List separately in addition to code for primary procedure) What exactly is "transforaminal epidural injection"? codes 64479-64484. TFE describe injections that enter the epidural space through the intervetebral foramen. This technique differs from interlaminar / translaminar epidural injection technique (62321-62327) and the paravertebral facet joint nerve injection technique (64490-64495). Since the vertebral artery (in the cervical spine), radiculomedullary arteries, as well as the spinal cord are in close proximity to the nerve root, this procedure involves a much higher risk with more work than a translaminar epidural injection. If ultrasound is used to guide the transforaminal injections, a code from the category III code set should be used instead of a code from the 64479-64484 code series. Therefore, parenthetical notes instruct users to report Category III codes 0228T, 0229T, 0230T, and 0231T for ultrasound-guided transforaminal epidural procedures. Additionally ultrasound guidance procedure code 76942, Ultrasound guidance for needle placement (eg biopsy, aspiration, injection, localization device), imaging supervision and interpretation, has been revised to clarify that it may not be used as guidance for 64479-64495 injections. Coding Tip Codes 64479-64484 are inherently unilateral procedures. When these procedures are performed bilaterally, they should be appended with modifier 50 or with a HCPCS Level II modifier "RT" or "LT" depending upon payer requirements. Paravertebral Spinal Nerves and Branches New Guidelines The paravertebral facet joint is the site of interaction between the vertebral bone above and below, and can be a source of pain. Injections can be made either into the joint, or at each of the nerves that supply the joint (ie, the medial nerve branches). To coordinate with the revision of codes 64479-64484, new parenthetical notes in the Paravertebral Spinal Nerves and Branches section of the CPT codebook direct users to the appropriate code to identify paravertebral facet joint injections when performed with imaging guidance. When performing a paravertebral facet injection into the T12-L1 joint, or at the nerves innervating that joint, code 64490 is reported. Fluoroscopy and CT imaging guidance and any injection of contrast are inclusive components of codes 64490- 64495. Imaging guidance and localization are required for the performance of paravertebral facet joint injections, as described by codes 64490-64495. If imaging guidance is not used, code 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s), or code 20553 , Injection(s); single or multiple trigger point(s), 3 or more muscle(s), should be reported instead of a code from the 64490-64495 code series. If ultrasound guidance is used, it is appropriate to report Category III codes 0213T-0218T. Coding Tip Paravertebral facet injection codes 64490-64495 and 0213T-0218T are unilateral. When performed bilaterally, they may be appended with modifier 50 or a HCPCS Level II modifier "RT" or "LT" depending on the requirements of the payer. Neurostimulators (Peripheral Nerve) New Codes Code 64573 was deleted and the following four new codes were added for 2011: 64566Posterior tibial neurostimulation, percutaneous needle electrode, single treatment, includes programming 64568Incision for implantation of cranial nerve (eg, vagus nerve) neurostimulator electrode array and pulse generator 64569Revision or replacement of cranial nerve (eg, vagus nerve) neurostimulator electrode array, including connection to existing pulse generator 64570Removal of cranial nerve (eg, vagus nerve) neurostimulator electrode array and pulse generator Code 64566 is reported for a treatment of voiding dysfunction (eg, urge incontinence), posterior tibial nerve stimulation. Code 64566 was created to describe a minimally invasive procedure that includes both the needle insertion through the skin adjacent to the tibial nerve, as well as the placement of an electrode on the surface of the skin. The treatment consists of a series of sessions involving insertions of a percutaneous needle electrode, with intermittent neuromodulation for approximately 30 minutes while the needle electrode remains in place. The neurostimulator includes a lead set with surface electrodes and a needle electrode, which produces an adjustable electrical pulse that travels to the sacral nerve plexus via the tibial nerve. The sacral nerve plexus then regulates the bladder and the pelvic floor functionality. Code 64566 would be reported once for each neurostimulation treatment session. References:
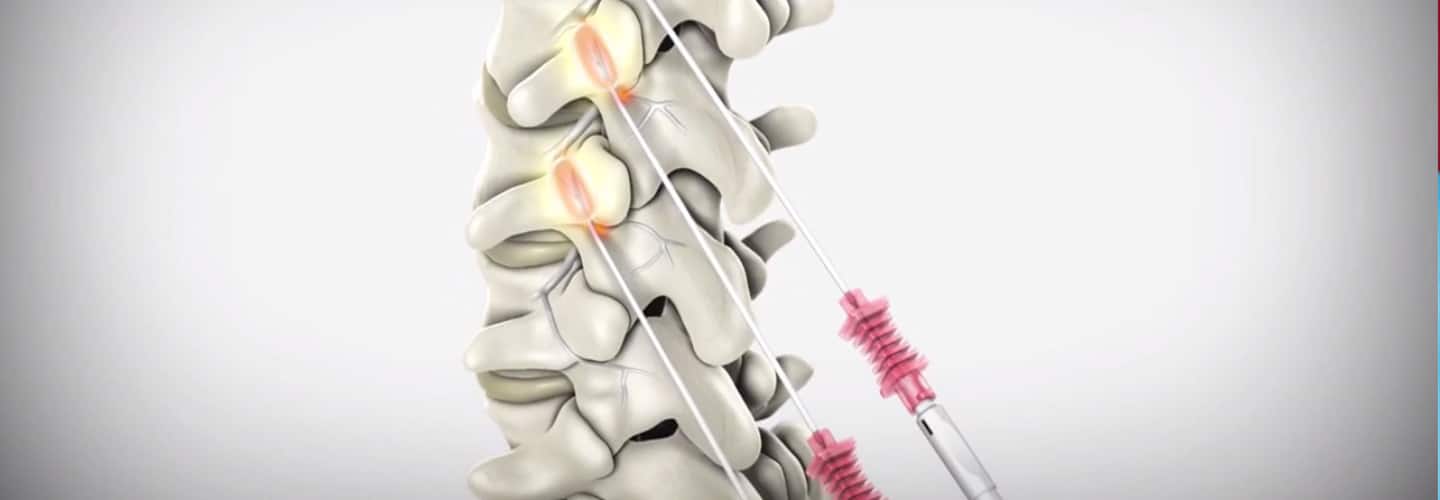
2017 / 2018 Coding Books (CPT is a Trademark and Owned by the American Medical Association) AMA's CPT Assistant Archives CMS Medicare Website (LMN, NCD/LCD, Manuals) Commercial Payers Guidelines Billing and Coding for Orthopedic Spinal Fusion Let's begin with some terminology to remember;
Understanding the Posterior Lumbar Interbody Spinal Fusion 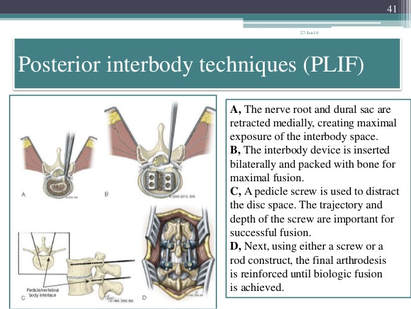 Techniques:
Image Source: https://www.slideshare.net/drpraveenktripathi/lumbar-interbody-fusion-indications-techniques-and-complications
Your CPT® Codes for PLIF and TLIF Spinal Fusion Coding: CPT Code 22630, +22632 22630 Arthrodesis, posterior interbody technique, including laminectomy and/or discectomy to prepare interspace (other than for decompression), single interspace; lumbar +22632 Each Additional interspace (list separately in addition to code for primary procedure code) Here's what occurs when 22630 is performed: The provider performs an arthrodesis, also known as spinal fusion, in the lumbar spine, or lower back, to permanently join two vertebrae, the interlocking bones of the spine. He excises the lamina and disk material and applies bone graft between the disks to fuse them. The procedure helps to alleviate persistent pain caused by various spinal conditions, including herniated intervertebral disks, stenosis, or spinal injuries. Then, in 2012 Code 22633 was introduced to to represent the combination of 22630 and 22612 Arthrodesis, posterior or posterolateral technique, single level; lumbar (with lateral transverse technique, when performed) at the same level. The Anterior Interbody Fusion Approach
Videos to watch for Procedure PLIF and TLIF Your CPT® Codes for ALIF, DLIF and OLIF Spinal Fusion Coding: CPT Code 22558, +22585 22558 Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace (other than for decompression); lumbar Remember: (For arthrodesis using pre-sacral interbody technique, see 22586, 0195T) +22585 Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace (other than for decompression); each additional interspace (List separately in addition to code for primary procedure) Remember: (Use 22585 in conjunction with 22554, 22556, 22558) (Do not report 22585 in conjunction with 63075, even if performed by a separate individual. To report anterior cervical discectomy and interbody fusion at the same level during the same session, use 22552) Here's what occurs when 22558 is being performed: The provider performs arthrodesis, also known as spinal fusion, in the lower back, to permanently join two vertebrae, the interlocking bones of the spine, to alleviate persistent pain caused by a herniated, or bulging, disk, or other spinal condition. He makes an incision in the abdomen to access the spine and remove disk material. Instrumentation may be required to stabilize the Spinal Fusion POSTERIOR INSTRUMENTATION: Add-Code +22840 Posterior non-segmental instrumentation (eg, Harrington rod technique, pedicle fixation across 1 interspace, atlantoaxial transarticular screw fixation, sublaminar wiring at C1, facet screw fixation) (List separately in addition to code for primary procedure) (Use 22840 in conjunction with 22100-22102, 22110-22114, 22206, 22207, 22210-22214, 22220-22224, 22310-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300-63307) Add-On Code +22841 Internal spinal fixation by wiring of spinous processes (List separately in addition to code for primary procedure) Add-On Code +22842 Posterior segmental instrumentation (eg, pedicle fixation, dual rods with multiple hooks and sublaminar wires); 3 to 6 vertebral segments (List separately in addition to code for primary procedure) Use 22842 in conjunction with 22100- 22102, 22110- 22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300- 63307)Text has been updated Add-On Code +22843 7 to 12 vertebral segments (List separately in addition to code for primary procedure) (Use 22843 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081,63085, 63087, 63090, 63101, 63102, 63170-63290,63300- 63307)Text has been updated Add-On Code +22844 13 or more vertebral segments (List separately in addition to code for primary procedure) (Use 22844 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300- 63307) ANTERIOR INSTRUMENTATION Add-On Code +22845 Anterior instrumentation; 2 to 3 vertebral segments (List separately in addition to code for primary procedure) (Use 22845 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081,63085, 63087, 63090, 63101, 63102, 63170-63290,63300- 63307)Text has been updated Add-On Code +22846 4 to 7 vertebral segments (List separately in addition to code for primary procedure) Use 22846 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300- 63307)Text has been updated Add-On Code +22847 8 or more vertebral segments (List separately in addition to code for primary procedure) (Use 22847 in conjunction with 22100-22102, 22110-22114, 22206, 22207, 22210-22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040- 63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290,63300-63307)Text has been updated Add-On Code +22848 Pelvic fixation (attachment of caudal end of instrumentation to pelvic bony structures) other than sacrum (List separately in addition to code for primary procedure) (Use 22848 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300- 63307)  Co-Surgeon Modifier 62 may not be appended with your Instrumentation Codes! Spinal Prosthetic Devices may also be required to be reported CPT Code 22853 22853 Insertion of interbody biomechanical device(s) (eg, synthetic cage, mesh) with integral anterior instrumentation for device anchoring (eg, screws, flanges), when performed, to intervertebral disc space in conjunction with interbody arthrodesis, each interspace (List separately in addition to code for primary procedure) Notes: (Use 22853 in conjunction with 22100-22102, 22110-22114, 22206, 22207, 22210-22214, 22220-22224, 22310-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300-63307) (Report 22853 for each treated intervertebral disc space) Code +22853 is one of several new codes within the spine section for the insertion of biomechanical devices that replace deleted code +22851 (Application of intervertebral biomechanical device[s] ...). The new add-on codes are more specific regarding the type and location of the biomechanical devices. CPT® guidelines direct you to report +22853 for each treated intervertebral disc space. Report +22853 in addition to the definitive procedure(s) since it is an add-on code. Do not append modifier 62 (Two surgeons) to 22853. The provider inserts a metallic cage or mesh device between two vertebrae and may use screws or flanges to attach it to the front part of the vertebrae; the device maintains the disc space, provides spinal stability, and yet preserves some range of motion, which helps relieve persistent pain caused by a herniated, or bulging, disk or other spinal condition. The provider performs this procedure during a spinal interbody arthrodesis procedure, which is fusion, or permanent joining, of vertebrae over the joint space. Remember! Code +22853 is an add–on code and must be reported with an appropriate primary procedure, such as 22548–22586 (Anterior or anterolateral approach technique arthrodesis procedures on the spine [vertebral column]), but there are many other codes that can be reported as a primary code. Report one unit of this code for each interspace treated, not for the number of devices inserted. For example, if the provider inserts two cages into a single interspace, you report this code only once. If the provider inserts a device at two separate interspaces, e.g., between C3–4 and C5–6, then you would report this code twice. This code is for the application of a device to expand or maintain an intervertebral disc space. For a similar procedure to cover a defect created by removal of a vertebral body, report 22854 (Insertion of intervertebral biomechanical device(s) [e.g., synthetic cage, mesh] with integral anterior instrumentation for device anchoring [e.g., screws, flanges], when performed, to vertebral corpectomy[ies] [vertebral body resection, partial or complete] defect, in conjunction with interbody arthrodesis, each contiguous defect [List separately in addition to code for primary procedure]). For insertion of a similar device to treat an intervertebral disc space or vertebral body removal defect but without interbody fusion (arthrodesis), report 22859 (Insertion of intervertebral biomechanical device[s] [e.g., synthetic cage, mesh, methylmethacrylate] to intervertebral disc space or vertebral body defect without interbody arthrodesis, each contiguous defect [List separately in addition to code for primary procedure]). Report Bone Grafting if allowable, CPT Code 20930 20930 Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition to code for primary procedure) Notes: (Use 20930 in conjunction with 22319, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) Here's what occurs when 20930 is being performed; The provider applies small pieces of donor or synthetic bone graft material during a spinal surgery to encourage bone growth during the healing period. Coding Tip! Code 20930 is an add on code and used for specified spinal procedures only. Check with your payer to determine if 20930 can be billed separately or if the application of the bone graft material is included in the code for the primary surgical procedure. Do not append modifier 62 to bone graft codes 20900-20938. (For spinal surgery bone graft[s] see codes 20930-20938) Check with your payer if you can separately report this code; +20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Notes: (Use 20931 in conjunction with 22319, 22532-22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) A provider uses a structural allograft, a type of donor bone, to fill in bony defects as she performs a spinal surgery procedure. Coding Tips: Code 20931 is an add on code describing application of structural allograft to spinal defects and must be reported with an allowable primary spinal procedure code. Report 20930, Allograft, morselized, or placement of osteopromotive material, for spine surgery only, together with 20931 only in the case of a human donor who is a different person from the recipient. You should never append modifier 50, Bilateral procedure, to 20931. The CMS Physician Fee Schedule Database includes a 9 indictor in the BILAT SURG column for this code. According to further CMS instructions, a 9 indicator in this column means that the concept of a bilateral surgery with spinal grafting does not apply. +20936 Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar fragments) obtained from same incision (List separately in addition to code for primary procedure) Notes: (Use 20936 in conjunction with 22319, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) A provider uses an autograft, a type of donor bone, to fill in bony defects as she performs a spinal surgery procedure. She extracts the autograft from the patient’s own bone, taken from the same surgical incision. Coding Tips: Code 20936 is an add on code describing grafting from a donor area using the same incision during a major operative procedure and must be reported with an allowable primary spinal procedure code. You should never append modifier 50, Bilateral procedure, to 20936. The CMS Physician Fee Schedule Database includes a 9 indictor in the BILAT SURG column for this code. According to further CMS instructions, a 9 indicator in this column means that the concept of a bilateral surgery with spinal grafting does not apply. +20937 Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial incision) (List separately in addition to code for primary procedure) Notes: (Use 20937 in conjunction with 22319, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) The provider uses an autograft, a type of donor bone, to fill in bony defects as she performs a spinal surgery procedure. She extracts the autograft from the patient’s own body during the surgical procedure, through a separate incision. Coding Tips: Code 20937 is an add on code describing preparation and application of a morselized autograft through a separate skin incision and must be reported with an allowable primary spinal procedure code. *** A vertebral segment describes the basic constituent part into which the spine may be divided. It represents a single complete vertebral bone with its associated articular processes and laminae. A vertebral interspace is the non-bony compartment between two adjacent vertebral bodies which contains the intervertebral disc, and includes the nucleus pulposus, annulus fibrosus, and two cartilaginous endplates. Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate skin or fascial incision) (List separately in addition to code for primary procedure) Notes: (Use 20938 in conjunction with 22319, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) (For aspiration of bone marrow for bone grafting, spine surgery only, use 20939) The provider uses an autograft, a type of donor bone, to fill in bony defects as she performs a spinal surgery procedure. She extracts the autograft from the patient's own body during the surgical procedure, through a separate incision. Reporting Cosurgeries Source: CPT® Assistant July 1996 page 7 Coding Tip Reporting Cosurgeries "We receive many questions concerning how to report surgeries performed by more than one physician. To help you understand the proper coding we present the following information." The General Question "I am a general surgeon who sometimes performs surgeries with other surgeons (cosurgeries), such as orthopedic or neurosurgeons. I open the surgical site, the other surgeon does the definitive portion of the procedure, and then I close. What CPT codes should I report for my services? I have heard from some sources that I should bill for a thoracotomy and wound repair. But other sources have told me to report the same CPT codes as the other surgeon. Which is correct? CPT® ASSISTANT'S REPLY: Here's How to Code: "For situations in which one surgeon performs the opening and closing of a surgery and another physician performs the definitive portion of the procedure, both physicians should report the same CPT codes, and appropriately append either modifier -62 or modifier -66." Illustration A patient's surgery includes arthrodesis of two interspaces of the thoracic spine by anterior interbody technique, with anterior instrumentation of three vertebral segments. Physician "A" performs a thoracotomy at the start of the surgical session, and Physician "B" performs the arthrodesis and spinal instrumentation. Upon completion of the arthrodesis and spinal instrumentation, Physician A closes the operative site. Coding the Illustration (The physicians in the illustration would report the codes indicated below.) Physician A 22556-62 Physician B 22556-62 22558-62 22558-62 22845-62 22845-62 When performing these cosurgeries, it is important to communicate with the other surgeon's office to be certain that you submit the claims properly 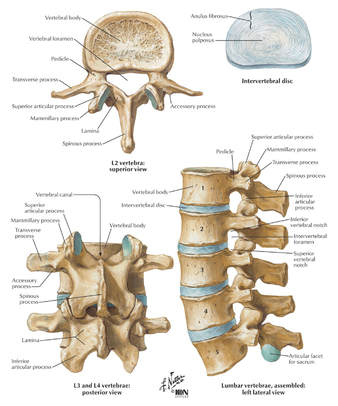 CPT® Guideline September 1997 page 8 Coding Communication How to Code Prosthetic Devices It is not often that we devote an entire article to a single code, but sometimes this is the only way to fully explain the use of certain codes-22851, application of prosthetic device (eg, metal cages, methylmethacrylate) to vertebral defect or interspace, is such a code. But before we review how to report this code, it is probably a good idea to first do a brief anatomical review of the vertebral column. The vertebral column (spine) consists of a series of bones known as vertebrae. An adult human possesses 33 vertebrae divided into the following five types: 7 cervical vertebrae; 12 thoracic vertebrae; 5 lumbar vertebrae; 5 sacral vertebrae; and 4 coccygeal vertebrae. The sacral vertebrae are typically fused into a single bone known as the sacrum. The coccygeal vertebrae are sometimes fused into a single bone known as the coccyx. Therefore, the actual number of bones in the vertebral column may be 26-29, depending on if the coccygeal vertebrae are fused. Vertebrae are commonly named by a letter that corresponds to the region of the vertebral column to which the vertebrae belongs, followed by a number that indicates where in the region the vertebrae is located. For example, the most superior cervical vertebra is called C1, with the next cervical vertebrae down designated C2. The most superior thoracic vertebrae is T1, with the next one down designated T2. Fig. 1 - Spinal Prosthetic Devices Between each pair of vertebrae is a disc that cushions the spinal column. If one of the discs degenerates or if one of the 26-29 vertebrae are injured (as in the case of a fracture, degenerative disease, or secondary to tumor destruction) the physician may need to place a prosthetic device (eg, metal cages or methyl-methacrylate) in the vertebral defect or interspace. (Fig. 1) In these instances, a segment of vertebral level may be drilled and metal cages packed with porous implants of bone graft may be inserted or methylmethacrylate may be placed between the affected vertebrae. Proper Reporting of code 22851 It is important to note that CPT® code 22851 is not intended to be reported per cage. CPT® code 22851 should only be reported one time, regardless if one or more metal cages are placed in the intervertebral space at the same level. However, if metal cages are placed at two different levels, (eg, metal cage placed at L3-4 interspace and L5-S1 interspace), then 22851 may be reported more than once to indicate that one or more cages were placed at two or more different levels. It is important to note that a single cage or methylmethacrylate can cover a defect of several vertebral segments (eg, a single cage may replace three entire vertebrae), wherein code 22851 would still only be reported one time. Within the spine section, instrumentation procedure codes (22840-22855) are reported in addition to the definitive procedure(s) without appending the modifier -51. Therefore, if arthrodesis is performed in addition to the placement of the metal cages, then it would be appropriate to report code 22851 in addition to the appropriate arthrodesis code, 22548-22632. In this instance, the modifier -51 would not be appended to code 22851. If metal cages are placed through an anterior approach and pedicle screws are placed through a posterior approach, it would be appropriate to report both code 22851 and one of the codes from the posterior instrumentation series, 22840, 22842-22844. However, if different instrumentation is used in addition to the metal cages or methylmethacrylate through the same approach (eg, an anterior plating system) or pedicle screws and posterior lumbar interbody fusion utilizing cages), then the appropriate instrumentation code would be reported in addition to code 22851. However, 22851 and 22845 should not both be reported if only the metal cage is inserted. If fracture treatment, dislocation, or arthrodesis is performed in addition to spinal instrumentation, then the appropriate fracture treatment, dislocation or arthrodesis code (22325, 22326, 22327, 22548-22812) would be reported separately in addition to code 22851. In this instance, CPT® code 22851 would be reported in addition to the definitive procedure(s) without the modifier -51 appended. If bone grafting is performed in addition to code 22851, then the appropriate bone grafting code, 20930-20938, would be reported additionally. Clinical Sample: CPT® Code 22851 A 50-year-old man undergoes an anterior fusion of L5-S1 for degenerative disease. A retroperitoneal incision is made and an arthrodesis performed using a BAK cage. A distracter is placed in the interspace, a hole is drilled in the interspace, and the BAK cage is placed in the hole. The spacer is removed and replaced with another BAK cage. Both cages are filled with bone graft. (Report arthrodesis and/or bone grafting separately using the appropriate CPT code[s]). The exposed disk space and adjacent vertebrae are prepared with bone-cutting instruments for acceptance of the prosthetic device. Preparation of the recipient site is made according to the protocol of the particular device. If methylmethacrylate is to be used, a screw or pin may be inserted into the adjacent vertebral surfaces to anchor the methylmethacrylate. Provision is made for cooling of adjacent tissues and protection of heat sensitive tissue from the exothermic reaction of the curing of the methylmethacrylate. For cages, the recipient site is prepared by bone dissection, a trial fit with the device or a spacer or template as indicated by the protocol is inserted and removed for any final modifications of the recipient site. The prosthetic device is then screwed, impacted, or injected into place according to protocol for this particular device. (Additional fixation, other provision for arthrodesis, or bone grafting are coordinated with the placement of the prosthetic device and are coded separately.) For devices that incorporate graft material, that material is appropriately placed into the device prior to its final insertion. CPT® ASSISTANT September 2000 page 10 Coding Consultation Musculoskeletal System, Surgery, 22548-22585, 22899 (Q&A) Question "Should I use the anterior or anterolateral approach technique arthrodesis series of codes (22548-22585) to report intra-abdominal laparoscopic, video assisted anterior interbody fusion?" AMA CPT® Comment "The anterior or anterolateral approach technique arthrodesis series of codes (22548-22585) are intended to describe arthrodesis performed via an open surgical approach. There is not a specific CPT code that accurately describes laparoscopic anterior interbody fusion. Therefore, code 22899, Unlisted procedure, spine should be reported. When reporting an unlisted code to describe a procedure or service, it will be necessary to submit supporting documentation (eg, procedure report) along with the claim to provide an adequate description of the nature, extent, need for the procedure, and the time limit, effort, and equipment necessary to provide the service." CPT® ASSISTANT March 2015 page 9 Frequently Asked Questions:Surgery: Musculoskeletal System Question: "Are CPT codes 22851 and 22845 appropriate to report when modular implants, such as the RSB (RSB LLC; Cleveland, OH) InterPlate® (a modular interbody platform technology), are implanted for spinal fusion procedures?" Answer: "No. The RSB InterPlate® describes a stand-alone interbody fusion device that consists of an interbody spacer with screw fixation or other mechanisms, which engage adjacent vertebrae. Such devices should be reported with code 22558, Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace (other than for decompression); lumbar, and 22851, Application of intervertebral biomechanical device(s) (eg, synthetic cage(s), methylmethacrylate) to vertebral defect or interspace (List separately in addition to code for primary procedure). An additional anterior instrumentation code (22845) is not applicable because there is no separate construct placed across the vertebral segment." Question: "Would it be appropriate to separately report any of the following with the hammertoe correction code 28285 (2nd digit), if adequately documented? (1) Resection of hypertrophied base of proximal phalanx (28126), if performed through a separate incision at the metatarsophalangeal (MTP joint); (2) flexor tenotomy (28232) performed through a separate incision at the distal interphalangeal (DIP) joint; (3) an additional unit of 28285 if K-wire is inserted through the DIP, MTP, or proximal interphalangeal (PIP) joint." Answer: "No. Code 28126, Resection, partial or complete, phalangeal base, each toe; code 28232, Tenotomy, open, tendon flexor; toe, single tendon (separate procedure); and the insertion of K-wire through DIP, PIP, and MTP joints are all inclusive components of the procedure described by code 28285, Correction, hammertoe (eg, interphalangeal fusion, partial or total phalangectomy), and should not be reported separately." References: 2020 AMA's CPT® Guidelines 2019 AMA's CPT® Guidelines 2018 AMA's CPT® Guidelines 2017 AMA's CPT® Guidelines CPT® Assistant Archives Websites: NASS Spine-Health Medtronic Ahima AAPC CMS All other commercial payers clinical guidelines from the public domains on the internet Read more blog posts:Why the CPT UNLISTED CODES IMPORTANT? Here are our Unlisted Service or Procedure Codes A service encounter or surgical procedure may be provided that is not listed in this edition of the CPT code book. When reporting such a encounter or service, the appropriate “Unlisted Procedure” code may be used to indicate the service, identifying it by “Special Report” as discussed in the section below. The “Unlisted Procedures” and accompanying codes for Surgery are as follows: 15999 Unlisted procedure, excision pressure ulcer 17999 Unlisted procedure, skin, mucous membrane and subcutaneous tissue 19499 Unlisted procedure, breast 20999 Unlisted procedure, musculoskeletal system, general 21089 Unlisted maxillofacial prosthetic procedure 21299 Unlisted craniofacial and maxillofacial procedure 21499 Unlisted musculoskeletal procedure, head 21899 Unlisted procedure, neck or thorax 22899 Unlisted procedure, spine 22999 Unlisted procedure, abdomen, musculoskeletal system 23929 Unlisted procedure, shoulder 24999 Unlisted procedure, humerus or elbow 25999 Unlisted procedure, forearm or wrist 26989 Unlisted procedure, hands or fingers 27299 Unlisted procedure, pelvis or hip joint 27599 Unlisted procedure, femur or knee 27899 Unlisted procedure, leg or ankle 28899 Unlisted procedure, foot or toes 29799 Unlisted procedure, casting or strapping 29999 Unlisted procedure, arthroscopy 30999 Unlisted procedure, nose 31299 Unlisted procedure, accessory sinuses 31599 Unlisted procedure, larynx 31899 Unlisted procedure, trachea, bronchi 32999 Unlisted procedure, lungs and pleura 33999 Unlisted procedure, cardiac surgery 36299 Unlisted procedure, vascular injection 37501 Unlisted vascular endoscopy procedure 37799 Unlisted procedure, vascular surgery 38129 Unlisted laparoscopy procedure, spleen 38589 Unlisted laparoscopy procedure, lymphatic system 38999 Unlisted procedure, hemic or lymphatic system 39499 Unlisted procedure, mediastinum 39599 Unlisted procedure, diaphragm 40799 Unlisted procedure, lips 40899 Unlisted procedure, vestibule of mouth 41599 Unlisted procedure, tongue, floor of mouth 41899 Unlisted procedure, dentoalveolar structures 42299 Unlisted procedure, palate, uvula 42699 Unlisted procedure, salivary glands or ducts 42999 Unlisted procedure, pharynx, adenoids, or tonsils 43289 Unlisted laparoscopy procedure, esophagus 43499 Unlisted procedure, esophagus 43659 Unlisted laparoscopy procedure, stomach 43999 Unlisted procedure, stomach 44238 Unlisted laparoscopy procedure, intestine (except rectum) 44799 Unlisted procedure, intestine 44899 Unlisted procedure, Meckel’s diverticulum and the mesentery 44979 Unlisted laparoscopy procedure, appendix 45399 Unlisted procedure, colon 45499 Unlisted laparoscopy procedure, rectum 45999 Unlisted procedure, rectum 46999 Unlisted procedure, anus 47379 Unlisted laparoscopic procedure, liver 47399 Unlisted procedure, liver 47579 Unlisted laparoscopy procedure, biliary tract 47999 Unlisted procedure, biliary tract 48999 Unlisted procedure, pancreas 49329 Unlisted laparoscopy procedure, abdomen, peritoneum and omentum 49659 Unlisted laparoscopy procedure, hernioplasty, herniorrhaphy, herniotomy 49999 Unlisted procedure, abdomen, peritoneum and omentum 50549 Unlisted laparoscopy procedure, renal 50949 Unlisted laparoscopy procedure, ureter 51999 Unlisted laparoscopy procedure, bladder 53899 Unlisted procedure, urinary system 54699 Unlisted laparoscopy procedure, testis 55559 Unlisted laparoscopy procedure, spermatic cord 55899 Unlisted procedure, male genital system 58578 Unlisted laparoscopy procedure, uterus 58579 Unlisted hysteroscopy procedure, uterus 58679 Unlisted laparoscopy procedure, oviduct, ovary 58999 Unlisted procedure, female genital system (nonobstetrical) 59897 Unlisted fetal invasive procedure, including ultrasound guidance, when performed 59898 Unlisted laparoscopy procedure, maternity care and delivery 59899 Unlisted procedure, maternity care and delivery 60659 Unlisted laparoscopy procedure, endocrine system 60699 Unlisted procedure, endocrine system 64999 Unlisted procedure, nervous system 66999 Unlisted procedure, anterior segment of eye 67299 Unlisted procedure, posterior segment 67399 Unlisted procedure, ocular muscle 67599 Unlisted procedure, orbit 67999 Unlisted procedure, eyelids 68399 Unlisted procedure, conjunctiva 68899 Unlisted procedure, lacrimal system 69399 Unlisted procedure, external ear 69799 Unlisted procedure, middle ear 69949 Unlisted procedure, inner ear 69979 Unlisted procedure, temporal bone, middle fossa approach When you bill for unlisted code, I always recommend to submit medical documentation. Most of the payers may require additional information. So make sure you submit your documentation and operative report as well. This way, we can avoid payment delays.
|

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985

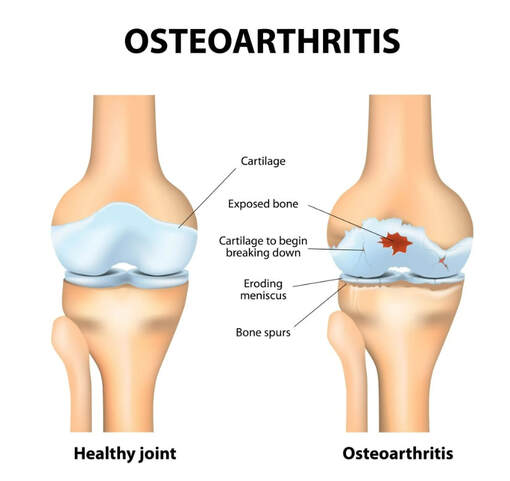

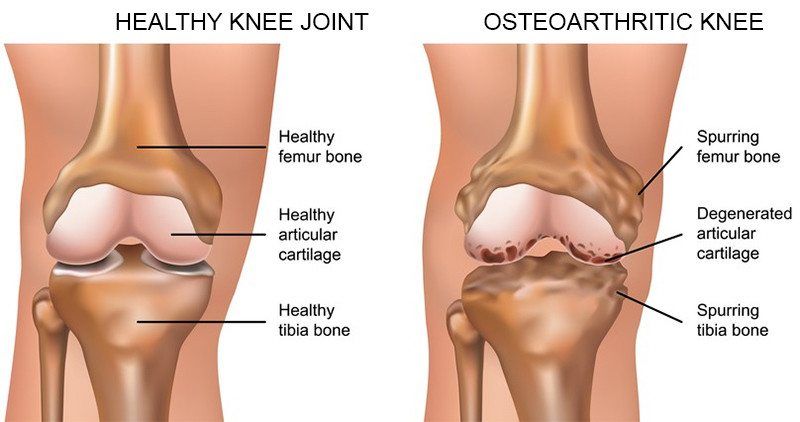



 RSS Feed
RSS Feed