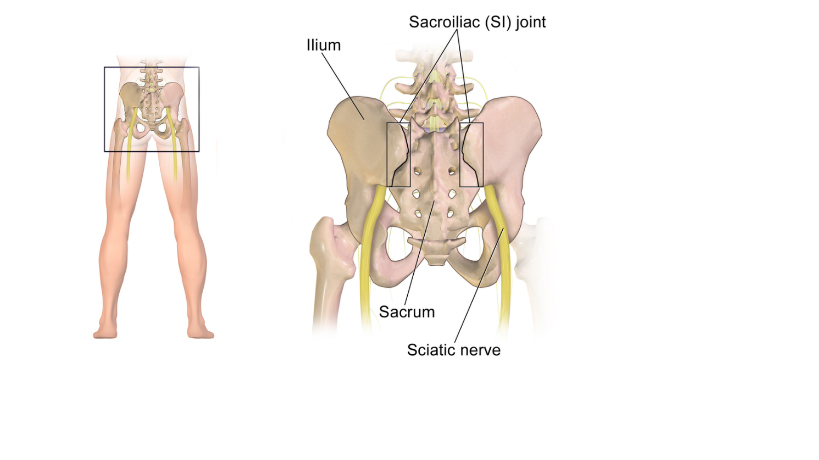
When your Pain Physician performed a Peripheral Nerve Blocks (unilateral) at the Dorsal Ramus Nerve levels L5, S1, S2 and S3, we would always look on CPT Codes 64450 (Injection, anesthetic agent; other peripheral nerve or branch) for the S1, S2 and S3. Here's the good news! Effective January 1, 2020, we now have a more specific code instead of using the "other peripheral" nerve block. Our 2020 Pain Management New Code is:
64451, Injection(s), anesthetic agent(s) and/or steroid; nerves innervating the sacroiliac joint, with image guidance (ie, fluoroscopy or CT computed tomography), should be reported once for this procedure. The fluoroscopic guidance should not be separately reported as it is included in the work described with code 64451.
0 Comments
Here are the 7 Common Reasons that I know make sense why many physicians cannot make more money! 1. Reimbursements are NOT being Maximized due to Poor Medical Coding Knowledge, Skill and Analysis Let me show you some example: a. Bilateral Procedure billed anatomically at only "one side" b. Surgery Converted to Open Procedure (the OP report documents from "Lap" to "Open" was performed) - how will you bill and code for this encounter? You may not know this, you cannot bill for both lap and open (check your CCI Edits!) together. And the guideline says, you have to report "Open" on your claim upon submission. c. Unbundling/bundling services that are billable based on the "Edits" and medical necessity d. No knowledge on how to utilize and use Modifiers e. Too naive that payments processed at 100% of the charged amount ("allowed amount") is NOT GOOD! - it would've allowed more! 2. Out of Network Physician Services Payments can be a Big Challenge! Non-contracted physicians can be very challenging. Especially when they send the payments directly to their member / the patient! Any one experienced this? That's why it is very important that you "Accept Assignment" and make your patient sign a re-assignment of benefits so you get paid directly by the insurance company! 3. Lack of Effective Collection Techniques and Staff Traininga. Copay is always due at the time of service - do many physicians do collect copay upfront? b. How often are patient statements being sent out? c. ... there's a lot more to site! 4. Now, isn't it Time to Negotiate Fees and Update the Fee Schedule?When was the last time or have you ever thought of renegotiating your contracted fees? Wouldn't it be time to analyze and review your contracts? Maybe its time to renegotiate your fees. 5. Missing "Revenue-Making" Opportunity for Additional Services in the PracticeOne good example, they know they can make big profit-margin on medically coded LSO Back Braces. And yet, they hesitate to even look at it. The truth is, it is always based on Medical Necessity! and Real-Time-Accurate Documentation, Period. You have to know your guidelines, policies and limitations. They are all out there, well documented. For instance, as a Physician, you are exempted to the Accreditation Process and Surety Bond - as long as you ONLY provide the LSO braces to your own patients as part of your services. 6. Low Productivity is also one of the Reasons! a. Physician Services b. Accounts Receivables Collection 7. Too Much Cost Running the Practice a. Staffing b. Technology c. Supplies d. Lease There you go the 7 reasons I think why Physicians can not make more money! And there is only one recommendation I can give to every physician out there - become a Leader. Build a team within your practice rather than employee and managers. Provide training and education to everyone including your self. Here are my 3 Useful Tips (and so easy to implement in your office): 1. Always check and verify patient's insurance benefits and eligibility (imperative!) 2. Always know your payers' clinical and reimbursement guidelines, policies and limitations (do your best!) 3. Hire the most qualified and experienced billing and coding staff or choose the right billing service company that are experienced based on your specialty. (very important to consider!) Be open to every possibility and strategic planning that you can definitely run a profitable practice while focusing on delivering high quality patient care.I hope you found value in this article. Your comment will be highly appreciated. Is your practice STRUGGLING?! |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985




 RSS Feed
RSS Feed