|
Understanding Telemedicine:
Telemedicine is the delivery of medical healthcare services using HIPAA-compliant and secure electronic communications, information technology, or other electronic or technological means to bridge the gap between a health care provider who is located at a distant site and a patient who is located at an originating site, either with or without the assistance of an intervening health care provider for the purpose of diagnosis, consultation, and/or treatment of a patient. We need to understand though that Telemedicine does not include the use:
What a "Distant site" means - it is a site which the health care provider, working within their scope of practice and a valid license or certification, is located while providing health care services by means of HIPAA-compliant telemedicine technology. What an "Originating site" means - it is a site at which a patient is located at the time that health care services are provided to the patient by means of telemedicine. Synchronous means live (real-time live), two-way interaction between a person and a provider using audio-visual telecommunications technology. Asynchronous also known as “store and forward” or “non-interactive telecommunication” means the acquisition and transmission of images, diagnostics, data, and medical information either to, or from, and originating site or to, or from, the healthcare provider at a distant site which allows for the patient to be evaluated without being physically present. What are the covered services in Telemedicine? Well it depends on your insurance payers. But you can find Medicare's guidelines here, CLICK HERE. Other Payers?, you can scroll down as I have added several payers. Common Modifiers used for Telehealth ServicesModifier 95 Synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system. Please refer to Appendix P within the American Medical Association’s Current Procedural Terminology (CPT®) code manual to review the CPT codes for which a "95" modifier can be used to indicate that the service was provided via a real-time, interactive audio and video telecommunications system. Modifier GT Via interactive audio and video telecommunications systems Modifier GQ Services provided via asynchronous ** always check with your payers if the above Modifiers are acceptable based on their policy. Place of Service code use 02 *** check with your payers if POS 02 is applicable for telemedicine services based on their policy Commercial and Private Payers Policy Blue Cross Blue Shield of New Jersey - Telemedicine Services
The following lists of codes is provided as an informational tool only, to help identify some of the applicable CPT® codes/code ranges and HCPCS codes that may be utilized in reporting telemedicine services. The inclusion of a specific code does not indicate eligibility for coverage in all situations. CPT Codes 90785, 90863, 96116, 90791-90792, 90832-90838, 90839-90840, 90845-90847, 90951-90961, 90963-90966, 90967-90970, 96150-96154, 96160-96161, 97802-97804, 99201-99205, 99211-99215, 99231-99233, 99241-99245, 99251-99255, 99307-99310, 99354-99357, 99406-99407, 99408-99409, 99495-99496, 99497-99498 HCPCS Codes G0108-G0109, G0270, G0296, G0396-G0397, G0406, G0407, G0408, G0420-G0421, G0425-G0427, G0438-G0439, G0459, G0473, G0506, G0508-G0509, G0513-G0514, S0199 The following services are not eligible for reimbursement under this policy:
0 Comments
Medicare's Telehealth and Telemedicine Services during Covid-19. Understanding Provider and Non-Provider Services. Understanding “EXPANSION OF TELEHEALTH WITH 1135 WAIVER” So, under this Waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patient’s places of residence starting March 6, 2020 (date of service). Due to the Coronavirus (COVID-19) Public Health Emergency, doctors and other health care providers can use telehealth services to treat COVID-19 (and for other medically reasonable purposes) from offices, hospitals, and places of residence (like homes, nursing homes, and assisted living facilities) as of March 6, 2020. Medicare will pay for these services for patients who have seen the health care provider or another health care provider in the same practice. These visits are considered as in-person visits and are paid at the rate as regular, in person visits. Starting services rendered on March 6, 2020 and for the duration of the Covid-19 Public Health Emergency, Medicare will make payment for Telehealth Medicine Professional services rendered to Medicare beneficiaries in:
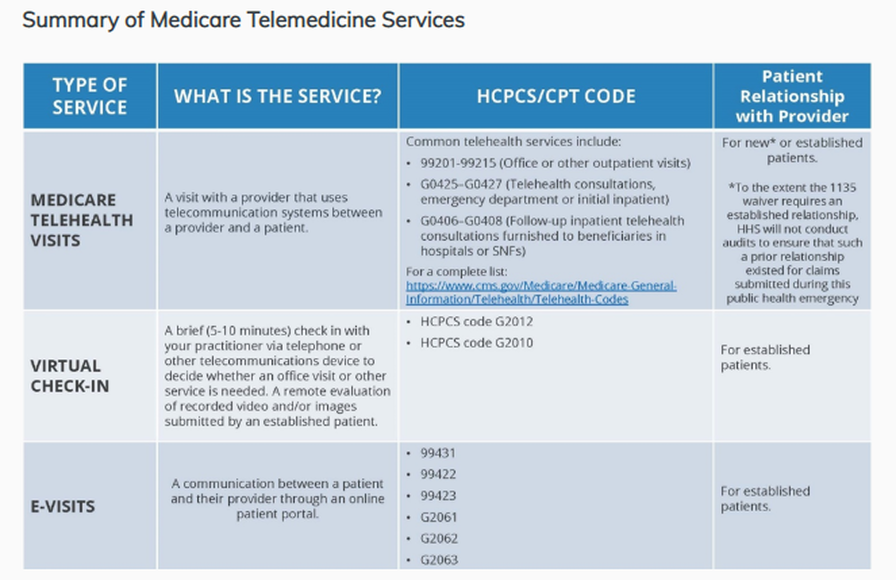
Deductible and Coinsurance will normally apply to these services. But the HHS Office of the Inspector General or the OIG is providing flexibility for healthcare Providers to reduce or waive cost-sharing for telehealth visits paid by the federal healthcare programs. It is imperative during this public health emergency that patients avoid / should not travel, when possible, to physicians’ offices, clinics, hospitals, or other health care facilities where they could risk their own or others’ exposure to further illness. Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act. Prior to this Waiver: Medicare could only pay for telehealth on a limited basis: that is; when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the service. Changes in last year (2019), Medicare started reimbursing for brief communications or Virtual Check-Ins, which are short patient-initiated communications with a healthcare practitioner. Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal as well. Effective date of service March 6, 2020: Providers can provide and render Telehealth Medicine including Evaluation and Management visits (E/M common office visits), Mental Health Counseling and Preventive Health Screenings. This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, are able to visit with their doctor from their home, without having to go to the doctor’s office or hospital which puts themselves and others at risk for Covid-19. Medicare will make payment for professional services furnished to beneficiaries in all areas of the country in all settings. While they must generally travel to or be located in certain types of originating sites such as a physician’s office, skilled nursing facility or hospital for the visit, effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Since the 1135 Waiver requires an established relationship, HHS however will not conduct an audit for all claims submitted during this public health emergency. Question: Will I get Paid? as a Provider? Answer: YES based on MEDICAL NECESSITY! We have 3 types of VIRTUAL SERVICES:
Telehealth Visits: What’s required? The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home. Distant site practitioners and clinicians who can furnish and get reimbursement for covered telehealth services is subject to State Law. REMEMBER! - report using PLACE OF SERVICE is 02 Let’s identify the Providers Billable Services: 3 types of VIRTUAL SERVICES:
Telehealth Visits: What’s required? The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home. Distant site practitioners and clinicians who can furnish and get reimbursement for covered telehealth services (check your State Law as this is subject to State Law) may include the following:
Covered Telehealth Services CY 2020 (Updated 11/01/19) Source: https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes Virtual Check-ins visits may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. Virtual Check-ins visits: Virtual check-ins can be used for the treatment for the Coronavirus (COVID-19) from anywhere, including places of residence (like homes, nursing homes, and assisted living facilities). Virtual check-in services will be initiated by the patient; however, practitioners may need to educate beneficiaries on the availability of the service prior to patient initiation. Must render only to established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. Services render via:
Here are your billable codes for Virtual Check-ins visits are as follows: HCPCS code G2012 Brief communication technology-based service, e.g. virtual check-in, by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an e/m service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion. Requirements:
*** As being recommended by CMS to use G2012 for telehealth services. More information, click here. HCPCS code G2010 Remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M Evaluation and Management service provided within the previous 7 days nor leading to an e/m service or procedure within the next 24 hours or soonest available appointment. Virtual check-ins can be conducted with a broader range of communication methods, unlike Medicare Telehealth or Telemedicine visits, which require audio and visual capabilities for real-time communication. e-visits services are only rendered via an online patient portal. e-VISITS Services: E-visits services are only rendered via an online patient portal. These services can only be reported when the billing practice has an established relationship with the patient. This is not limited to only rural settings. There are no geographic or location restrictions for these visits. Practitioners who may furnish these services include:
Your Billable Codes for e-visits are as follows: CPT 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes CPT 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11– 20 minutes CPT 99423: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes. Clinicians who may not independently bill for evaluation and management visits . For example are:
They can also provide these e-visits and bill using the following codes: HCPCS Code G2061: Qualified non-physician healthcare professional online assessment and management, for an established patient, for up to seven days, cumulative time during the 7 days; 5–10 minutes HCPCS Code G2062: Qualified non-physician healthcare professional online assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 11–20 minutes HCPCS Code G2063: Qualified non-physician qualified healthcare professional assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 21 or more minutes. For more information: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/index.html For Medicare Beneficiaries, you can learn more about telehealth services here - https://www.medicare.gov/coverage/telehealth HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT (HIPAA): Effective immediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency. For more information: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/index.html HEADS-UP! - Use of GT modifier on Medicare claims was eliminated in 2018. According to CMS, the place of service code 02 is sufficient. To read more on Medicare Payment for Telemedicine. - CLICK HERE Medicare Claims Processing Manual Chapter 12 - Physicians/Nonphysician Practitioners 190 - Medicare Payment for Telehealth Services 190.1 - Background 190.2 - Eligibility Criteria 190.3 - List of Medicare Telehealth Services 190.3.1 - Telehealth Consultation Services, Emergency Department or Initial Inpatient versus Inpatient Evaluation and Management (E/M) Visits 190.3.2 - Telehealth Consultation Services, Emergency Department or Initial Inpatient Defined 190.3.3 - Follow-Up Inpatient Telehealth Consultations Defined 190.3.4 – Payment for ESRD-Related Services as a Telehealth Service 190.3.5 – Payment for Subsequent Hospital Care Services and Subsequent Nursing Facility Care Services as Telehealth Services 190.3.6 – Payment for Diabetes Self-Management Training (DSMT) as a Telehealth Service 190.3.7 – Payment for Telehealth for Individuals with Acute Stroke 190.4 - Conditions of Payment 190.5 - Originating Site Facility Fee Payment Methodology 190.6 - Payment Methodology for Physician/Practitioner at the Distant Site 190.6.1 - Submission of Telehealth Claims for Distant Site Practitioners 190.6.2 - Exception for Store and Forward (Non-Interactive) Telehealth 190.7 - A/B MAC (B) Editing of Telehealth Claims Timeline and Important Links: (source: CMS.GOV) For more information on telehealth benefits in the Medicare program, read the fact sheet: https://www.cms.gov/files/document/03052020-medicare-covid-19-fact-sheet.pdf.
Summary of CMS Public Health Action on COVID-19 to date: March 6, 2020, CMS issued frequently asked questions and answers (FAQs) for healthcare providers regarding Medicare payment for laboratory test and other services related to the 2019-Novel Coronavirus (COVID-19). https://www.cms.gov/newsroom/press-releases/covid-19-response-news-alert-cms-issues-frequently-asked-questions-assist-medicare-providers March 5, 2020: CMS issued a second Healthcare Common Procedure Coding System (HCPCS) code for certain COVID-19 laboratory tests, in addition to three fact sheets about coverage and benefits for medical services related to COVID-19 for CMS programs. https://www.cms.gov/newsroom/press-releases/cms-develops-additional-code-coronavirus-lab-tests March 4, 2020: CMS issued a call to action to healthcare providers nationwide and offered important guidance to help State Survey Agencies and Accrediting Organizations prioritize their inspections of healthcare. https://www.cms.gov/newsroom/press-releases/cms-announces-actions-address-spread-coronavirus February 13, 2020: CMS issued a new HCPCS code for providers and laboratories to test patients for COVID-19. https://www.cms.gov/newsroom/press-releases/public-health-news-alert-cms-develops-new-code-coronavirus-lab-test February 6, 2020: CMS gave CLIA-certified laboratories information about how they can test for SARS-CoV-2. https://www.cms.gov/medicareprovider-enrollment-and-certificationsurveycertificationgeninfopolicy-and-memos-states-and/notification-surveyors-authorization-emergency-use-cdc-2019-novel-coronavirus-2019-ncov-real-time-rt February 6, 2020: CMS issued a memo to help the nation’s healthcare facilities take critical steps to prepare for COVID-19. https://www.cms.gov/medicareprovider-enrollment-and-certificationsurveycertificationgeninfopolicy-and-memos-states-and/information-healthcare-facilities-concerning-2019-novel-coronavirus-illness-2019-ncov For the updated information on the range of CMS activities to address COVID-19, visit: https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Current-Emergencies-page How are the Commercial Payers' Policy on Telehealth during this trying time due to Covid-19? A3843 Requires health insurance and Medicaid coverage for testing of coronavirus disease 2019 and for telemedicine and telehealth during coronavirus disease 2019 state of emergency. - NJ State New York State Medicaid Coverage and Reimbursement Policy for Services Related to TRICARE covers the use of interactive audio/video technology services, and are subject to the same referral and authorization requirements and include, but are not limited to: clinical consultations, office visits and telemental health. CLICK HERE for more details. Telehealth visits: what’s required? The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home. Distant site practitioners and clinicians who can furnish and get reimbursement for covered telehealth services (check your State Law as this is subject to State Law) may include the following:
Medicare Covered Telehealth Services CY 2020 (Updated 11/01/19) Code Short Descriptor
90785 Psytx complex interactive 90791 Psych diagnostic evaluation 90792 Psych diag eval w/med srvcs 90832 Psytx pt&/family 30 minutes 90833 Psytx pt&/fam w/e&m 30 min 90834 Psytx pt&/family 45 minutes 90836 Psytx pt&/fam w/e&m 45 min 90837 Psytx pt&/family 60 minutes 90838 Psytx pt&/fam w/e&m 60 min 90839 Psytx crisis initial 60 min 90840 Psytx crisis ea addl 30 min 90845 Psychoanalysis 90846 Family psytx w/o patient 90847 Family psytx w/patient 90951 Esrd serv 4 visits p mo <2yr 90952 Esrd serv 2-3 vsts p mo <2yr 90954 Esrd serv 4 vsts p mo 2-11 90955 Esrd srv 2-3 vsts p mo 2-11 90957 Esrd srv 4 vsts p mo 12-19 90958 Esrd srv 2-3 vsts p mo 12-19 90960 Esrd srv 4 visits p mo 20+ 90961 Esrd srv 2-3 vsts p mo 20+ 90963 Esrd home pt serv p mo <2yrs 90964 Esrd home pt serv p mo 2-11 90965 Esrd home pt serv p mo 12-19 90966 Esrd home pt serv p mo 20+ 90967 Esrd home pt serv p day <2 90968 Esrd home pt serv p day 2-11 90969 Esrd home pt serv p day 12-19 90970 Esrd home pt serv p day 20+ 96116 Neurobehavioral status exam 96150 Assess hlth/behave init 96151 Assess hlth/behave subseq 96152 Intervene hlth/behave indiv 96153 Intervene hlth/behave group 96154 Interv hlth/behav fam w/pt 96160 Pt-focused hlth risk assmt 96161 Caregiver health risk assmt 97802 Medical nutrition indiv in 97803 Med nutrition indiv subseq 97804 Medical nutrition group 99201 Office/outpatient visit new 99202 Office/outpatient visit new 99203 Office/outpatient visit new 99204 Office/outpatient visit new 99205 Office/outpatient visit new 99211 Office/outpatient visit est 99212 Office/outpatient visit est 99213 Office/outpatient visit est 99214 Office/outpatient visit est 99215 Office/outpatient visit est 99231 Subsequent hospital care 99232 Subsequent hospital care 99233 Subsequent hospital care 99307 Nursing fac care subseq 99308 Nursing fac care subseq 99309 Nursing fac care subseq 99310 Nursing fac care subseq 99354 Prolonged service office 99355 Prolonged service office 99356 Prolonged service inpatient 99357 Prolonged service inpatient 99406 Behav chng smoking 3-10 min 99407 Behav chng smoking > 10 min 99495 Trans care mgmt 14 day disch 99496 Trans care mgmt 7 day disch 99497 Advncd care plan 30 min 99498 Advncd are plan addl 30 min G0108 Diab manage trn per indiv G0109 Diab manage trn ind/group G0270 Mnt subs tx for change dx G0296 Visit to determ ldct elig G0396 Alcohol/subs interv 15-30mn G0397 Alcohol/subs interv >30 min G0406 Inpt/tele follow up 15 G0407 Inpt/tele follow up 25 G0408 Inpt/tele follow up 35 G0420 Ed svc ckd ind per session G0421 Ed svc ckd grp per session G0425 Inpt/ed teleconsult30 G0426 Inpt/ed teleconsult50 G0427 Inpt/ed teleconsult70 G0436 Tobacco-use counsel 3-10 min G0437 Tobacco-use counsel>10min G0438 Ppps, initial visit G0439 Ppps, subseq visit G0442 Annual alcohol screen 15 min G0443 Brief alcohol misuse counsel G0444 Depression screen annual G0445 High inten beh couns std 30m G0446 Intens behave ther cardio dx G0447 Behavior counsel obesity 15m G0459 Telehealth inpt pharm mgmt G0506 Comp asses care plan ccm svc G0508 Crit care telehea consult 60 G0509 Crit care telehea consult 50 G0513 Prolong prev svcs, first 30m G0514 Prolong prev svcs, addl 30m G2086 Off base opioid tx first m G2087 Off base opioid tx, sub m G2088 Off opioid tx month add 30 Source: https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes When Medicare is a Primary Insurance for the patient, the patient's part responsibility (coinsurance/deductible) normally crosses over to its secondary insurance for secondary coverage (if Medicare has the secondary insurance on file or if its set up to cross over based on the patient's coordination of benefits).
As you will notice on your Remittance advise, "Claim Information forwarded to: (insurance company here) Meaning, Medicare will forward the information to the secondary insurance. If not, try to find out if there is a secondary insurance for the patient, then you need to send the paper claim (using the HCFA 1500 form for Office/Provider/Professional Claims) to the secondary and attach a copy of the Medicare EOB (explanation of benefits). If your Practice Software can bill secondary to Medicare electronically, then that's great! Send them by electronic. If your practice management software is capable of doing this by electronic submission with attached copy of the EOB - much better!After you submit the claim to the secondary insurance, the secondary insurance EOB will then tell you if there is a copay being applied towards the patient being a secondary insurance after Medicare.You will then obviously collect that copay based on your contract with the secondary insurance company (and this is also based on the patient's contract with his/her secondary insurance). Medicare patients are mostly aware of their responsibility after the secondary insurance picks up. Bottom line here: (1) Medicare must process (not deny or reject!) the claim first being the primary; (2) Secondary insurance must then process the claim with Medicare's claim information; (3) Then, if there is a copay being applied towards the patient's responsibility -- you have to bill your patient for that copay!But honestly, I do not collect secondary insurance copay not until the secondary insurance had processed the claim (after Medicare's allowance!). WHY? because it is possible that the patient may no longer have an active policy (at the time of service) with the secondary insurance, or maybe, there is no more copay because the patient had met his/her out of pocket limit. So to streamline this issue (of which not all offices are doing it) - you must always check benefits and eligibility for your patient's primary, secondary or even tertiary insurance coverage!It may be a lot of work too, but what I do is that, when I am billing the patient a copay (from the secondary insurance's determination and per the EOB) or even for their coinsurance! I do my best to attach a copy of the EOB on the statement. That way, the patient has a copy of the said EOB and he/she will understand why I am billing him/her. How do you describe CPT 99204? Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: a comprehensive examination; medical decision making of moderate complexity. Counseling and/ or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are of moderate to high severity. Typically, 45 minutes are spent face-to-face with the patient and/or family. How do you report CPT 99205? - read below. Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 components: A comprehensive history; A comprehensive examination; Medical decision making of the complexity. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family needs. Usually, the presenting problems(s) are of moderate to high severity. Typically, 60 minutes are spent face-to-face with the patient and/or family CPT 99204 and or CPT 99205 Key Points:
5 Mindful ways to Improving Patient Access Access is a significant concern in the United States and all over the world when it comes to patient care. We all know that the patients have to wait for months to get the physician they want, and a good doctor has more patients than they can manage. The patients waiting for months to get the physician surely lead to delayed treatment and also can jeopardize their health and their life. On the other hand, it will certainly reduce the patient satisfaction scores for the doctors and the medical service providers. As these scores have to be shared with third parties such as pharmaceuticals and drug companies as well as the insurance companies, managing the scores is extremely significant for the doctors. So here are a few ways that you can make sure your patients are not sitting and waiting for you to give them an appointment for half a year. Step 1: Learn how to Measure The first appointment available is a valuable commodity. So make sure that you have a good system to call people who are on the waiting list. Not just the first appointment available, but the second and third appointments available can also be prescheduled. You should inform the patients that are on the waiting list that they can be called in for a consult at short notice. When a person is coming up for the next available appointment, you can inform them that they are next on the list. That will allow individuals to prepare for showing up without feeling like it was impractical to ask on such short notice. Call people up or have a reminder system in place that will inform people on the list when they are next on the list of first appointment available. There are many openings happening every day, and placing then effectively can reduce overextended waiting lists considerably. Step 2: Denied Appointment Requests The patients who were denied an appointment is also a crucial list that needs to be monitored closely. There are many reasons that a patient is denied care, and those reasons should be listed clearly. If there is no appointment available or the appointment is not given for another reason, the reasons should be listed. That process will allow the nurses and administration to solve the problem and will allow them to develop a system that reduces denied appointments. Step 3: Implementation of the Data The main focus of all of the points mentioned above is to have a system that focuses on developing data sheets on appointment schedules so that you can decide how to have a more productive appointment culture. Here are a few steps you should take in the implementation process:
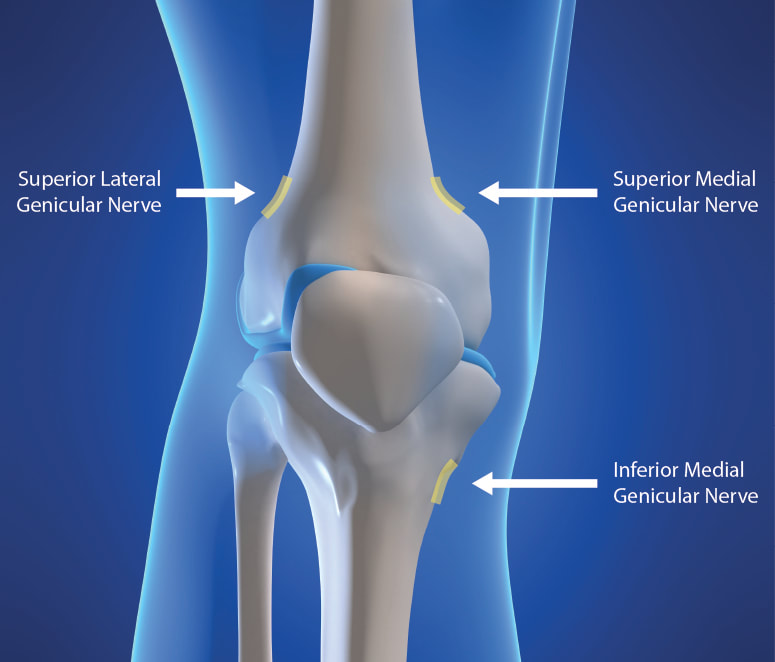
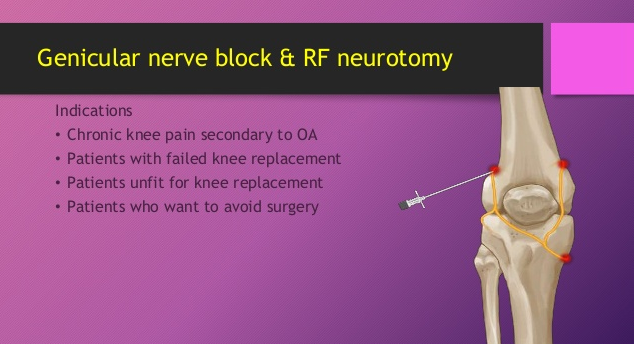
● Ask your administration about how they feel that they are being pushed too hard in the appointment process. ● Develop a severity scale of the patient’s complaint in the form of a questionnaire. The patient will answer the questionnaire on the phone, and the nurse or staff can decide how urgently they need to see the doctor. Step 4: Effective Ways to Problem Solving Find effective and simple solutions that will increase patient access on a daily basis. A few and simple tips on the matter are as follows: ● Have four backup appointments for every day that the patients have already been informed of. That way, the patient can simply come in if another patient cancels their appointment, and they will already be prepared for it. ● Patients on their second consult or with small concerns can come and see the doctor while the first patient is getting their physical. ● If there is a list of symptoms common in the specialty of the doctor, then nurses can provide that list to the administrator. If a patient complains of these symptoms, then they will be called in by the nursing staff on an urgent basis. ● Avoid letting worthy patients go to waiting lists for chronic complainers. Patients who have a tendency to over complaint can be seen and managed by the nursing staff. Step 5: Execute Now, all it is left is to reorganize these concepts and make sure that they are implemented effectively. You will see amazing results with a small number of initiatives. We are here for any ideas that you want to discuss. We are experts in the field. Share your experiences with us in the comments section, and we would love to get back to you! How to Bill for Knee Genicular Nerve Branches RFA or Ablation, Destruction Billing for the Genicular Nerve Branches RFA have been a struggle since it was not too clear to us on how we should be billing for this service. The good news is, we have a new code for this effective January 1, 2020. New CPT 2020 Changes. New Pain Management 2020 Codes. When your physician is performing an RFA on Genicular nerves, use code 64624 (Destruction by neurolytic agent of genicular nerve branches). Take note of the word "branches". These changes are explained as follows: Destruction by Neurolytic Agent (eg, Chemical, Thermal, Electrical or Radiofrequency), Chemodenervation on the Somatic Nerves CPT CODE 64624 Destruction by neurolytic agent, genicular nerve branches including imaging guidance, when performed (Do not report 64624 in conjunction with 64454 - Injection(s), anesthetic agent(s) and/or steroid; genicular nerve branches, including imaging guidance, when performed Pay attention to this, the CPT 64624 requires the destruction of each of the following genicular nerve branches: (make sure your Provider had documented this!)
If a neurolytic agent for the purposes of destruction is not applied to all of these nerve branches, you can report CPT 64624 but you MUST append the MODIFIER 52: 64624-52 What is Modifier 52? Modifier 52 is usually used for reduced services. It may occur under certain circumstances that a service or procedure is partially reduced or eliminated at the physician’s discretion. There can be several reasons behind the physician’s decision. In this situation, service provided can be identified by its usual procedure number and the addition of the modifier 52, which indicates that the service was reduced. Understanding the 3 Genicular Nerve Branches of 64624What is the CPT code for Knee Genicular Nerve Branches Block or Injection? Understanding the 3 Genicular Nerve Branches of 64454When your Physician is Blocking the Knee Genicular Nerves - here's your code: (pay attention with the imaging! it is included!). CPT 64454 - Injection(s), anesthetic agent(s) and/or steroid; genicular nerve branches; (make sure your Provider had documented this!)
If all 3 of these genicular nerve branches are not injected, report 64454 with Modifier; 64454-52 What is Modifier 52? Modifier 52 is usually used for reduced services. It may occur under certain circumstances that a service or procedure is partially reduced or eliminated at the physician’s discretion. There can be several reasons behind the physician’s decision. In this situation, service provided can be identified by its usual procedure number and the addition of the modifier 52, which indicates that the service was reduced. Article Source: CPT Assistant December 2019 page 8 Destruction by Neurolytic Agent (Genicular Injection; Radiofrequency Neurotomy Sacroiliac Joint) For Current Procedural Terminology Got additional questions or concerns? call us today! Billing Tip: Always make sure you understand and you know the Medical, Clinical, Utilization and Reimbursement Policy of your Payers. Read other blog posts: |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985





 RSS Feed
RSS Feed