UNDERSTANDING HOW TO USE MODIFIER 79  How to Use Modifier 79 How to Use Modifier 79 Per the Current Procedure Terminology® (CPT®) manual, the descriptor of modifier 79 is: • "Unrelated procedure or service by the same physician during the postoperative period." As indicated, this modifier is used to bill an unrelated procedure or service performed by the same physician during the postoperative period of a previous surgical procedure. When a patient has surgery performed, there is a postoperative period -- a period after the surgery has been performed when additional surgical care related to the initial surgery is considered already covered (and paid for) by the allowance provided for the initial surgery. The postoperative period can be zero or 10 days (minor surgical procedure) or 90 days (major surgical procedure). (Note that some surgeries are considered so minor that they have a zero day postoperative period, usually a very quick outpatient procedure.) Modifier 79 should be used when a surgical procedure is:
REMEMBER! When the 79 modifier is used, a new postoperative period for the second surgical procedure begins. Additionally, the remainder of the postoperative period of the original surgery is still applicable. References: Medicare CMS Website American Medical Association CPT Coding Books Payers Websites
0 Comments
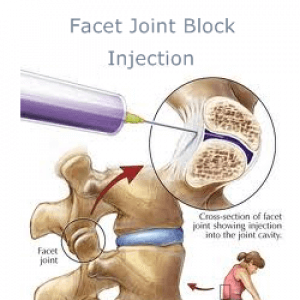
Still confused with Coding and reporting medial and lateral branch nerve blocks and understanding Pain Management procedures? Coding Billing for Medial and Lateral Nerve Blocks. According to the AMA, the code series for medial branch blocks and the facet joint injections are the same (i.e., CPT series 64490-64495), with reporting based on the number of facet joints injected, not the number of nerves injected. For example: If three (3) medial branch nerves are injected only two (2) facet joint injection codes would be reported despite the fact that three nerves were injected, since each facet joint is connected to two medial nerves. The lateral branch nerve is a peripheral nerve and would be reported with CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch, when a lateral branch nerve block is performed. Please note: CPT code 64450 should only be reported per nerve or branch and not per injection. CPT code 76942, Ultrasonic guidance for needle placement (e.g., biopsy, aspiration, injection, localization device), imaging supervision and interpretation, would be additionally reported when utilizing ultrasound guidance for certain nerve block procedures when it is not inherent in the primary procedure code. The Different kinds or types of NERVE BLOCKS and what are they targeting: NERVE BLOCKS: Brachial plexus block, elbow block, wrist block BODY AREAS: Shoulder, arm, hand, elbow, wrist) NERVE BLOCKS: Cervical epidural, thoracic epidural, lumbar epidural block BODY AREAS: Neck, back NERVE BLOCKS: Cervical plexus block, cervical paravertebral block BODY AREAS: Shoulder, upper neck NERVE BLOCKS: Maxillary nerve block BODY AREAS: Upper jaw NERVE BLOCKS: Ophthalmic nerve block BODY AREAS: Eyelids, scalp NERVE BLOCKS: Sphenopalatine nerve block BODY AREAS: Nose, palate NERVE BLOCKS: Subarachnoid block, Celiac plexus block BODY AREAS: Abdomen, pelvis NERVE BLOCKS: Supraorbital nerve block BODY AREAS: Forehead NERVE BLOCKS: Trigeminal nerve block BODY AREAS: Face CPT 64490, 64493, 64495, 64633 - Billing and Coding for Facet Nerve Block and Nerve Ablation RFA CPT CODE 64490 PARAVERTEBRAL FACET JOINT BILLING AND CODING WITH IMAGING GUIDANCEInjection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), cervical or thoracic; single level 64491 ----------- second level 64492 ----------- third and any additional level(s) level CPT CODE 64493Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), lumbar or sacral; single level 64494 ----------- second level 64495 ----------- third and any additional level(s) level FACET JOINT BILLING AND CODING WITH ULTRA-SOUND 0213T Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, cervical or thoracic; single level ....................................................................+ 0214T second level ....................................................................+ 0215T third and any additional level(s) 0216TInjection(s), diagnostic or therapeutic agent, paravertebral facet (zygapophyseal) joint (or nerves innervating that joint) with ultrasound guidance, lumbar or sacral; single level ..................................................................+ 0217T second level ..................................................................+ 0218T third and any additional level(s) Billing and Coding for Radiofrequency Facet denervationCPT CODE 64633 Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); cervical or thoracic, single facet joint' +64634 cervical or thoracic, each additional facet joint (List separately in addition to code for primary procedure) CPT CODE 64635 Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); lumbar or sacral, single facet joint; +64636 lumbar or sacral, each additional facet joint (List separately in addition to code for primary procedure) Other Searched Keywords: Billing and Coding for RFA of Facet Joint Nerves Billing and Coding for Facet Joint AblationKey Points for CPT 64490, 64493, 64495, 64633 - Billing and Coding for Facet Nerve Block and Nerve Ablation RFA These codes are unilateral
 Let's look at these questions and answers: #1 Question "What are the appropriate code assignments when a patient receives 3 separate nerve blocks into the same lateral branch nerve? Would it be appropriate to report 3 units of this service?" The right CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch, would be appropriately reported only once in this case since all 3 nerve blocks were administered to the same nerve or branch. #2 Question "We are getting conflicting information regarding coding medial and lateral branch blocks S1, S2, and S3, Medial 64493, 64494, Lateral 64493, and 64494. Our Pain Center wants to use facet injection for the medial branch block and other peripheral nerve for the lateral branch block. Are we correct in reporting lateral branch nerve block(s) to the peripheral nerve CPT code?" Yes, you are correct. The lateral branches of the dorsal sacral nerve plexus are considered peripheral nerves. Therefore, for the four lateral branch block injections at S1, S2, S3, and S4, report 4 units of CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch. Report multiple units of the injection for the four lateral branch block injections performed, modifier 59 would not be appended in this case. # 3 Question "A patient was seen at our facility and underwent a left-sided L5 and S1, S2, S3, and S4 lateral branch nerve block for diagnostic purpose with C-arm fluoroscopy. What are the correct codes for a lateral nerve block?" So OK, ... based on the operative report a medial branch nerve block was performed at the L5 and a lateral branch nerve block was performed at the S1, S2, S3 and S4 Therefore, it would be appropriate to report CPT code 64493, Injection(s), diagnostic or therapeutic agent, paravertebral facet (zygapohphyseal) joint (or nerves innervating that joint) with image guidance (fluoroscopy or CT), lumbar or sacral, single level, for the L5 medial branch block. For the 4 lateral branch block injections at S1, S2, S3, and S4, report 4 units of CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch. From AMA's CPT Assistant: February 2011 page 4 (In September 2011 questions relating to this article were discussed.) Revisions made to certain pain medicine procedures in the CPT 2011 codebook include new procedure codes, and guidelines were created in the Nervous System section to clarify the reporting of these services. The following code sets are affected: • Introduction/Injection of Anesthetic Agent (Nerve Block), Diagnostic or Therapeutic (64400-64530) • Neurostimulators (Peripheral Nerve) (64550-64595) • Destruction by Neurolytic Agent (eg, Chemical, Thermal, Electrical or Radiofrequency) (64600-64681) Introduction/Injection of Anesthetic Agent (Nerve Block), Diagnostic or Therapeutic Revised Codes The following codes were revised for 2011: 64479Injection(s), anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance (fluoroscopy or CT); cervical or thoracic, single level 64480Injection(s), anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance (fluoroscopy or CT); cervical or thoracic, each additional level (List separately in addition to code for primary procedure) 64483Injection(s), anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance (fluoroscopy or CT); lumbar or sacral, single level 64484Injection(s), anesthetic agent and/or steroid, transforaminal epidural, with imaging guidance (fluoroscopy or CT); lumbar or sacral, each additional level (List separately in addition to code for primary procedure) What exactly is "transforaminal epidural injection"? codes 64479-64484. TFE describe injections that enter the epidural space through the intervetebral foramen. This technique differs from interlaminar / translaminar epidural injection technique (62321-62327) and the paravertebral facet joint nerve injection technique (64490-64495). Since the vertebral artery (in the cervical spine), radiculomedullary arteries, as well as the spinal cord are in close proximity to the nerve root, this procedure involves a much higher risk with more work than a translaminar epidural injection. If ultrasound is used to guide the transforaminal injections, a code from the category III code set should be used instead of a code from the 64479-64484 code series. Therefore, parenthetical notes instruct users to report Category III codes 0228T, 0229T, 0230T, and 0231T for ultrasound-guided transforaminal epidural procedures. Additionally ultrasound guidance procedure code 76942, Ultrasound guidance for needle placement (eg biopsy, aspiration, injection, localization device), imaging supervision and interpretation, has been revised to clarify that it may not be used as guidance for 64479-64495 injections. Coding Tip Codes 64479-64484 are inherently unilateral procedures. When these procedures are performed bilaterally, they should be appended with modifier 50 or with a HCPCS Level II modifier "RT" or "LT" depending upon payer requirements. Paravertebral Spinal Nerves and Branches New Guidelines The paravertebral facet joint is the site of interaction between the vertebral bone above and below, and can be a source of pain. Injections can be made either into the joint, or at each of the nerves that supply the joint (ie, the medial nerve branches). To coordinate with the revision of codes 64479-64484, new parenthetical notes in the Paravertebral Spinal Nerves and Branches section of the CPT codebook direct users to the appropriate code to identify paravertebral facet joint injections when performed with imaging guidance. When performing a paravertebral facet injection into the T12-L1 joint, or at the nerves innervating that joint, code 64490 is reported. Fluoroscopy and CT imaging guidance and any injection of contrast are inclusive components of codes 64490- 64495. Imaging guidance and localization are required for the performance of paravertebral facet joint injections, as described by codes 64490-64495. If imaging guidance is not used, code 20552, Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s), or code 20553 , Injection(s); single or multiple trigger point(s), 3 or more muscle(s), should be reported instead of a code from the 64490-64495 code series. If ultrasound guidance is used, it is appropriate to report Category III codes 0213T-0218T. Coding Tip Paravertebral facet injection codes 64490-64495 and 0213T-0218T are unilateral. When performed bilaterally, they may be appended with modifier 50 or a HCPCS Level II modifier "RT" or "LT" depending on the requirements of the payer. Neurostimulators (Peripheral Nerve) New Codes Code 64573 was deleted and the following four new codes were added for 2011: 64566Posterior tibial neurostimulation, percutaneous needle electrode, single treatment, includes programming 64568Incision for implantation of cranial nerve (eg, vagus nerve) neurostimulator electrode array and pulse generator 64569Revision or replacement of cranial nerve (eg, vagus nerve) neurostimulator electrode array, including connection to existing pulse generator 64570Removal of cranial nerve (eg, vagus nerve) neurostimulator electrode array and pulse generator Code 64566 is reported for a treatment of voiding dysfunction (eg, urge incontinence), posterior tibial nerve stimulation. Code 64566 was created to describe a minimally invasive procedure that includes both the needle insertion through the skin adjacent to the tibial nerve, as well as the placement of an electrode on the surface of the skin. The treatment consists of a series of sessions involving insertions of a percutaneous needle electrode, with intermittent neuromodulation for approximately 30 minutes while the needle electrode remains in place. The neurostimulator includes a lead set with surface electrodes and a needle electrode, which produces an adjustable electrical pulse that travels to the sacral nerve plexus via the tibial nerve. The sacral nerve plexus then regulates the bladder and the pelvic floor functionality. Code 64566 would be reported once for each neurostimulation treatment session. References:
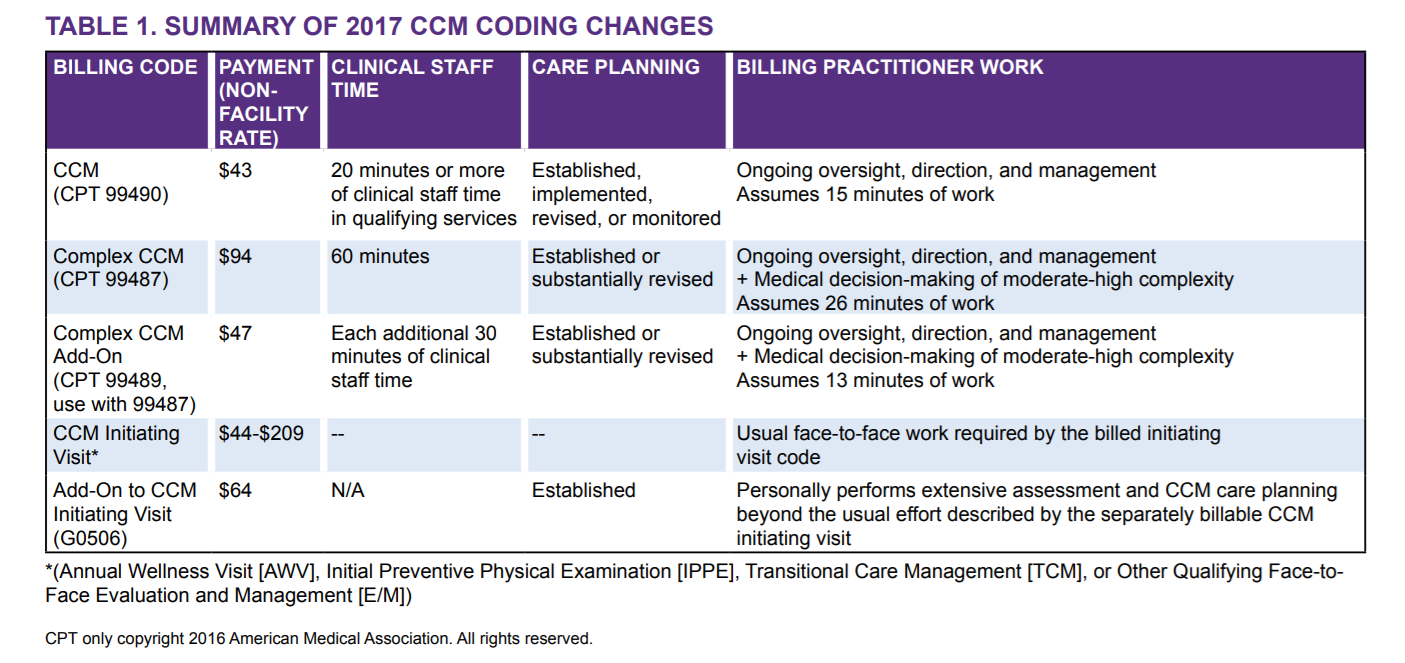
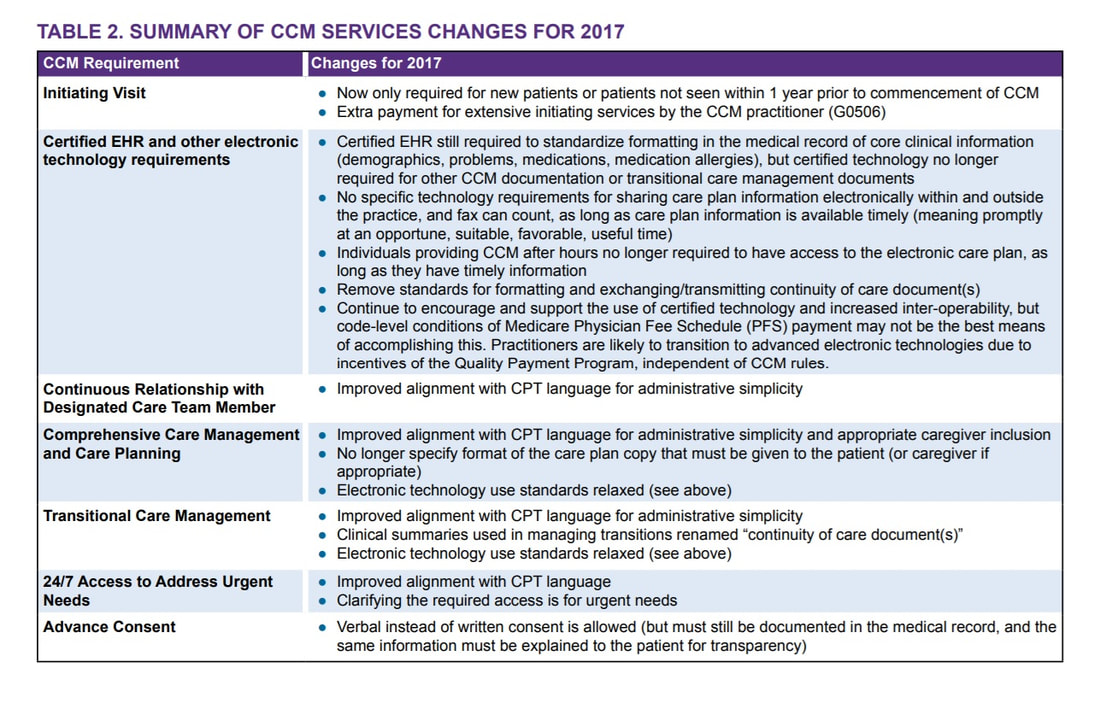
2017 / 2018 Coding Books (CPT is a Trademark and Owned by the American Medical Association) AMA's CPT Assistant Archives CMS Medicare Website (LMN, NCD/LCD, Manuals) Commercial Payers Guidelines How to Bill Chronic Care Management 99490 and Complex CCM 99487, 99489  Chronic Care Management Services and the New Changes for 2017 CMS Medicare recognizes the Chronic Care Management (CCM) as a critical component of primary care services that contributes to better health and care for individuals. So in 2015, Medicare began paying separately under the Medicare Physician Fee Schedule for CCM services furnished to Medicare patients with multiple chronic conditions. Beginning January 1, 2017, the CCM codes are: Code 99490 Chronic care management services, at least 20 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month, with the following required elements:
Keys to Remember: Let’s try to describe what CCM is or Chronic Care Management Services. These are services rendered by a Physician or Non-Physician Practitioners such as Nurse Practitioners, Physician Assistants, Clinical Nurse Specialist, Certified Nurse-Midwife and the CLINICAL Staff --- per month, for patients with two or more chronic medical conditions expected to last at least 12 months or until the death of the patient, and that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline. Take note that ONLY (1) One Practitioner can report and bill for Chronic Care Management per month. The included services are: ○ Access and use of a Certified Electronic Health Record (EHR) ○ Continuity of Care with Designated Care Team Member ○ Comprehensive Care Management and Care Planning ○ Transitional Care Management ○ Coordination with Home and Community-Based Clinical Service Providers ○ 24/7 Access to Address Urgent Needs ○ Enhanced Communication (email, and telephone for example) ○ Advance Consent CCM Changes in 2017 are the following:
There is a more complex care and we describe it as Complex Chronic Care Management services; Here are your two new codes for the Complex CCM - Complex Chronic Care Management services: CPT 99487 Complex chronic care management services, with the following required elements: ● Multiple (two or more) chronic conditions expected to last at least 12 months, or until the death of the patient; ● Chronic conditions place the patient at significant risk of death, acute exacerbation/ decompensation, or functional decline; ● Establishment or substantial revision of a comprehensive care plan ● Moderate or high complexity medical decision making ● 60 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month (Novitas Part B NJ North $102.36) CPT +99489 --- (this is an add-code and cannot be billed by itself!) Each additional 30 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month (List separately in addition to code for primary procedure) Complex CCM services of less than 60 minutes in duration, in a calendar month, are not reported separately(Novitas Part B NJ North $50.98) Supervision The CCM codes (CPT 99487, 99489, and 99490) are assigned general supervision under the Medicare PFS. General supervision means when the service is not personally performed by the billing practitioner, it is performed under his or her overall direction and control although his or her physical presence is not required. Patient Eligibility Patients with multiple (two or more) chronic conditions expected to last at least 12 months or until the death of the patient, and that place the patient at signifcant risk of death, acute exacerbation/decompensation, or functional decline are eligible for CCM services. ● Billing practitioners may consider identifying patients who require CCM services using criteria suggested in CPT guidance (such as number of illnesses, number of medications or repeat admissions or emergency department visits) or the profile of typical patients in the CPT prefatory language. ● There is a need to reduce geographic and racial/ethnic disparities in health through provision of CCM services. Table 2 provides a number of resources for identifying and engaging subpopulations to help reduce these disparities. The billing practitioner cannot report both complex and regular (non-complex) CCM for a given patient for a given calendar month. In other words, a given patient receives either complex or non-complex CCM during a given service period, not both. Examples of chronic conditions include, but are not limited to, the following: ● Alzheimer’s disease and related dementia ● Arthritis (osteoarthritis and rheumatoid) ● Asthma ● Atrial fbrillation ● Autism spectrum disorders ● Cancer ● Cardiovascular Disease ● Chronic Obstructive Pulmonary Disease ● Depression ● Diabetes ● Hypertension ● Infectious diseases such as HIV/AIDS Initiating Visit For new patients or patients not seen within one year prior to the commencement of CCM, Medicare requires initiation of CCM services during a face-to-face visit with the billing practitioner (an Annual Wellness Visit [AWV] or Initial Preventive Physical Exam [IPPE], or other face-to-face visit with the billing practitioner). This initiating visit is not part of the CCM service and is separately billed. Practitioners who furnish a CCM initiating visit and personally perform extensive assessment and CCM care planning outside of the usual effort described by the initiating visit code may also bill HCPCS code G0506 (Comprehensive assessment of and care planning by the physician or other qualifed health care professional for patients requiring chronic care management services [billed separately from monthly care management services] [Add-on code, list separately in addition to primary service]). G0506 is reportable once per CCM billing practitioner, in conjunction with CCM initiation. Patient Consent Obtaining advance consent for CCM services ensures the patient is engaged and aware of applicable cost sharing. It may also help prevent duplicative practitioner billing. A practitioner must obtain patient consent before furnishing or billing CCM. Consent may be verbal or written but must be documented in the medical record, and includes informing them about: ● The availability of CCM services and applicable cost-sharing ● That only one practitioner can furnish and be paid for CCM services during a calendar month ● The right to stop CCM services at any time (effective at the end of the calendar month) Definition: Indicates an Evaluation and Management (E/M) service resulted in the initial decision to perform surgery either the day before a major surgery (90 day global) or the day of a major surgery. You can access this information on the Medicare Physicians Fee Schedule Data Base.
APPROPRIATE:
INAPPROPRIATE:
Below are information that you need to understand and remember; many are still confused with this: Global period is the day before surgery, the day of the surgery and the number of days following the surgery as indicated on the MPFSDB. Often, a major surgery has a 90 day post operative period and a minor surgery has either a zero or a 10 day post operative period. A preoperative period is the day before the surgery or the day of surgery. When an E/M service resulting in the initial decision to perform major surgery is furnished during the post-operative period of another, unrelated procedure, then the E/M service must be billed with both the 24 and 57 modifiers. See Codes: 92002-92014 E/M Ophthalmology Services 99201-99499 E/M all locations Definition: Bilateral Procedure; procedures/services that occur on identical, opposing structures (such as for example - "LEFT" and "RIGHT" Side)
Many Billers are still really confused on how Modifier 50 really works. APPROPRIATE:
Billed as 64490 -50 1 unit
INAPPROPRIATE:
Coding Tip: Generally speaking, the above information applies when two of the same procedure codes are performed on the same day for the same patient by the same provider. However, there could be instances where two separate procedure codes are used. If so, Medicare's payment or denial would depend on any other type of rules or regulations concerning the individual services in question. This could include the National Correct Coding Initiative (NCCI) that could necessitate additional modifiers, duplicate edits, and global surgery edits. Remember, the Modifier 50 is used as a payment, rather than informational, modifier. The addition of this modifier could affect payment depending on the procedure code and the BILAT SURG indicator. The BILAT SURG indicator for each procedure code can be found on the Medicare Physician Fee Schedule Relative Value File. Following are the indicators and their descriptions. BILAT SURG indicator "0" =150% payment adjustment for bilateral procedures does not apply. If procedure is reported with modifier -50 or with modifiers RT and LT, base the payment for the two sides on the lower of: (a) the total actual charge for both sides and (b) 100% of the fee schedule amount for a single code. Example: The fee schedule amount for code XXXXX is $125. The physician reports code XXXXX-LT with an actual charge of $100 and XXXXX-RT with an actual charge of $100. Payment should be based on the fee schedule amount ($125) since it is lower than the total actual charges for the left and right sides ($200). The bilateral adjustment is inappropriate for codes in this category (a) because of physiology or anatomy, or (b) because the code description specifically states that it is a unilateral procedure and there is an existing code for the bilateral procedure. BILAT SURG Indicator "1" =150% payment adjustment for bilateral procedures applies. If the code is billed with the bilateral modifier or is reported twice on the same day by any other means (e.g., with RT and LT modifiers, or with a 2 in the units field), base the payment for these codes when reported as bilateral procedures on the lower of: (a) the total actual charge for both sides or (b) 150% of the fee schedule amount for a single code. If the code is reported as a bilateral procedure and is reported with other procedure codes on the same day, apply the bilateral adjustment before applying any multiple procedure rules. Reference Manual: The CMS Internet-Only Manual, Publication 100-04, Chapter 12 , Section 40.7.B, indicates "If a procedure is not identified by its terminology as a bilateral procedure (or unilateral or bilateral), physician must report the procedure with modifier "-50". They report such procedure as a single line item." BILAT SURG Indicator "2" =150% payment adjustment does not apply. Relative Value Units (RVUs) are already based on the procedure being performed as a bilateral procedure. If the procedure is reported with modifier -50 or is reported twice on the same day by any other means (e.g., with RT and LT modifiers or with a 2 in the units field), base the payment for both sides on the lower of (a) the total actual charge by the physician for both sides, or (b) 100% of the fee schedule for a single code. Example: The fee schedule amount for code YYYYY is $125. The physician reports code YYYYY-LT with an actual charge of $100 and YYYYY-RT with an actual charge of $100. Payment should be based on the fee schedule amount ($125) since it is lower than the total actual charges for the left and right sides ($200). The RVUs are based on a bilateral procedure because (a) the code descriptor specifically states that the procedure is bilateral, (b) the code descriptor states that the procedure may be performed either unilaterally or bilaterally, or (c) the procedure is usually performed as a bilateral procedure. BILAT SURG Indicator "3" = the usual payment adjustment for bilateral procedures does not apply. If the procedure is reported with modifier -50 or is reported for both sides on the same day by any other means (e.g., with RT and LT modifiers or with a 2 in the units field), base the payment for each side or organ or site of a paired organ on the lower of (a) the actual charge for each side or (b) 100% of the fee schedule amount for each side. If the procedure is reported as a bilateral procedure and with other procedure codes on the same day, determine the fee schedule amount for a bilateral procedure before applying any multiple procedure rules. Services in this category are generally radiology procedures or other diagnostic tests which are not subject to the special payment rules for other bilateral surgeries. BILAT SURG Indicator "9" = The bilateral payment adjustment concept does not apply. Ambulatory Surgical Centers (ASCs) and Modifier 50 Bilateral surgical procedures furnished by certified ASCs may be covered under Part B. While use of the 50 modifier is not prohibited according to Medicare billing instructions, the modifier is not recognized for payment purposes and if used, may result in incorrect payment to ASCs. Bilateral procedures should be reported as a single unit on two separate lines or a single unit with "2" in the unit field on one line, in order for both procedures to be paid correctly. The multiple procedure reduction of 50 percent will apply to all bilateral procedures subject to multiple procedure discounting. Read more examples for appropriate billing procedures in the MLN Matters article, "Revised Payment System for Ambulatory Surgical Centers (ASC) in Calendar Year (CY) 2008" (Revised SE 0742). References: CMS: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf Noridian: https://med.noridianmedicare.com/web/jeb/specialties/surgery/bilateral-surgery American Medical Association Coding Guidelines Definition: Unrelated evaluation and management (E/M) service by the same physician* during a postoperative period APPROPRIATE:
INAPPROPRIATE:
*Same physician - Medicare regulation states: "Physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician." Reporting Multiple Surgery Modifiers on the Same Claim Line The following is an example of appropriate reporting of both modifiers 24 (Unrelated E/M by the same physician during a postoperative period), and 25 (Significant, separately identifiable E/M by the same physician on the same day of the procedure or other service), on the same E/M code. Many are still confused on this. But here... "A physician performs a major surgery and within the global period sees the patient for an unrelated E/M visit. During this unrelated E/M visit, the physician determines the necessity of a minor surgery or other procedure. This minor surgery/other procedure is significant and separately identifiable from the E/M and unrelated to the original major surgery. Both the 24 and 25 modifiers are appropriate to add to the E/M code. The 24 modifier is appropriate because the E/M service is unrelated and during the postoperative period of the major surgery. The 25 modifier is necessary to identify that the minor surgery/procedure performed on the same day is separately identifiable from the E/M service. In addition, the minor surgery procedure code may need a 79 modifier to indicate the procedure is not related to the major surgery." Definition: Increased Procedural Service requiring work substantially greater than typically required.
The RIGHT WAY:
When the modifier 22 is used, two separate documents will be required to support the claim:
Important Information for Billing and Documentation Based on Medicare's Guideline of which most payers does follow Medicare's Guideline. So pay attention on this: If you append a 22 modifier to a procedure you will receive an Additional Documentation Request (ADR) letter requesting medical records to support the use of the 22 Modifier. It is important that both the operative report and a separate concise statement on why it was beyond the normal difficulty be returned with a copy of the ADR letter. Failure to submit the statement and documentation in a timely fashion will result in processing of the claim with the fee schedule rate for the same surgery submitted without the 22 modifier. Documentation Tips: When developing a separate statement avoid using a generalized statement. Comments like "patient was obese" or "surgery took longer than usual" or "multiple adhesions" lack specific details which identify why the procedure was beyond the normal difficulties that could be encountered with the procedure. Further, it is important that your operative note supports the statement on why the surgical procedure was beyond the ordinary range of difficulty. Unassigned Claim For unassigned claims, an increase in the limiting charge is allowed only when a charge above the fee schedule amount is justified. Reference CMS Manual Instruction: The CMS Internet-Only Manual (IOM) Publication 100-04, Chapter 12 , Section 20.4.6 shows the requirements for using this modifier. How to use MODIFIERS for MEDICAL AND GLOBAL SURGERY Encounters - GoHealthcare is a Leader in Revenue Cycle Management. I have shared a lot of guidelines on each of this modifier. But today, this blog post will cover from Modifier 22 to Modifier 99. So are you ready? Make sure to click on "DIG DEEPER" for learn more and read more on clinical scenario samples. All of these guidelines are based on Medicare's Guidelines. References are attached on each guideline. I strongly believe 98% of all the commercial payers does follow Medicare's Guidelines. Period. Modifier 22
Increased Procedural Services (Dig Deeper to learn more ... CLICK HERE) Modifier 23 Unusual Anesthesia Modifier 24 Unrelated Evaluation and Management Service by the Same Physician or Other Qualified Health Care Professional During a Postoperative Period (Dig Deeper to learn more ... CLICK HERE) Modifier 25 Significant, Separately Identifiable Evaluation and Management Service by the Same Physician or Other Qualified Health Care Professional on the Same Day of the Procedure or Other Service Modifier 26 Professional Component Modifier 27 Multiple Outpatient Hospital E/M Encounters on the Same Date Modifier 32 Mandated Services Modifier 33 Preventive Services Modifier 47 Anesthesia by Surgeon Modifier 50 Bilateral Procedure (Dig Deeper to learn more ... CLICK HERE) Modifier 51 Multiple Procedures Modifier 52 Reduced Services Modifier 53 Discontinued Procedure Modifier 54 Surgical Care Only Modifier 55 Postoperative Management Only Modifier 56 Preoperative Management Only Modifier 57 Decision for Surgery (Dig Deeper to learn more ... CLICK HERE) Modifier 58 Staged or Related Procedure or Service by the Same Physician or Other Qualified Health Care Professional During the Postoperative Period (Dig Deeper to learn more ... CLICK HERE) Modifier 59 Distinct Procedural Service (Dig Deeper to learn more ... CLICK HERE) Modifier 62 Two Surgeons Modifier 63 Procedure Performed on Infants less than 4 kg Modifier 66 Surgical Team Modifier 73 Discontinued Out-Patient Hospital/Ambulatory Surgery Center (ASC) Procedure Prior to the Administration of Anesthesia Modifier 74 Discontinued Out-Patient Hospital/Ambulatory Surgery Center (ASC) Procedure After Administration of Anesthesia Modifier 76 Repeat Procedure or Service by Same Physician or Other Qualified Health Care Professional Modifier 77 Repeat Procedure by Another Physician or Other Qualified Health Care Professional Modifier 78 Unplanned Return to the Operating/Procedure Room by the Same Physician or Other Qualified Health Care Professional Following Initial Procedure for a Related Procedure During the Postoperative Period Modifier 79 Unrelated Procedure or Service by the Same Physician or Other Qualified Health Care Professional During the Postoperative Period (Dig Deeper to learn more ... CLICK HERE) Modifier 80 Assistant Surgeon Modifier 81 Minimum Assistant Surgeon Modifier 82 Assistant Surgeon (when qualified resident surgeon not available) Modifier 90 Reference (Outside) Laboratory Modifier 91 Repeat Clinical Diagnostic Laboratory Test Modifier 92 Alternative Laboratory Platform Testing Modifier 95 Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunications System Modifier 96 Habilitative Services Modifier 97 Rehabilitative Services Modifier 99 Multiple Modifiers Billing and Coding for Orthopedic Spinal Fusion Let's begin with some terminology to remember;
Understanding the Posterior Lumbar Interbody Spinal Fusion 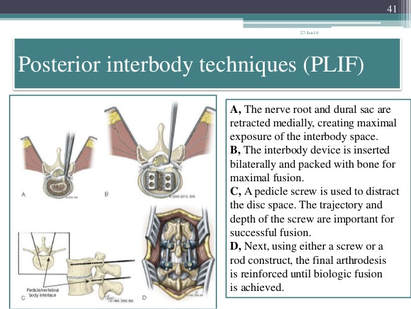 Techniques:
Image Source: https://www.slideshare.net/drpraveenktripathi/lumbar-interbody-fusion-indications-techniques-and-complications
Your CPT® Codes for PLIF and TLIF Spinal Fusion Coding: CPT Code 22630, +22632 22630 Arthrodesis, posterior interbody technique, including laminectomy and/or discectomy to prepare interspace (other than for decompression), single interspace; lumbar +22632 Each Additional interspace (list separately in addition to code for primary procedure code) Here's what occurs when 22630 is performed: The provider performs an arthrodesis, also known as spinal fusion, in the lumbar spine, or lower back, to permanently join two vertebrae, the interlocking bones of the spine. He excises the lamina and disk material and applies bone graft between the disks to fuse them. The procedure helps to alleviate persistent pain caused by various spinal conditions, including herniated intervertebral disks, stenosis, or spinal injuries. Then, in 2012 Code 22633 was introduced to to represent the combination of 22630 and 22612 Arthrodesis, posterior or posterolateral technique, single level; lumbar (with lateral transverse technique, when performed) at the same level. The Anterior Interbody Fusion Approach
Videos to watch for Procedure PLIF and TLIF Your CPT® Codes for ALIF, DLIF and OLIF Spinal Fusion Coding: CPT Code 22558, +22585 22558 Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace (other than for decompression); lumbar Remember: (For arthrodesis using pre-sacral interbody technique, see 22586, 0195T) +22585 Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace (other than for decompression); each additional interspace (List separately in addition to code for primary procedure) Remember: (Use 22585 in conjunction with 22554, 22556, 22558) (Do not report 22585 in conjunction with 63075, even if performed by a separate individual. To report anterior cervical discectomy and interbody fusion at the same level during the same session, use 22552) Here's what occurs when 22558 is being performed: The provider performs arthrodesis, also known as spinal fusion, in the lower back, to permanently join two vertebrae, the interlocking bones of the spine, to alleviate persistent pain caused by a herniated, or bulging, disk, or other spinal condition. He makes an incision in the abdomen to access the spine and remove disk material. Instrumentation may be required to stabilize the Spinal Fusion POSTERIOR INSTRUMENTATION: Add-Code +22840 Posterior non-segmental instrumentation (eg, Harrington rod technique, pedicle fixation across 1 interspace, atlantoaxial transarticular screw fixation, sublaminar wiring at C1, facet screw fixation) (List separately in addition to code for primary procedure) (Use 22840 in conjunction with 22100-22102, 22110-22114, 22206, 22207, 22210-22214, 22220-22224, 22310-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300-63307) Add-On Code +22841 Internal spinal fixation by wiring of spinous processes (List separately in addition to code for primary procedure) Add-On Code +22842 Posterior segmental instrumentation (eg, pedicle fixation, dual rods with multiple hooks and sublaminar wires); 3 to 6 vertebral segments (List separately in addition to code for primary procedure) Use 22842 in conjunction with 22100- 22102, 22110- 22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300- 63307)Text has been updated Add-On Code +22843 7 to 12 vertebral segments (List separately in addition to code for primary procedure) (Use 22843 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081,63085, 63087, 63090, 63101, 63102, 63170-63290,63300- 63307)Text has been updated Add-On Code +22844 13 or more vertebral segments (List separately in addition to code for primary procedure) (Use 22844 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300- 63307) ANTERIOR INSTRUMENTATION Add-On Code +22845 Anterior instrumentation; 2 to 3 vertebral segments (List separately in addition to code for primary procedure) (Use 22845 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081,63085, 63087, 63090, 63101, 63102, 63170-63290,63300- 63307)Text has been updated Add-On Code +22846 4 to 7 vertebral segments (List separately in addition to code for primary procedure) Use 22846 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300- 63307)Text has been updated Add-On Code +22847 8 or more vertebral segments (List separately in addition to code for primary procedure) (Use 22847 in conjunction with 22100-22102, 22110-22114, 22206, 22207, 22210-22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040- 63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290,63300-63307)Text has been updated Add-On Code +22848 Pelvic fixation (attachment of caudal end of instrumentation to pelvic bony structures) other than sacrum (List separately in addition to code for primary procedure) (Use 22848 in conjunction with 22100- 22102, 22110-22114, 22206, 22207, 22210- 22214, 22220-22224, 22305-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300- 63307)  Co-Surgeon Modifier 62 may not be appended with your Instrumentation Codes! Spinal Prosthetic Devices may also be required to be reported CPT Code 22853 22853 Insertion of interbody biomechanical device(s) (eg, synthetic cage, mesh) with integral anterior instrumentation for device anchoring (eg, screws, flanges), when performed, to intervertebral disc space in conjunction with interbody arthrodesis, each interspace (List separately in addition to code for primary procedure) Notes: (Use 22853 in conjunction with 22100-22102, 22110-22114, 22206, 22207, 22210-22214, 22220-22224, 22310-22327, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812, 63001-63030, 63040-63042, 63045-63047, 63050-63056, 63064, 63075, 63077, 63081, 63085, 63087, 63090, 63101, 63102, 63170-63290, 63300-63307) (Report 22853 for each treated intervertebral disc space) Code +22853 is one of several new codes within the spine section for the insertion of biomechanical devices that replace deleted code +22851 (Application of intervertebral biomechanical device[s] ...). The new add-on codes are more specific regarding the type and location of the biomechanical devices. CPT® guidelines direct you to report +22853 for each treated intervertebral disc space. Report +22853 in addition to the definitive procedure(s) since it is an add-on code. Do not append modifier 62 (Two surgeons) to 22853. The provider inserts a metallic cage or mesh device between two vertebrae and may use screws or flanges to attach it to the front part of the vertebrae; the device maintains the disc space, provides spinal stability, and yet preserves some range of motion, which helps relieve persistent pain caused by a herniated, or bulging, disk or other spinal condition. The provider performs this procedure during a spinal interbody arthrodesis procedure, which is fusion, or permanent joining, of vertebrae over the joint space. Remember! Code +22853 is an add–on code and must be reported with an appropriate primary procedure, such as 22548–22586 (Anterior or anterolateral approach technique arthrodesis procedures on the spine [vertebral column]), but there are many other codes that can be reported as a primary code. Report one unit of this code for each interspace treated, not for the number of devices inserted. For example, if the provider inserts two cages into a single interspace, you report this code only once. If the provider inserts a device at two separate interspaces, e.g., between C3–4 and C5–6, then you would report this code twice. This code is for the application of a device to expand or maintain an intervertebral disc space. For a similar procedure to cover a defect created by removal of a vertebral body, report 22854 (Insertion of intervertebral biomechanical device(s) [e.g., synthetic cage, mesh] with integral anterior instrumentation for device anchoring [e.g., screws, flanges], when performed, to vertebral corpectomy[ies] [vertebral body resection, partial or complete] defect, in conjunction with interbody arthrodesis, each contiguous defect [List separately in addition to code for primary procedure]). For insertion of a similar device to treat an intervertebral disc space or vertebral body removal defect but without interbody fusion (arthrodesis), report 22859 (Insertion of intervertebral biomechanical device[s] [e.g., synthetic cage, mesh, methylmethacrylate] to intervertebral disc space or vertebral body defect without interbody arthrodesis, each contiguous defect [List separately in addition to code for primary procedure]). Report Bone Grafting if allowable, CPT Code 20930 20930 Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition to code for primary procedure) Notes: (Use 20930 in conjunction with 22319, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) Here's what occurs when 20930 is being performed; The provider applies small pieces of donor or synthetic bone graft material during a spinal surgery to encourage bone growth during the healing period. Coding Tip! Code 20930 is an add on code and used for specified spinal procedures only. Check with your payer to determine if 20930 can be billed separately or if the application of the bone graft material is included in the code for the primary surgical procedure. Do not append modifier 62 to bone graft codes 20900-20938. (For spinal surgery bone graft[s] see codes 20930-20938) Check with your payer if you can separately report this code; +20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Notes: (Use 20931 in conjunction with 22319, 22532-22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) A provider uses a structural allograft, a type of donor bone, to fill in bony defects as she performs a spinal surgery procedure. Coding Tips: Code 20931 is an add on code describing application of structural allograft to spinal defects and must be reported with an allowable primary spinal procedure code. Report 20930, Allograft, morselized, or placement of osteopromotive material, for spine surgery only, together with 20931 only in the case of a human donor who is a different person from the recipient. You should never append modifier 50, Bilateral procedure, to 20931. The CMS Physician Fee Schedule Database includes a 9 indictor in the BILAT SURG column for this code. According to further CMS instructions, a 9 indicator in this column means that the concept of a bilateral surgery with spinal grafting does not apply. +20936 Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar fragments) obtained from same incision (List separately in addition to code for primary procedure) Notes: (Use 20936 in conjunction with 22319, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) A provider uses an autograft, a type of donor bone, to fill in bony defects as she performs a spinal surgery procedure. She extracts the autograft from the patient’s own bone, taken from the same surgical incision. Coding Tips: Code 20936 is an add on code describing grafting from a donor area using the same incision during a major operative procedure and must be reported with an allowable primary spinal procedure code. You should never append modifier 50, Bilateral procedure, to 20936. The CMS Physician Fee Schedule Database includes a 9 indictor in the BILAT SURG column for this code. According to further CMS instructions, a 9 indicator in this column means that the concept of a bilateral surgery with spinal grafting does not apply. +20937 Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial incision) (List separately in addition to code for primary procedure) Notes: (Use 20937 in conjunction with 22319, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) The provider uses an autograft, a type of donor bone, to fill in bony defects as she performs a spinal surgery procedure. She extracts the autograft from the patient’s own body during the surgical procedure, through a separate incision. Coding Tips: Code 20937 is an add on code describing preparation and application of a morselized autograft through a separate skin incision and must be reported with an allowable primary spinal procedure code. *** A vertebral segment describes the basic constituent part into which the spine may be divided. It represents a single complete vertebral bone with its associated articular processes and laminae. A vertebral interspace is the non-bony compartment between two adjacent vertebral bodies which contains the intervertebral disc, and includes the nucleus pulposus, annulus fibrosus, and two cartilaginous endplates. Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate skin or fascial incision) (List separately in addition to code for primary procedure) Notes: (Use 20938 in conjunction with 22319, 22532, 22533, 22548-22558, 22590-22612, 22630, 22633, 22634, 22800-22812) (For aspiration of bone marrow for bone grafting, spine surgery only, use 20939) The provider uses an autograft, a type of donor bone, to fill in bony defects as she performs a spinal surgery procedure. She extracts the autograft from the patient's own body during the surgical procedure, through a separate incision. Reporting Cosurgeries Source: CPT® Assistant July 1996 page 7 Coding Tip Reporting Cosurgeries "We receive many questions concerning how to report surgeries performed by more than one physician. To help you understand the proper coding we present the following information." The General Question "I am a general surgeon who sometimes performs surgeries with other surgeons (cosurgeries), such as orthopedic or neurosurgeons. I open the surgical site, the other surgeon does the definitive portion of the procedure, and then I close. What CPT codes should I report for my services? I have heard from some sources that I should bill for a thoracotomy and wound repair. But other sources have told me to report the same CPT codes as the other surgeon. Which is correct? CPT® ASSISTANT'S REPLY: Here's How to Code: "For situations in which one surgeon performs the opening and closing of a surgery and another physician performs the definitive portion of the procedure, both physicians should report the same CPT codes, and appropriately append either modifier -62 or modifier -66." Illustration A patient's surgery includes arthrodesis of two interspaces of the thoracic spine by anterior interbody technique, with anterior instrumentation of three vertebral segments. Physician "A" performs a thoracotomy at the start of the surgical session, and Physician "B" performs the arthrodesis and spinal instrumentation. Upon completion of the arthrodesis and spinal instrumentation, Physician A closes the operative site. Coding the Illustration (The physicians in the illustration would report the codes indicated below.) Physician A 22556-62 Physician B 22556-62 22558-62 22558-62 22845-62 22845-62 When performing these cosurgeries, it is important to communicate with the other surgeon's office to be certain that you submit the claims properly 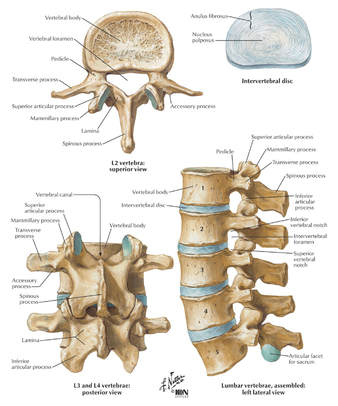 CPT® Guideline September 1997 page 8 Coding Communication How to Code Prosthetic Devices It is not often that we devote an entire article to a single code, but sometimes this is the only way to fully explain the use of certain codes-22851, application of prosthetic device (eg, metal cages, methylmethacrylate) to vertebral defect or interspace, is such a code. But before we review how to report this code, it is probably a good idea to first do a brief anatomical review of the vertebral column. The vertebral column (spine) consists of a series of bones known as vertebrae. An adult human possesses 33 vertebrae divided into the following five types: 7 cervical vertebrae; 12 thoracic vertebrae; 5 lumbar vertebrae; 5 sacral vertebrae; and 4 coccygeal vertebrae. The sacral vertebrae are typically fused into a single bone known as the sacrum. The coccygeal vertebrae are sometimes fused into a single bone known as the coccyx. Therefore, the actual number of bones in the vertebral column may be 26-29, depending on if the coccygeal vertebrae are fused. Vertebrae are commonly named by a letter that corresponds to the region of the vertebral column to which the vertebrae belongs, followed by a number that indicates where in the region the vertebrae is located. For example, the most superior cervical vertebra is called C1, with the next cervical vertebrae down designated C2. The most superior thoracic vertebrae is T1, with the next one down designated T2. Fig. 1 - Spinal Prosthetic Devices Between each pair of vertebrae is a disc that cushions the spinal column. If one of the discs degenerates or if one of the 26-29 vertebrae are injured (as in the case of a fracture, degenerative disease, or secondary to tumor destruction) the physician may need to place a prosthetic device (eg, metal cages or methyl-methacrylate) in the vertebral defect or interspace. (Fig. 1) In these instances, a segment of vertebral level may be drilled and metal cages packed with porous implants of bone graft may be inserted or methylmethacrylate may be placed between the affected vertebrae. Proper Reporting of code 22851 It is important to note that CPT® code 22851 is not intended to be reported per cage. CPT® code 22851 should only be reported one time, regardless if one or more metal cages are placed in the intervertebral space at the same level. However, if metal cages are placed at two different levels, (eg, metal cage placed at L3-4 interspace and L5-S1 interspace), then 22851 may be reported more than once to indicate that one or more cages were placed at two or more different levels. It is important to note that a single cage or methylmethacrylate can cover a defect of several vertebral segments (eg, a single cage may replace three entire vertebrae), wherein code 22851 would still only be reported one time. Within the spine section, instrumentation procedure codes (22840-22855) are reported in addition to the definitive procedure(s) without appending the modifier -51. Therefore, if arthrodesis is performed in addition to the placement of the metal cages, then it would be appropriate to report code 22851 in addition to the appropriate arthrodesis code, 22548-22632. In this instance, the modifier -51 would not be appended to code 22851. If metal cages are placed through an anterior approach and pedicle screws are placed through a posterior approach, it would be appropriate to report both code 22851 and one of the codes from the posterior instrumentation series, 22840, 22842-22844. However, if different instrumentation is used in addition to the metal cages or methylmethacrylate through the same approach (eg, an anterior plating system) or pedicle screws and posterior lumbar interbody fusion utilizing cages), then the appropriate instrumentation code would be reported in addition to code 22851. However, 22851 and 22845 should not both be reported if only the metal cage is inserted. If fracture treatment, dislocation, or arthrodesis is performed in addition to spinal instrumentation, then the appropriate fracture treatment, dislocation or arthrodesis code (22325, 22326, 22327, 22548-22812) would be reported separately in addition to code 22851. In this instance, CPT® code 22851 would be reported in addition to the definitive procedure(s) without the modifier -51 appended. If bone grafting is performed in addition to code 22851, then the appropriate bone grafting code, 20930-20938, would be reported additionally. Clinical Sample: CPT® Code 22851 A 50-year-old man undergoes an anterior fusion of L5-S1 for degenerative disease. A retroperitoneal incision is made and an arthrodesis performed using a BAK cage. A distracter is placed in the interspace, a hole is drilled in the interspace, and the BAK cage is placed in the hole. The spacer is removed and replaced with another BAK cage. Both cages are filled with bone graft. (Report arthrodesis and/or bone grafting separately using the appropriate CPT code[s]). The exposed disk space and adjacent vertebrae are prepared with bone-cutting instruments for acceptance of the prosthetic device. Preparation of the recipient site is made according to the protocol of the particular device. If methylmethacrylate is to be used, a screw or pin may be inserted into the adjacent vertebral surfaces to anchor the methylmethacrylate. Provision is made for cooling of adjacent tissues and protection of heat sensitive tissue from the exothermic reaction of the curing of the methylmethacrylate. For cages, the recipient site is prepared by bone dissection, a trial fit with the device or a spacer or template as indicated by the protocol is inserted and removed for any final modifications of the recipient site. The prosthetic device is then screwed, impacted, or injected into place according to protocol for this particular device. (Additional fixation, other provision for arthrodesis, or bone grafting are coordinated with the placement of the prosthetic device and are coded separately.) For devices that incorporate graft material, that material is appropriately placed into the device prior to its final insertion. CPT® ASSISTANT September 2000 page 10 Coding Consultation Musculoskeletal System, Surgery, 22548-22585, 22899 (Q&A) Question "Should I use the anterior or anterolateral approach technique arthrodesis series of codes (22548-22585) to report intra-abdominal laparoscopic, video assisted anterior interbody fusion?" AMA CPT® Comment "The anterior or anterolateral approach technique arthrodesis series of codes (22548-22585) are intended to describe arthrodesis performed via an open surgical approach. There is not a specific CPT code that accurately describes laparoscopic anterior interbody fusion. Therefore, code 22899, Unlisted procedure, spine should be reported. When reporting an unlisted code to describe a procedure or service, it will be necessary to submit supporting documentation (eg, procedure report) along with the claim to provide an adequate description of the nature, extent, need for the procedure, and the time limit, effort, and equipment necessary to provide the service." CPT® ASSISTANT March 2015 page 9 Frequently Asked Questions:Surgery: Musculoskeletal System Question: "Are CPT codes 22851 and 22845 appropriate to report when modular implants, such as the RSB (RSB LLC; Cleveland, OH) InterPlate® (a modular interbody platform technology), are implanted for spinal fusion procedures?" Answer: "No. The RSB InterPlate® describes a stand-alone interbody fusion device that consists of an interbody spacer with screw fixation or other mechanisms, which engage adjacent vertebrae. Such devices should be reported with code 22558, Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace (other than for decompression); lumbar, and 22851, Application of intervertebral biomechanical device(s) (eg, synthetic cage(s), methylmethacrylate) to vertebral defect or interspace (List separately in addition to code for primary procedure). An additional anterior instrumentation code (22845) is not applicable because there is no separate construct placed across the vertebral segment." Question: "Would it be appropriate to separately report any of the following with the hammertoe correction code 28285 (2nd digit), if adequately documented? (1) Resection of hypertrophied base of proximal phalanx (28126), if performed through a separate incision at the metatarsophalangeal (MTP joint); (2) flexor tenotomy (28232) performed through a separate incision at the distal interphalangeal (DIP) joint; (3) an additional unit of 28285 if K-wire is inserted through the DIP, MTP, or proximal interphalangeal (PIP) joint." Answer: "No. Code 28126, Resection, partial or complete, phalangeal base, each toe; code 28232, Tenotomy, open, tendon flexor; toe, single tendon (separate procedure); and the insertion of K-wire through DIP, PIP, and MTP joints are all inclusive components of the procedure described by code 28285, Correction, hammertoe (eg, interphalangeal fusion, partial or total phalangectomy), and should not be reported separately." References: 2020 AMA's CPT® Guidelines 2019 AMA's CPT® Guidelines 2018 AMA's CPT® Guidelines 2017 AMA's CPT® Guidelines CPT® Assistant Archives Websites: NASS Spine-Health Medtronic Ahima AAPC CMS All other commercial payers clinical guidelines from the public domains on the internet Read more blog posts: |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985






 RSS Feed
RSS Feed