|
Understand the necessity of Prior Authorization (PA) in healthcare delivery, especially in orthopedics, pain management, and hospital settings. Unpack the detailed PA process and discover the best PA services for surgeons, providers, and hospitals. At GoHealthcare Practice Solutions, we specialize in providing an essential service to the healthcare sector – Prior Authorization (PA) services. As a trusted partner for surgeons, providers, and hospitals, we are committed to delivering timely, accurate, and comprehensive PA approvals, reducing the administrative burden on medical professionals, and ensuring the uninterrupted flow of patient care. Our goal is to facilitate seamless healthcare experiences, particularly within orthopedic, pain management, and hospital contexts, by managing the often complicated and time-consuming PA process. Understanding the IMPORTANCE AND PROCESS OF PRIOR AUTHORIZATION SERVICES: FOCUSING ON ORTHOPEDIC, PAIN MANAGEMENT, AND HOSPITAL CARE Prior Authorization (PA), also known as pre-approval, is an essential component of healthcare delivery, serving as a gatekeeper between patients, providers, and insurance companies. The process aims to validate the necessity of certain treatments or medications before they are administered, ensuring patient safety, preventing unnecessary procedures, and controlling healthcare costs. When applied correctly, PA services can be a significant force for good in healthcare. However, the process can be complex and challenging. Therefore, it is imperative to understand why PA approvals are so important and the procedures required for a successful application. The Importance of Prior Authorization Approvals. The importance of PA cannot be overstated. Firstly, it helps in maintaining the quality of healthcare services. By requiring prior authorization for orthopedic surgeries, pain management therapies, and other hospital treatments, insurance companies can ensure that the recommended procedures align with evidence-based medicine. It acts as a protective measure, screening out potentially harmful or unnecessary treatments and medications. For instance, in pain management, it may prevent the over-prescription of opioids, mitigating the risk of addiction. Secondly, PA also assists in controlling healthcare costs. It can deter the excessive use of costly treatments when more cost-effective alternatives can provide equivalent outcomes. By mitigating overutilization, PA helps manage healthcare expenditures, potentially translating into lower insurance premiums. Lastly, PA plays a crucial role in promoting transparency. It obliges providers to justify their treatment plans, which fosters open communication between all stakeholders—patients, providers, and payers. The Prior Authorization Process The PA process typically starts when a healthcare provider identifies a service or medication that requires pre-approval from the patient's health insurance company. The steps involved are:
Despite its benefits, the PA process can be time-consuming and complex, often leading to delays in patient care. This is where dedicated PA services, like those offered by XYZ Healthcare Solutions, come into We act as intermediaries between healthcare providers and insurance companies, managing all aspects of the PA process. This includes identifying the need for PA, completing and submitting the necessary paperwork, tracking PA requests, and facilitating communication between the provider and insurer. Our specialized PA service spans across various medical specialties. We provide prior authorization for orthopedic surgeries, handling the intricate approval processes associated with various orthopedic procedures such as joint replacements, spinal surgeries, and arthroscopic procedures. We also provide prior authorization for pain management, helping ensure that patients have access to necessary treatments like nerve blocks, epidurals, and opioid medications while minimizing potential misuse. Our team of experts understands the specific requirements for these authorizations and works diligently to expedite approvals. In the broader context of hospital care, we manage PAs for an extensive range of treatments and procedures. This can significantly reduce the administrative burden on hospital staff, allowing them to focus on patient care. With our expert knowledge and experience, we can help streamline the PA process, minimize delays, and ensure that patients receive their treatments in a timely manner. Our goal is to make the PA process as efficient and hassle-free as possible for both providers and patients. Prior authorization is a critical aspect of healthcare delivery. It serves as a quality control measure, ensures cost-effectiveness, and promotes transparency. However, navigating the PA process can be a challenge for many providers. At GoHealthcare Practice Solutions, we're dedicated to making this process easier. Our prior authorization services for surgeons, providers, and hospitals ensure that medical professionals can focus on what they do best – providing excellent patient care – while we handle the administrative complexities of the PA process. We're committed to offering the best PA services, particularly in orthopedics, pain management, and hospital settings. We understand that the sooner a PA is approved, the sooner a patient can receive the necessary care. Together, let's make healthcare more efficient, effective, and patient-centric. Prior Authorization Services: A Necessity Not Just an Option While PA services are indispensable for any healthcare setting, they become crucial when specialized care is involved. The unique challenges in these fields demand a more nuanced understanding of the intricacies involved in the PA process. For instance, the prior authorization for orthopedic procedures involves understanding a wide array of surgeries, each with its own set of considerations. Joint replacements may require justifications for why less invasive methods are not applicable, while spinal surgeries may necessitate a detailed history of conservative treatments before the insurance company approves the procedure. Our PA service in the orthopedic field is equipped to handle these complexities, allowing for a smoother process and more effective outcomes. Similarly, in pain management, the need for PA services becomes more acute due to the ongoing opioid crisis. Ensuring that the treatment is medically necessary, safe, and effective for the patient becomes crucial, requiring careful handling of the PA process. Streamlining the Prior Authorization Process: We have developed a systematic, clinical and physician-patient centric approach to managing the prior authorization process. Accurate Documentation: We ensure that all patient information, diagnosis details, proposed treatment plans, and supporting medical literature is accurately documented and submitted in a timely manner. This not only speeds up the process but also reduces the likelihood of denials due to incomplete or incorrect information. Persistent Follow-ups: We actively follow up on every PA request with the insurance company. Regular follow-ups prevent delays and keep the process moving forward. Managing Denials and Appeals: In case of a denial, we don't just stop there. We work closely with the healthcare provider to understand the reason for denial and collect additional information that can be used for an appeal. Communication: We keep everyone in the loop - patients, providers, and insurance companies. This ensures transparency and builds trust among all parties involved. Prior Authorization for Hospitals: A Special Focus Hospitals face unique challenges when it comes to prior authorization. They deal with a high volume of patients, diverse medical conditions, and a wide array of procedures and treatments. Additionally, hospitals also have to manage administrative work, patient care, and regulatory compliance, which can make the PA process quite overwhelming. Our dedicated prior authorization services for hospitals are designed to handle these challenges efficiently. We have a team of experts who understand hospital operations and the specific PA requirements associated with various hospital treatments. Our aim is to reduce the administrative burden on hospitals, improve operational efficiency, and ultimately enhance patient satisfaction. The Takeaway: Prior Authorization Services as a Valuable Ally In the dynamic and often demanding world of healthcare, services like ours can play an instrumental role in smoothing processes and enhancing outcomes. While the benefits of prior authorization are manifold, the complexities involved in securing approvals can act as hurdles. By leveraging our specialized prior authorization services for orthopedic surgeries, pain management, and hospital care, these obstacles can be effectively addressed. As we continue to evolve, innovate, and refine our offerings at GoHealthcare Practice Solutions, we remain committed to our core mission - facilitating better healthcare experiences by simplifying the PA process. We invite you to partner with us in this mission, and together, let’s create a healthcare environment that is efficient, patient-centric, and transparent. Building Partnerships: A Collaborative Approach to Prior Authorization ServicesIn the healthcare ecosystem, collaboration is key. At GoHealthcare Practice Solutions, we pride ourselves on being more than just a service provider. We aim to be a partner to all our clients - be they surgeons, pain management specialists, or hospitals. By understanding the unique challenges each medical professional faces, we are able to tailor our PA services to meet their specific needs. In our partnership, we work closely with your team, aligning ourselves with your operational workflow, understanding your patient demographics, and acquainting ourselves with your insurance scenarios. This collaboration allows us to provide you with a seamless, integrated prior authorization process. Proactive Problem-Solving: The Future of Prior Authorization Services Looking forward, we at GoHealthcare Practice Solutions believe in a proactive rather than reactive approach to the prior authorization process. Using advanced analytics and predictive modeling, we aim to identify potential roadblocks in the PA process ahead of time and resolve them before they cause delays. By predicting which treatments or medications might require more extensive documentation or may be more likely to be denied, we can preemptively prepare the necessary information, resulting in faster PA approvals. Our Commitment to Continuous Improvement The world of healthcare is constantly evolving, and so are we. We continually invest in our technology and our people to stay ahead of the curve. Regular training and education sessions keep our team up-to-date on the latest trends and changes in the prior authorization landscape. This ensures that we can offer our clients the most efficient and effective PA services, regardless of changes in insurance policies or regulatory requirements. In addition, we are dedicated to refining our processes based on feedback from our clients and their patients. Patient care is at the heart of everything we do. By continually improving our PA services, we can help ensure that patients receive the care they need, when they need it. From understanding the importance of prior authorization approvals to examining the detailed process for securing these approvals, it's clear that prior authorization services play an integral role in the healthcare landscape. Whether you're a surgeon, a provider of pain management services, or a hospital, engaging a specialist in the PA process can help you navigate the often complex approval process, ensuring your patients get timely access to the treatments they need. At GoHealthcare Practice Solutions, we're proud to offer industry-leading prior authorization services. With a particular focus on orthopedics, pain management, and hospital care, we're dedicated to helping you deliver the best possible care to your patients. Reach out to us today to learn more about how we can simplify the PA process for you, freeing you up to focus on what you do best - providing top-notch patient care. The Crucial Connection Between Prior Authorization and Claims Payments Denials: One aspect that truly underscores the importance of a well-managed prior authorization process is the direct impact it has on claims approval. Claims denial due to the lack of or incorrect prior authorization is a common issue plaguing the healthcare industry. Let's delve deeper into this connection. Prior Authorization: A Prerequisite for Claims Approval Insurance companies necessitate prior authorization for certain procedures or treatments to ensure they are medically necessary, align with coverage policies, and prevent misuse of healthcare services. It becomes especially crucial for high-cost procedures like surgeries, advanced diagnostic tests, and specialized treatments in orthopedics and pain management. When a claim is submitted to the insurance company without appropriate prior authorization, it is very likely to be denied. This not only results in non-payment for the provider but also leads to financial stress for patients, administrative hassles, and delays in care delivery. The Impact of Claims Denial Claims denial can have far-reaching consequences. For providers and hospitals, it directly impacts revenue, disrupts cash flow, and adds to administrative costs. The effort required to correct and resubmit denied claims or manage appeals is time-consuming and diverts staff from patient care responsibilities. For patients, claim denials can mean unexpected out-of-pocket costs, leading to financial stress. It also creates dissatisfaction and mistrust, potentially damaging the provider-patient relationship. Navigating the Challenge with Effective Prior Authorization Services At Gohealthcare Practice Solutions, our goal is to minimize claim denials related to prior authorization issues. Our team of experts navigates the intricacies of the prior authorization process to ensure a higher approval rate. Thorough Documentation: We ensure that every PA request is supported by thorough and accurate documentation, presenting a compelling case for the medical necessity of the procedure. Timely Submissions: We adhere to strict timelines for submitting PA requests, ensuring that there are no delays that might lead to procedural postponements and subsequent claims denial. Appeals and Resubmissions: In case of PA denial, we promptly manage the appeal or resubmission process, furnishing additional supporting information as needed. Regular Updates and Follow-ups: We regularly follow up on the status of PA requests and update healthcare providers, ensuring they are informed at every stage of the process. A Preventive Approach: Minimizing Claims Denial Our preventive approach at XYZ Healthcare Solutions is designed to tackle potential issues before they arise. Our specialized prior authorization services not only facilitate prompt PA approvals but also significantly minimize the risk of claims denial. Our experts understand the PA requirements of various insurance companies and are well-versed in the specific prerequisites of different treatments, be it orthopedic surgeries or pain management therapies. Navigating the complex landscape of prior authorization is no easy task, but it's a crucial step in ensuring claims are approved, and timely care is delivered to patients. The role of expert prior authorization services like those offered by GoHealthcare Practice Solutions in mitigating claims denial cannot be overstated. We are committed to providing the best in prior authorization services, allowing healthcare providers to concentrate on their core objective - patient care. With our specialized services, let's together ensure a smoother, more efficient, and patient-centric healthcare delivery system. Eliminating the Need for Peer-to-Peer Reviews: Enhancing Efficiency and Cost-SavingsIn the healthcare landscape, a peer-to-peer review, also known as a physician-to-physician review, often becomes necessary when a prior authorization request is denied by the insurance company. This process involves a conversation between the requesting provider and a doctor representing the insurer, aiming to discuss the case and provide an opportunity for the provider to justify the medical necessity of the requested service. While peer-to-peer reviews can sometimes overturn an initial denial, they require significant investment of time and resources. The need for detailed preparation, scheduling, and follow-ups can detract from a provider’s time that could have otherwise been devoted to patient care. For hospitals and healthcare providers, this can translate into substantial costs, adding to the financial burden. At GoHealthcare Practice Solutions, we understand these challenges and strive to minimize the need for peer-to-peer reviews, ultimately contributing to cost savings for our clients. Mitigating the Need for Peer-to-Peer ReviewsOur strategy revolves around proactive and comprehensive management of the prior authorization process, which significantly reduces the likelihood of initial denials that lead to peer-to-peer reviews. Robust Documentation: We prioritize providing thorough and accurate documentation right from the first PA request. By furnishing comprehensive medical histories, supporting literature, and a clear demonstration of the treatment's necessity, we minimize questions or concerns from the insurer's side. Clear Communication: We maintain open lines of communication with insurance companies, proactively addressing queries and providing clarifications. This reduces misinterpretations or misunderstandings that might lead to a denial. Staying Updated: Our team stays abreast of the ever-evolving insurance policies and guidelines, ensuring that all PA requests comply with the latest insurer requirements. Streamlining the Peer-to-Peer ProcessIn cases where a peer-to-peer review becomes unavoidable, we work closely with providers to streamline the process. We help prepare for the review by gathering all necessary information, scheduling the review at a time convenient for the provider, and assisting in follow-up steps. Prior Authorization Services: Enhancing Profitability and Patient CareBy mitigating the need for time-consuming peer-to-peer reviews, our prior authorization services not only bring about direct cost savings but also allow healthcare professionals to focus on their core task - patient care. This contributes to enhanced patient satisfaction, improved health outcomes, and overall profitability. At GoHealthcare Practice Solutions, our objective extends beyond managing the prior authorization process. We aim to be a partner in your growth, helping streamline operations, reduce costs, and enhance the quality of care. Together, let's create a healthcare system that's efficient, cost-effective, and patient-centric. Our success rate is at 98% and it's a faster turnaround time. We can get started in less than 48 hours. It's a very easy process. We do not have a binding contract. The GoHealthcare Practice Solutions Advantage: High Success Rates, Rapid Turnaround, and MoreOur commitment to delivering excellence in prior authorization services is reflected in our performance metrics. With a success rate of 98%, we pride ourselves on our ability to secure PA approvals quickly and efficiently. Our team's expertise and dedication translate into faster turnaround times, ensuring patients can access needed treatments without unnecessary delays. Swift Implementation, No Binding Contracts. Getting started with us is a breeze. We can have our services up and running for your practice in less than 48 hours. Plus, we believe in our services and the value they provide, so we don't tie you down with a binding contract. Our goal is to make the transition as smooth and hassle-free as possible. Your Return on Investment with GoHealthcare Practice Solutions Choosing GoHealthcare Practice Solutions as your partner in the prior authorization process yields tangible results. Here are the key returns on investment you can anticipate: Cost-Effectiveness: Our services, by mitigating the need for in-house teams to handle prior authorization, help you save on operational costs. Elimination of Unnecessary Peer-to-Peer Process: We minimize the need for time-consuming and resource-intensive peer-to-peer reviews, adding to your bottom line. Solution to Staffing Shortages: By taking over the prior authorization tasks, we help eliminate staffing shortages, ensuring your team can focus on their primary responsibilities. Increased Revenue: Our efficient management of the PA process, combined with a reduction in claim denials, can increase your revenue by up to 35%. Boosted Physician Productivity: With less time spent on administrative tasks, physicians can concentrate more on patient care, boosting their productivity by up to 30%. Don't forget and keep in mind claims denials. This might help you decide why you seriously need help with your prior authorization and utilization management. Understanding Claim Denials: Common Reasons and Mitigation Strategies Claim denials pose significant challenges to healthcare providers, interrupting revenue cycles and adding to administrative burdens. Understanding the common reasons behind denials can help providers better navigate the prior authorization process and enhance their chances of approval. 1. Lack of Prior Authorization: One of the most common reasons for claim denials is the absence of proper prior authorization for the services rendered. Certain procedures, medications, and treatments require pre-approval from the insurance company to ensure their medical necessity and appropriateness. 2. Incorrect Patient Information: Errors in patient demographic details, such as name, date of birth, policy number, or insurance ID, can lead to claim denials. These mistakes can occur due to typographical errors or outdated information. 3. Invalid or Incorrect Procedure or Diagnosis Codes: Every claim submitted needs to include accurate procedure codes (CPT codes) and diagnosis codes (ICD-10 codes). If the codes are incorrect, incomplete, or do not match, the claim can be denied. 4. Service Not Covered by the Plan: Each insurance plan has specific coverage limitations. If the service rendered is not covered under the patient's insurance plan, the claim will be denied. 5. Time Limit for Claim Submission Exceeded: Insurance companies have a specific timeframe within which a claim must be submitted. If the claim is submitted after this period, it is likely to be denied. At GoHealthcare Practice Solutions, our prior authorization services are designed to proactively address these common issues, significantly reducing the risk of claim denials. Our team meticulously ensures each PA request is accompanied by correct patient information, accurate procedure and diagnosis codes, and compelling evidence of medical necessity. We also maintain strict timelines for PA requests and claim submissions, ensuring they are sent within the stipulated periods. By effectively managing these common causes of claim denials, we can help increase your claims approval rate, enhance your revenue, and reduce the administrative burden on your team. With our expert services, claim denials become less of a hurdle and more of a stepping stone towards a streamlined and efficient healthcare practice.
0 Comments
Medicare denial codes, also known as Remittance Advice Remark Codes (RARCs) and Claim Adjustment Reason Codes (CARCs), communicate why a claim was paid differently than it was billed. These codes are universal among all insurance companies. Most of the commercial insurance companies the same or similar denial codes. Pay attention to action that you need to make in order for the claims to get paid. Here are some common Medicare denial codes:
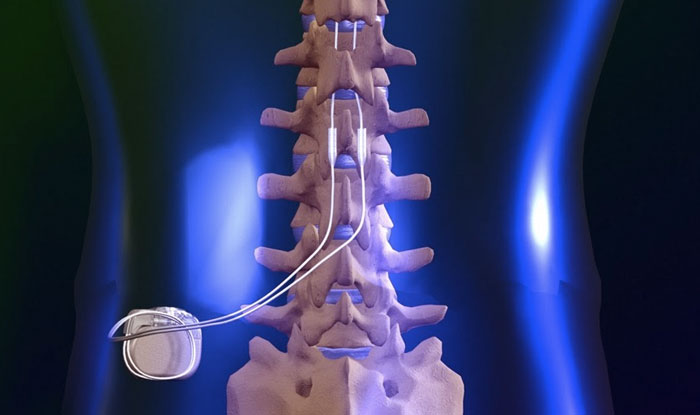
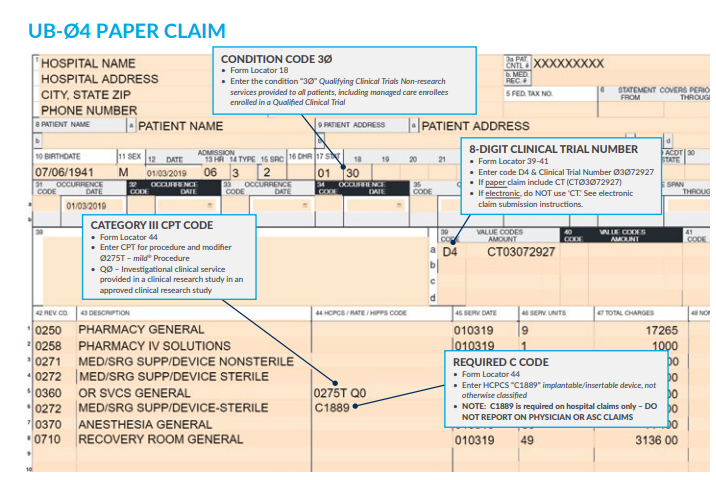
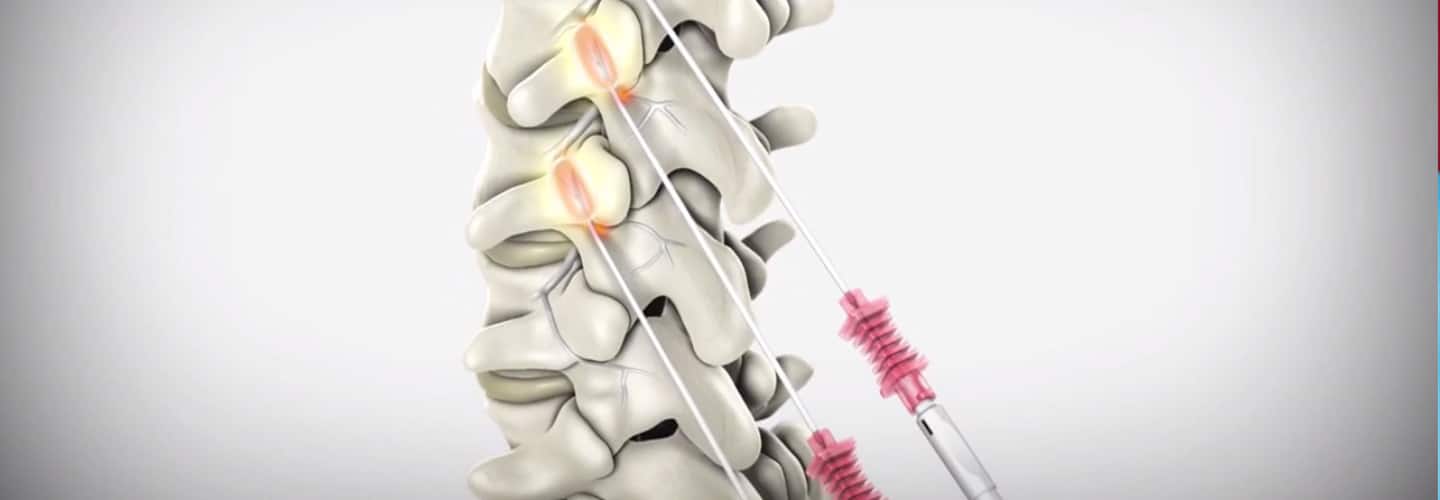
searched keywords: Medicare Denial Codes, Medicare Claims, Claims Denial, Claims Adjustment, Healthcare Providers and Medicare, Understanding Medicare Denial Codes, Medicare Claims Processing, Medicare Coverage, Responding to Medicare Denials, Medicare Claims Adjudication, Medicare Billing, Medicare Coverage Rules, Denial Codes Guide, Medicare Benefits, Medical Billing and Coding Mastering MILD Procedure Billing and Coding: Essential Tips for Maximizing Reimbursement and Ensuring Compliance Discover expert strategies to navigate the complexities of MILD procedure billing and coding. Learn how to streamline the process, optimize reimbursement, and ensure compliance with payer guidelines and industry standards. The Vertos Medical Billing and Coding Guide for 2023 provides detailed information on how to bill and code for the MILD (Minimally Invasive Lumbar Decompression) procedure. The guide refers specifically to the coverage and billing policies of the Centers for Medicare & Medicaid Services (CMS) for this procedure. Here's a detailed and informative explanation of the key points from the guide:
[Your Name, MD]
[Orthopedic Surgeon] [Name of Practice or Hospital] [Address] [ City, State, ZIP] [Phone Number] [Email Address] [Date] [Medical Director or Claims Reviewer's Name] [Insurance Company] [Address] [City, State, ZIP] Re: Medical Necessity of Orthopedic Knee Surgery for [Patient's Full Name] Date of Birth: [Patient's Date of Birth] Policy Number: [Patient's Policy Number] Group Number: [Patient's Group Number] Diagnosis: [ICD-10 Code(s) for Diagnosis] Dear [Medical Director or Claims Reviewer's Name], I am writing to request pre-authorization and to provide a statement of medical necessity for a proposed orthopedic knee surgery for my patient, [Patient's Full Name], who is suffering from [specific knee condition, e.g., severe osteoarthritis, torn meniscus, etc.]. The purpose of this letter is to provide detailed information about the patient's medical history, the proposed surgical intervention, and the expected benefits of the procedure. Medical History: [Patient's Full Name] has been under my care since [date]. Over the past [time period], they have experienced persistent pain, swelling, and reduced mobility in their affected knee, despite conservative treatment options. The patient has tried the following non-surgical interventions:
Proposed Surgical Intervention: After thorough examination, including [relevant diagnostic tests, e.g., X-rays, MRI, etc.], it has been determined that [Patient's Full Name] would benefit from [specific surgical procedure, e.g., total knee arthroplasty, arthroscopic meniscectomy, etc.]. This procedure will involve [briefly describe the surgical intervention, emphasizing the necessity of the procedure to improve the patient's condition]. Expected Benefits of the Procedure: The proposed surgery is medically necessary to alleviate the patient's pain and improve their functional capacity. The benefits of the procedure include:
Please do not hesitate to contact me if you require additional information or clarification. Thank you for your prompt attention to this matter, and I kindly request that you approve this medically necessary procedure for [Patient's Full Name]. Sincerely, [Your Name, MD] [Orthopedic Surgeon] Below is just a sample of a letter of medical necessity for interventional pain management procedure and may not be perfect! Always refer back to your provider, they know better about medical necessity. Sample of Letter of Medical Necessity for Interventional Pain Management Procedure[Your Name]
[Your Address] [City, State, ZIP] [Phone Number] [Email Address] [Date] [Recipient's Name] [Insurance Company Name] [Address] [ City, State, ZIP] Re: Medical Necessity for Interventional Pain Management Procedure Patient: [Patient's Full Name] Policy Number: [Policy Number] Group Number: [Group Number] Date of Birth: [Patient's Date of Birth] Procedure: [Name of the Procedure and CPT Code] Dear [Recipient's Name], I am writing this letter to request pre-authorization and coverage for the interventional pain management procedure, [Name of the Procedure and CPT Code], for my patient, [Patient's Full Name]. I believe this procedure is medically necessary to manage [Patient's Name]'s chronic pain, and I am confident that it will significantly improve their quality of life. [Patient's Name] has been under my care since [Date], and they suffer from [specific pain condition or diagnosis], which has been refractory to conservative treatment measures. [Briefly describe the patient's history, including treatments tried, medications, physical therapy, or other non-invasive modalities that have been ineffective in managing the patient's pain.] Despite these interventions, [Patient's Name] continues to experience significant pain and functional limitations, affecting their ability to perform daily activities, work, and maintain a satisfactory quality of life. As a result, I am recommending [Name of the Procedure], an evidence-based, minimally invasive interventional pain management procedure that has been proven effective in patients with similar conditions. The proposed procedure involves [briefly describe the procedure, including how it targets the specific pain generators and addresses the underlying pathology]. The goal of this procedure is to provide [Patient's Name] with long-lasting pain relief, improved function, and reduced dependence on pain medications, ultimately allowing them to return to a more productive and fulfilling life. Based on my clinical experience, as well as a review of the relevant literature, I believe that this procedure is the most appropriate and effective option for [Patient's Name]. In addition, it has the potential to decrease healthcare costs in the long term by reducing the need for ongoing conservative treatments and opioid medications. I kindly request that you consider this request for pre-authorization and coverage of the proposed interventional pain management procedure for [Patient's Name]. I have attached supporting documentation, including medical records, treatment history, and relevant literature, to further substantiate the medical necessity of this intervention. Thank you for your attention to this matter. Should you require additional information, please do not hesitate to contact me at [Phone Number] or [Email Address]. I look forward to your timely response in approving this medically necessary procedure. Sincerely, [Your Name] [Your Title] [Your Medical Practice Name] [Address] [City, State, ZIP] Does Medicare require that the surgeon or the physician should also report the ASC as credentialed as place of service? -Morgan from Nebraska Medicare does have specific guidelines for reporting the place of service for both the surgeon and the Ambulatory Surgical Center (ASC). While the surgeon is not directly responsible for reporting the ASC's credentials, they must correctly report the place of service on their claim forms to ensure proper billing and reimbursement.
According to the Centers for Medicare & Medicaid Services (CMS), the place of service code for an Ambulatory Surgical Center is "24." This code should be used on professional claims submitted by the surgeon to indicate that the services were performed in an ASC setting. The ASC, on the other hand, is responsible for reporting its own credentials and meeting Medicare's requirements for participation. To ensure compliance with Medicare's regulations, it is essential for both the surgeon and the ASC to correctly report the place of service and maintain proper documentation. References:
Reader's Question: How to bill for Osteopathic Manipulative Treatment and E/M Performed on the Same Day ANSWER:
When billing for an E/M (evaluation and management) service that includes osteopathic manipulation therapy (OMT), there are a few important considerations to keep in mind. First, the E/M service must meet the criteria for the selected level of service, based on the documentation of the history, examination, and medical decision making. This may be an office visit, hospital visit, or other E/M service. Second, the OMT performed must be medically necessary and documented in the medical record. The OMT should be specifically described in the documentation, including the technique(s) used, the location(s) treated, and the response to the treatment. When billing for an E/M service with OMT, there are a few different codes that may be used, depending on the circumstances. The following codes may be used: 99201-99215 for office or other outpatient E/M services 99221-99239 for initial hospital care, subsequent hospital care, or observation care E/M services 99241-99255 for consultations E/M services In addition to the E/M code, the appropriate CPT code for the OMT performed should also be reported. These codes include: 98925 for OMT of one to two body regions 98926 for OMT of three to four body regions 98927 for OMT of five or more body regions The E/M code and OMT code should be reported on the same claim form, with the appropriate modifiers appended to indicate that they are separate and distinct services. Modifier 25 should be used with the E/M code to indicate that the E/M service was a significant and separately identifiable service from the OMT. Modifier 59 should be used with the OMT code to indicate that it was a separate and distinct service from the E/M. It is important to review the payer's specific coding and billing guidelines to ensure compliance with their policies. The Centers for Medicare & Medicaid Services (CMS) has also published guidelines on the appropriate use of modifiers and the proper billing of E/M services with OMT. Source: American Osteopathic Association. Billing and Coding for Osteopathic Manipulative Treatment. 2019. CMS Internet-Only Manual, Publication 100-04, Medicare Claims Processing Manual, Chapter 12 (available on the CMS website). Does this sound familiar? - BILLING CODING L5 DORSAL RAMUS AND S1, S2, S3 LATERAL BRANCH BLOCK When CPT code 64451 is performed from L5 to S3, it should be reported as a single unit of service regardless of the number of sacroiliac joints injected. Each sacroiliac joint should not be counted as a separate injection. This is because the injection is being performed at the sacral plexus, which is located near the sacroiliac joint but is a different structure.
This information is supported by the American Medical Association's CPT Assistant, which states that "when injection of the sacral plexus is performed at multiple levels (e.g., L4, L5, and S1), each level should be separately identified and reported with the -59 modifier appended to the additional levels beyond the first level." However, in the scenario you described, since the injection is being performed from L5 to S3, it should be reported as a single unit of service using code 64451 without any modifiers. It is important to review the payer's specific coding and billing guidelines to ensure compliance with their policies. The Centers for Medicare & Medicaid Services (CMS) has also published guidelines on the appropriate use of CPT code 64451. Source: American Medical Association. CPT Assistant. May 2013 Volume 23, Issue 5, Page 9. CMS National Correct Coding Initiative Policy Manual for Medicare Services, Chapter 11, Section H (available on the CMS website). Let's start with the PROS to why hire a Virtual Scribe? Peace of Mind: Hiring a virtual medical scribes may alleviate some pressure on the healthcare professional and the patient. A doctor or other healthcare provider may put their full attention on patient care. A hired virtual medical scribes a professional that attends patient appointments with a doctor virtually, takes detailed notes, and creates detailed records of the visit. To save up doctors' time for direct patient care, they have a "virtual medical scribe" take care of their electronic medical records and clinical charting remotely. While this is going on, the Virtual medical scribe who was hired may take down all the pertinent data. Patients will feel more at ease knowing their doctor can devote full attention to them. Increased Perception of Privacy: A hired virtual medical scribe enables the doctor and patient to have privacy throughout the exam since the scribe is listening remotely. More privacy is provided, which is particularly welcome for patients uneasy about having a third set of eyes and ears in the room. If the patient feels comfortable, they will be more forthcoming about their symptoms, aiding in diagnosis and leading to better results. Fewer People to on-board: Having fewer personnel to implement is another crucial advantage of using a hired virtual medical scribe service. To make sure the rollout of your EHR goes off without a hitch, you'll need to train almost all of your employees on how to use it. To save time and effort, you may instead employ and educate a Virtual Medical Scribe who can translate complex medical jargon into language that everyone on the team can understand. Issues with Scheduling: The schedules of the practitioner and the scribe in a 1:1 or 2:1 relationship must be coordinated. The surgeon will be on their own as long as the scribe is away from the office for vacation or sickness. This issue is resolved when a Virtual Medical Scribe is used. Face-to-Face Interaction: One of the most significant factors to weigh while weighing the benefits and drawbacks of virtual medical scribes is the amount of face-to-face time they will spend with your patients. Patients still prefer face-to-face connections with medical professionals despite the increased use of telemedicine. Computer software cannot read a patient's mood like a hired virtual medical scribe. EMR experts: Many e-health record systems are now second nature to the Virtual Medical Scribe (EMRs). This motivates the Virtual Medical Scribe to coach doctors on EMR usage and template implementation. As a bonus, a Virtual Medical Scribe who is already acquainted with the practice's EMR may help train new personnel. The hired virtual medical scribe will help ease the learning curve for the new doctor in this manner. Reduced Functional Creep: One of the most significant issues with onsite hired virtual medical scribe is the phenomenon known as "functional creep," which occurs when an employee's duties go beyond what was initially expected of them. Faithful and independent scribes may be given more challenging EHR responsibilities to accomplish while doctors concentrate on patient care. Without proper precautions, a doctor may be held legally responsible for malpractice if functional creep occurs in their practice. Fortunately, the distance between the hired virtual medical scribe and the doctor considerably reduces the functional creep danger. Several virtual scribing agencies purposefully restrict staff access to the information they need to complete medical documentation, eliminating room for functional creep. The Flexibility of Service: As they can work from anywhere, virtual scribes are an excellent option for medical facilities that are located in distant or rural areas where onsite scribes may be scarce. The scheduling challenges often associated with onsite medical scribes are mitigated by the availability of several online medical scribe services, which provide coverage on short notice for employees who are off sick or on vacation. When onsite scribes are in short supply, medical facilities in distant or rural areas might benefit significantly from the services of virtual scribes, who can work from anywhere in the world. Scheduling issues that come with employing onsite medical scribes are mitigated by many online medical scribe firms providing an on-demand covering for absences due to sickness or vacation. Reduced Intrusiveness: Since hired virtual medical scribe no longer need to physically be present in the exam room, patients report feeling more at ease throughout their appointments. According to some research, patient anxiety and reluctance to provide private information have been linked to the presence of in-person scribes. This feeling of intrusion is much mitigated when using an online scribe. Cons of hiring Virtual Medical Scribes Lack of Streamlined Workflow: It is common knowledge that we'll discover methods to automate various jobs as our technological capabilities increase. This is why many hospitals are switching to EHRs instead of continuing to use a hired virtual medical scribe. One of the major drawbacks of hiring Virtual medical scribes, in the eyes of many, is that a computer program can replace them. Each individual who has contact with a patient may share what they learn instead of relying on a central repository. This approach may compile and make data available to doctors and patients. Medical errors: The fact that hiring Virtual medical scribes is human is one of the major "cons" when weighing the benefits of using virtual medical scribes. Humans are fallible, and you want as few errors as possible to occur in the medical industry. When adding a medical scribe to the mix, there is an increased risk of information being lost in translation. Weary Patients: Finally, when weighing the benefits and drawbacks of using hired virtual medical scribe, it is important to remember that some patients may be hesitant to open up to a healthcare provider they haven't met in person. They may experience frequent anxiety when there is more than one person present. Lack of Standardized Training: While demand for scribes continues to rise, standardized training has not kept pace. Some private employment organizations require onsite and remote scribes to complete in-house training programs, but the federal government provides no oversight or guidance for these initiatives. The scribes themselves have a vast range of expertise. According to a recent survey, 22% of scribes have formal training or certification, while 44% have no such background. Band-Aiding the Larger Problem: Even though scribes often help doctors, they are essentially only a stopgap solution to the much broader documentation issue. Although scribes may help speed up the note-taking process, doctors are still responsible for entering the scribe's work into the electronic health record (EHR). It is time to reassess our strategy for assisting doctors with note-taking and recordkeeping. From the minute a patient comes through the door until the final entry in the electronic health record is entered, the insurance claim is submitted, or the medication is dispensed, our solutions must meet concerns about cost and data security. This resulted in the study's main conclusion: that different scribes recorded varied data regarding duplicate patient contacts. Possibility of stifling EHR advances: While working with scribes may benefit doctors and hospitals in the short term, in the long run, it may have the unintended consequence of slowing down advancements in electronic health record technology and perhaps putting patients in danger. Lack of oversight: It is human nature to be a little reserved when one cannot physically see the new team member. However, Virtual medical scribes are experienced professionals who thrive in quiet, self-contained workspaces where they can set their own pace. This independence and control over their working day keep them far more motivated and productive than they would be if they were forced to stick to the rules in a typical office. So this may not be the downside as thought. Lack of availability is another standard reservation: To combat this issue, it is essential to not only explain tasks clearly, give clear briefs, and lay out what the expectations about their capacity to support the will be from the very start, but also to let them know the actual hours in the day one requires them to be contactable. Virtual Medical Scribes: Understanding Telescribes and Remote Scribes Virtual Medical Scribes: Understanding Telescribes and Remote Scribes A Virtual Medical Scribe is a professional who documents the patient's encounter with the physician, irrespective of the location and time. Remote Scribing comprises of a real-time working as a writer while connected to a doctor’s office who is attending a patient or performing a simple procedure on a patient in the office. The remote scribe can view and listen to the proceedings and must meticulously enter all the relevant data into the EHR. The scribe must be well versed in medical terminology and drug names and be computer savvy to quickly enter details while the doctor is attending to the patient. Remote scribing is a growing field essential to the healthcare industry's future. Whether someone wants a new career or a place to gain experience, remote scribing presents an exciting opportunity to learn and contribute to healthcare in various ways. Scribes ease the burden on healthcare teams, help medicine progress into the electronic age, and improve patient care. With the approval of the Texas Christian University's administration, the Virtual medical scribe was invented by John Geesbreght, which led to the recruitment of pre-med TCU students for the establishment medicine. Upon invention, the Virtual or tech-enabled-remote scribes proved to offer more ROI and benefit to doctors in 2019. The innovations of the remote scribing purported to elevate the natural conversation between a doctor and a patient and decode it into structural noted in the HER as an output. Through the year of 2019, there was a high demand for a high ratio of human in the loop are required earnestly. Tele-scribing is also about the execution of simple peripheral tasks. These domains generally appeal to medical technician investors and resemble the Alexa-like workflows that consumers experience at home. In practice, these workflows did not save much time and offered doctors a lot of ROI in 2019. Further, there are a lot of workflows that are best done in expert user interfaces. For example, imagine ordering a flight ticket through a phone tree voice interface. The role of a virtual scribe determines a smooth route for physicians to assess and evaluate patients comprehensively. This is accomplished by the detailed description of clinical synopsis documented by a respective virtual scribe assigned to a certain physician. These processes are performed under high-security parameters in a HIPAA-compliant data management center and are connected to examination rooms through secure internet and VoIP connections. Only a few companies are into this at the moment across the world. The services require a lot of compliance, most importantly HIPAA, since it deals with sensitive information and exposure to the clinic setting. Telescribes is almost like a doctor's assistant but works virtually for the doctor and is connected via webcam. The work usually happens when the doctor is in session, corresponding to business hours. Given their familiarity with medical reports, Telescribes can be a good alternative for medical transcriptionist although strenuous if the partake does not have a passion in the field. While Telescribes video promotes patient-doctor privacy, it also allows a live scribe to listen to and decode the conversation from a different room through a secure and easy-to-use app on a mobile tablet. The viewer will hear the dialogue between the doctor and patient as the video shows the remote scribe documenting the visit. Tracking information from doctor visits. Scribe works as an assistant to doctors and collects lab results on patient scribes are focused on patient interaction. In this example of a clinical scenario, one will see the documentation for subjective and objective patient data, including the HPI, ROS, Physical exam (PEx), Assessment, and Plan. Through this system, a remote scribe can easily fulfill different duties such as appointment scheduling, billing, phone call reception, and another sort of inquiries. They note down all the key points, which reduces the physician's additional time spent on notes and documentation. In the clinical setting, a virtual medical scribe may have more responsibilities since the pace is slower and patients are more likely to be stable. Some of these responsibilities include reporting the quality codes mentioned earlier and putting in orders and charges, all under the physician's close supervision, of course. This provides great exposure to medical decision-making for scribes seeking experience in advanced healthcare careers. Through tele-scribing and webcam, the scribe can know and see what tests physicians order for which symptoms and the variety of treatments they provide for different ailments and conditions. However, scribes are heavily used in the emergency department in a hospital setting, although some hospitals utilize them in other areas. Medical scribes can be considered paraprofessionals, making the job easy for doctors by watching and documenting doctor-patient encounters. Currently, there are Virtual Scribes present online and work for physicians. Scribes improve documentation. While being a Virtual Medical Scribe does not require one to attain a college degree, they should be well trained in speed typing, English language, grammar, medical coding, medical conversations, listening, analytical and reasonable skills, and software navigation skill. Working remotely, a medical scribe is a clinical experience through the tele-scribing system. A medical scribe performs a wide range of transcription-related tasks. A personal assistant to the physician performs electric record-keeping responsibilities for the physicians during patient encounters, ensuring the best patient care cannot be accomplished in time. Subsequently, computer competence is also an essential skill for virtual Medical Scribe jobs. It is important not only to be able to type at an above-average speed but to do so while multitasking. The profession needs one to be able to type, listen, and take notes as the physician bounces between dialogue with the patient while giving notes and findings in various parts of the chart. Conclusively, remote scribing is the process where the words and actions of a doctor, surgeon, nurse practitioner, or other medical professional are charted and documented. Medical scribing is an organized and well-esteemed fragment of the US healthcare system; personal assistant helps the physician deliver a high-quality healthcare system. Scribing in a clinic involves a more predictable setting, although sometimes it can be just as intense as in the ER. The benefits and drawbacks of scribing in each setting depend greatly on what one is seeking. Since a Virtual medical scribe works on the documentation of patients' records, the hospital offers scribes more action in which they can promote the work of the doctor. This provides a lot of flexibility in scheduling. They must be quick and not miss out on critical data, as everything happens in real time. The ability to comprehend and good writing abilities all come in handy. Virtual Nurse RX has a team of registered nurses who can help one run a more efficient practice. The virtual scribes are a vital asset to the team by watching and listening to the patient's needs. A medical scribe is a person who assists doctors in charting prescriptions and adding data to EHR. CPT Codes to Report (based on Medical Necessity and Service(s) Performed: 63650 PERCUTANEOUS IMPLANTATION OF NEUROSTIMULATOR ELECTRODE ARRAY, EPIDURAL 63655 LAMINECTOMY FOR IMPLANTATION OF NEUROSTIMULATOR ELECTRODES, PLATE/PADDLE, EPIDURAL 63663 REVISION INCLUDING REPLACEMENT, WHEN PERFORMED, OF SPINAL NEUROSTIMULATOR ELECTRODE PERCUTANEOUS ARRAY(S), INCLUDING FLUOROSCOPY, WHEN PERFORMED 63664 REVISION INCLUDING REPLACEMENT, WHEN PERFORMED, OF SPINAL NEUROSTIMULATOR ELECTRODE PLATE/PADDLE(S) PLACED VIA LAMINOTOMY OR LAMINECTOMY, INCLUDING FLUOROSCOPY, WHEN PERFORMED 63685 INSERTION OR REPLACEMENT OF SPINAL NEUROSTIMULATOR PULSE GENERATOR OR RECEIVER, DIRECT OR INDUCTIVE COUPLING REMEMBER: to always review documentations and medical necessity when performing these services. According to CMS Utilization Guidelines: Utilization Guidelines (most commercial payers also follow this guidelines): 63650 - Two temporary spinal cord stimulator trials per anatomic spinal region (two per DOS) or (four units) per patient per lifetime (with exceptions allowed for technical limitations for the initial trials or for use of different modalities of stimulation, including new technology), in place of service office, ASC, out-patient hospital, or hospital. Since permanent neurostimulator arrays can also be placed percutaneously, code 63650 can be covered more often in place of service ASC, out-patient hospital, or hospital. 63655 - One permanent spinal cord stimulator per patient per lifetime and must be performed in an ASC, out-patient hospital or hospital. 63663 - Will not be reimbursed in the office setting since they are included in 63650. Remember: The imaging guidance is NON-BILLABLE! Common ICD-10 Codes Cross-over meeting Medical Necessity: M51.16 Intervertebral disc disorders with radiculopathy, lumbar region M51.17 Intervertebral disc disorders with radiculopathy, lumbosacral region M51.24 Other intervertebral disc displacement, thoracic region M51.25 Other intervertebral disc displacement, thoracolumbar region M51.26 Other intervertebral disc displacement, lumbar region M51.27 Other intervertebral disc displacement, lumbosacral region M54.11 Radiculopathy, occipito-atlanto-axial region M54.12 Radiculopathy, cervical region M54.13 Radiculopathy, cervicothoracic region M54.14 Radiculopathy, thoracic region M54.15 Radiculopathy, thoracolumbar region M54.16 Radiculopathy, lumbar region M54.17 Radiculopathy, lumbosacral region M54.18 Radiculopathy, sacral and sacrococcygeal region M96.1 Postlaminectomy syndrome, not elsewhere classified Medicare and Most PAYERS DO NOT reimburse for the Leads. So be careful not to report the L-Code not unless you know your payer will pay for it! Reference: https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleId=57792&ver=6 CPT CODE BOOK: 2021 and 2022 ICD-10 GUIDELINE: 2021 CPT is a Trademark and Owned by the American Medical Association SCS Vendors Useful Links: Boston Scientific Interventional Pain Management Products Medtronic Spinal Stimulation Systems NALU NeuroStimulation St. Jude Medical NeuroStimulation Systems (Abbott) This blog post provides a comprehensive guide on how to correctly bill for MILD (Minimally-Invasive Lumbar Decompression) procedures in the healthcare industry. With clear instructions and helpful tips, the post aims to assist healthcare providers in navigating the billing process, avoiding common errors, and maximizing reimbursements. Whether you are a physician, coder, or biller, this informative post from GoHealthcare Practice Solutions LLC can serve as a valuable resource for billing MILD procedures accurately and efficiently. Some of my Pain Practice Offices are still confused on how to bill for MILD Procedure. As we all remember, there was no assigned CPT Code for this procedure, we used to report the unlisted code. In this Blog, I will describe the billing and coding for this procedure using the Vertos Device (www.vertosmed.com First, let's describe what is MILD? MILD stands for MINIMALLY INVASIVE LUMBAR DECOMPRESSION. HOW TO BILL FOR MILD - MINIMALLY INVASIVE LUMBAR DECOMPRESSION CPT 0275T is a Category III Code assigned for this procedure. 0275T - Percutaneous laminotomy/laminectomy (interlaminar approach) for decompression of neural elements, (with or without ligamentous resection, discectomy, facetectomy, and/or foraminotomy), any method, under indirect image guidance (eg. fluoroscopic, CT), single or multiple levels, unilateral or bilateral; lumbar. (For percutaneous decompression of the nuleus pulposus of intervertebral disc utilizing needle based technique, use 62287) So how do you report and bill for this MILD Procedure? Billing on HCFA 1500 form? Physician Claim:
The following information has to appear and included in your claim submission:
My additional recommendation (especially for Medicare beneficiaries): Enter the "referring physician" on Box 17 the same as the "rendering physician" on Box 24J since the assessment and treatment plan is that from the "Rendering Physician". 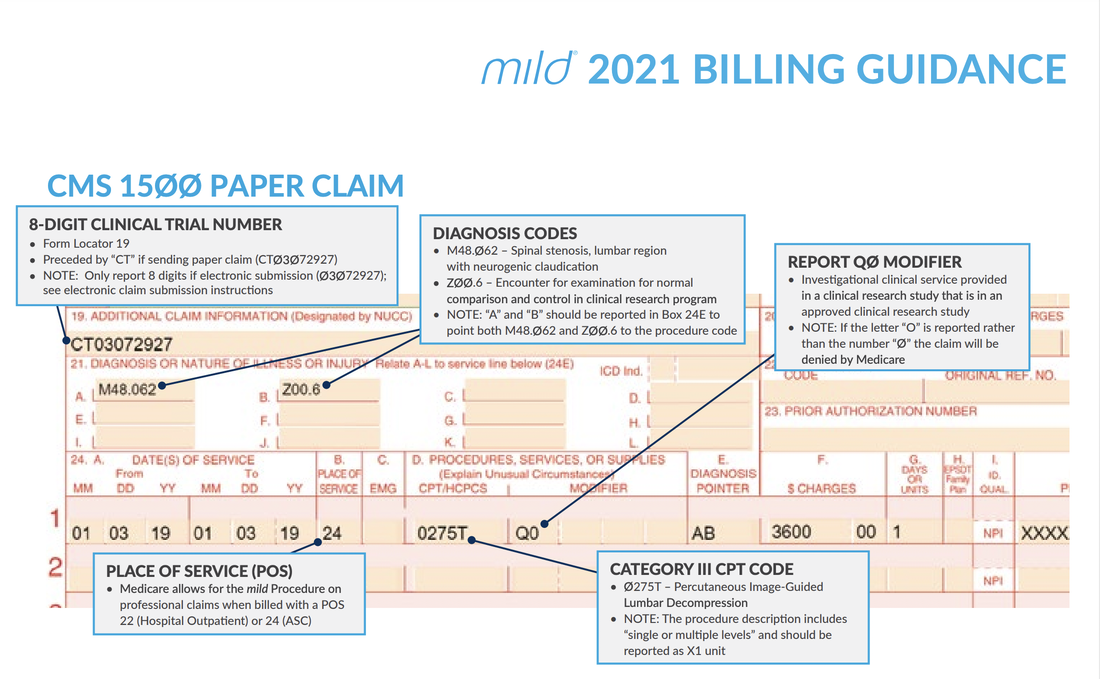 Image/Guidance Source: www.vertosmed.com Image/Guidance Source: www.vertosmed.com 2022 GUIDANCE HOW TO BILL FOR MILD - MINIMALLY INVASIVE LUMBAR DECOMPRESSION BILLING GUIDANCE for the Procedure (NCTØ3Ø72927) - SOURCE VERTOS (SEE ATTACHMENT BELOW)
Video Source is owned by: VERTOS MED - www.vertosmed.com Do you need additional help with billing?How to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers  Many physician groups or even individual solo practice offices are not happy with their contracted rates or the way they are being reimbursed by the insurance payers? Is it time to negotiate? when is the best time to negotiate your contract? There is no better time than NOW! But there are important steps that you need to do before doing so. Negotiating your contract is not only by picking up the phone and calling the insurance payer's provider services department and asking them that you would like to negotiate your contracted fees. Unfortunately, it doesn't work that way! But there are important steps that you need to do before doing so. Negotiating your contract is not only by picking up the phone and calling the insurance payer's provider services department. It doesn't work that way! Here are my tips: How to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers
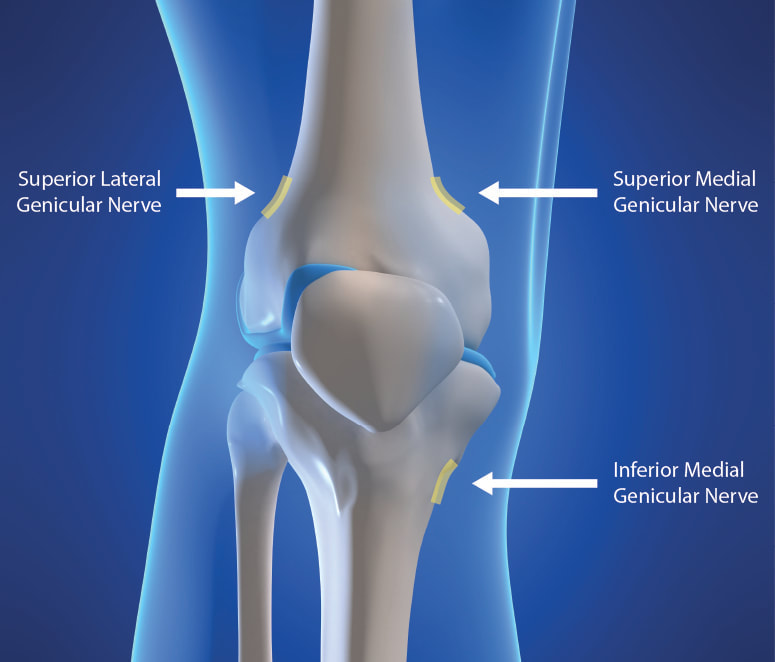
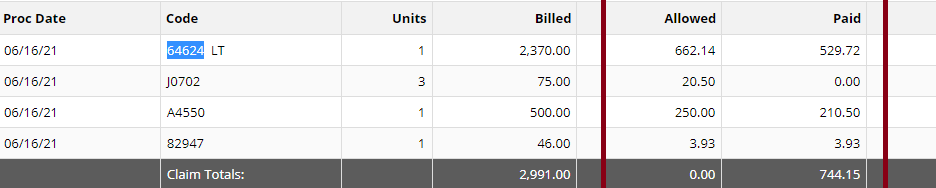
You need to present your reasoning why you think its time to negotiate your fees! All of the above, you can present it to the Insurance Payer through the Network Area Manager. Put them all together. Document everything! You can initiate the process by calling, and then by sending a formal letter of intent to renegotiate your contract rates or fee schedule. Don't forget to involve your billers and coders in this project! Let your patients leave feedback, reviews and about their experience in your practice! All these will surely help get you a better deal. It's a bit of a process but just be patient and work on it. Do you need help on how to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers? You should contact us today!Understanding the Genicular Nerves (image below)Do you remember the struggle when we didn't have the specific code for the Genicular Nerve Knee Block and for the ablation or the RFA? Prior to January 1, 2020, we used to code them using 64450 for the Peripheral Nerve Block and the you used the 64640 for the Ablation. Not only that, you need to know the nerves that were blocked or were RFA'ed. But Effective January 1, 2020, we have now a specific code for the Genicular Nerve Knee Block and the Genicular Nerve Knee Ablation. You can read more about that change in our blog. CLICK HERE. CPT 64454 Genicular Nerve Block Injection(s), anesthetic agent(s) and/or steroid; genicular nerve branches, including imaging guidance, when performed CPT 64624 Genicular Nerve Ablation or RFA Destruction by neurolytic agent, genicular nerve branches including imaging guidance, when performed Unfortunately many of our Pain and Orthopedic Physicians are still struggling getting reimbursed for these services even though we already have these specific codes in place since 2020. And why is that? There are common issues why: 1) Their billing staff are still using the old codes CPT 64450, CPT 64640 instead of the CPT Code 64454 and 64624 for the Genicular Nerve Block and Radiofrequency Ablation; 2) What I found is that, this is considered as Investigational and Experimental based on the following guideline when being reported: Genicular nerve blocks and genicular nerve ablation are considered investigational and not medically necessary for the treatment of chronic knee pain, including but not limited to any of the following:
But I have also read that there are two CMS Contractors who covers for this procedure based on Medical Necessity. See Group 1 Diagnosis Codes Cross Over: Group 1 DX Codes:
Read more about guidelines: National Government Services Inc Billing and Coding: Peripheral Nerve Blocks (A57452) First Coast Service Options, Inc Billing and Coding: Peripheral Nerve Blocks (A57788) More Guidelines from Payers which consider the procedure to be Investigational: Aetna Healthcare Anthem Blue Cross Blue Shield How do you handle Denial and Appeal for Genicular Nerve Ablation or Genicular Nerve Block? Here are my tips: Avoid the denials in the first place! by knowing your payers' guidelines; If the Provider says its Medically Necessary for the patient to receive the genicular nerve block or genicular nerve ablation, try getting a Predetermination based on Medical Necessity from your Payer! They will not allow you to submit Prior Authorization because for sure, it does not need Prior Authorization because its not a covered benefit based on their policy because the payer considers it "investigational" or "experimental"; Insist on reviewing Predetermination based on Medical Necessity instead! Already having denied claims? - pursue the claims by sending appeals, get your patient get involved with the appeals process. Be prepared with your medical documentation! How's the Patient's Pain Relief? Duration of Pain Relief? Improved ADL? - include that all in your documentation! Searched Keywords: GENICULAR NERVE BLOCK DENIAL AND APPEAL CPT BILLING CODE 64454 This is how it looks like when you get paid for Genicular Nerve Knee RFAgenicular-nerve-block-denial-and-appeal.html. Does this not look nice? HOW TO GET PAID FOR GENICULAR NERVE KNEE INJECTIONS Need help how to Appeal your claims? Contact Us today! Need help how to obtain Pre-determination before you render the Genicular Nerve Block to your patients? You should contact us today! NEW CPT Code 99072 and CPT Code 86413 DURING COVID19 PANDEMIC These 2 new CPT Codes 99072 and 86413 were published on September 8th 2020 and are effective immediately.  Let's describe these 2 new CPT Codes. CPT Code 99072 Additional supplies, materials, and clinical staff time over and above those usually included in an office visit or other non-facility service(s), when performed during a Public Health Emergency as defined by law, due to respiratory-transmitted infectious disease Take Note: This new code 99072 is reported only during a PHE (Public Health Emergency) and only for additional items required to support a safe in-person provision of evaluation, treatment, or procedural service(s). CPT Code 86413 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]) antibody, quantitative According to the AMA: "The first addition, CPT code 99072, was approved in response to sweeping measures adopted by medical practices and health care organizations to stem the spread of the novel coronavirus (SARS-CoV-2), while safely providing patients with access to high-quality care during in-person interactions with health care professionals. The additional supplies and clinical staff time to perform safety protocols described by code 99072 allow for the provision of evaluation, treatment or procedural services during a public health emergency in a setting where extra precautions are taken to ensure the safety of patients as well as health care professionals. The AMA/Specialty Society RVS Update Committee (RUC) worked with 50 national medical specialty societies and other organizations over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency and submitted recommendations today to the Centers for Medicare and Medicaid Services to inform payment of code 99072." "The second addition, CPT code 86413, was approved in response to the development of laboratory tests that provide quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) of SAR-CoV-2 antibodies provided by laboratory tests reported by other CPT codes. By measuring antibodies to SARS-CoV-2, the tests reported by 86413 can investigate a person’s adaptive immune response to the virus and help access the effectiveness of treatments used against the infection." Must be reported only once per in-person! (read more below) Code 99072 is to be reported only once per in-person patient encounter per provider identification number (PIN), regardless of the number of services rendered at that encounter. In the instance in which the noted clinical staff activities are performed by a physician or other qualified health care professional (eg, in practice environments without clinical staff or a shortage of available staff), the activity requirements of this code would be considered as having been met; however, the time spent should not be counted in any other time-based visit or service reported during the same encounter. CPT Guidelines, Q&A from the American Medical Association: Understanding PHE or Public Health Emergency in coordination with CPT Code 99072 Question: Code 99072 is stated as being applicable “during a PHE.” What information should be used to verify when a PHE is in effect? Answer: A PHE is in effect when declared by law by the officially designated relevant public health authority(ies). Understanding Patient Encounters Type for the determination of CPT Code 99072 Question: For what type of patient encounters or services should code 99072 be reported? Answer: Code 99072 may be reported with an in-person patient encounter for an office visit or other non-facility service, in which the implemented guidelines related to mitigating the transmission of the respiratory disease for which the PHE was declared are required. Use of this code is not dependent on a specific patient diagnosis. For a list of POS codes with facility/non-facility designations that are available in the Medicare Claims Processing Manual, visit https://www.cms.gov/Medicare/Coding/place-of-service-codes. Understanding Documentation Requirements when reporting CPT Code 99072 Question: What documentation is required to report code 99072? Answer: Given that code 99072 may only be reported during a PHE, one would not report this code in conjunction with an evaluation and management (E/M) service or procedure when a PHE is not in effect. Therefore, code 99072 is reported justifiably only when health and safety conditions applicable to a PHE require the type of supplies and additional clinical staff time explained in the code descriptor. Documentation requirements may vary among third-party payers and insurers; therefore, they should be contacted to determine their specifications. How about CPT Code 99072 with CPT Code 99070? Question: May code 99072 be reported with code 99070? Answer: Yes, code 99072 may be reported with code 99070 when the requirements for both codes have been met. Note that eligibility for payment, as well as coverage policy, is determined by each individual insurer or third-party payer. Reader's QUESTION - how much are you going to be reimbursed for these 2 new codes?  Reference sources: https://www.ama-assn.org/press-center/press-releases/ama-announces-new-cpt-codes-covid-19-advancements-expand https://www.ama-assn.org/system/files/2020-09/cpt-assistant-guide-coronavirus-september-2020.pdf CPT Assistant September 2020 Special Addition CPT is a trademark and owned by the American Medical Association. One of our blog readers asked why their claim for Trigger Point injection is being denied due to missing modifier. Let's describe these 2 Trigger point injection codes: 20552 Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s) 20553 Injection(s); single or multiple trigger point(s), 3 or more muscles Widely indicated for Myofascial Pain. Key point to remember! - these 2 CPT Codes 20552, 20553 DO NOT NEED A MODIFIER! Denial Reasons for Trigger Point Injection CPT 20553Denials Reasons for Trigger Point Injection CPT 20552, 20553 and what you should be looking for:
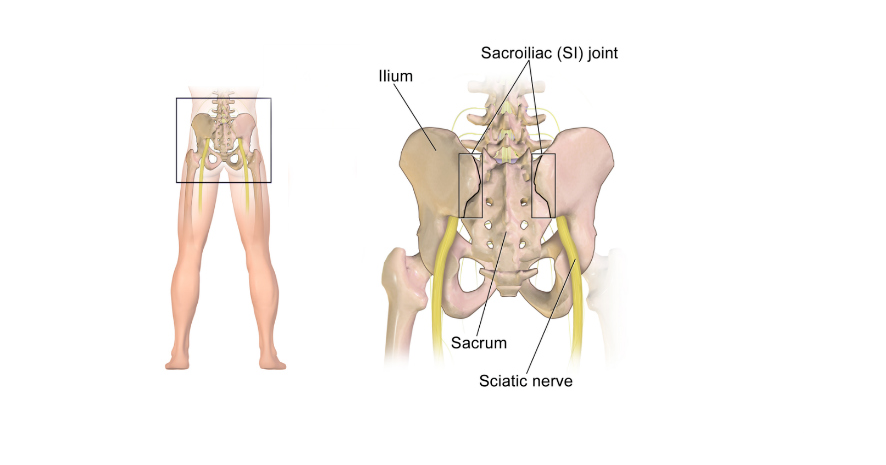
Need more help? Call us at 732-982-4800 today!January 1, 2020 - we now have a new Pain Management Code CPT 64625 - SI Ablation Description of CPT Code 64625 Radiofrequency ablation, nerves innervating the sacroiliac joint, with imaging guidance (Fluoroscopic or Computed Tomography). Keypoints to REMEMBER!
Need help? Contact our office today!Let's decribe this code: CPT 76140 Consultation on x-ray examination made elsewhere, written report. (2D reformatting is no longer separately reported. To report 3D rendering, see 76376, 76377) So the question is, can a Provider bill for X-ray review using CPT Code 76140? Sharing to you coding clarification here. (Source are from CPT Assistant as published by the AMA). CPT is a trademark and owned by the American Medical Association. CPT Assistant October 1997
Using CPT Code 76140 76140 Consultation on x-ray examination made elsewhere, written report. You would use this code when a physician's opinion or advice regarding a specific film is requested by another physician and upon examination of the film, the consulting physician renders his or her consultation (ie, or his/her opinion or advice) to the requesting physician in the form of a written report. If a patient presents to an office for a new patient visit and brings to the physician his or her medical records, including x-rays, you should not report code 76140. Although the x-rays may have been taken elsewhere, the physician does not perform a consultation as intended by code 76140. Rather, the review or re-read of the x-rays would be considered part of the face-to-face E/M service provided to the patient. Again, the E/M codes include work done before, during, or after the E/M visit. Review of x-rays is part of the E/M service. Remember, 76140 represents a consultation, in which a physician only renders an opinion or gives advice regarding the film in the form of a written report. In general, when reporting 76140, the physician is not concurrently providing an E/M face-to-face service to the patient. READER'S QUESTION: Does Medicare Cover Radiofrequency Ablation for Pain Management in New York? Here's the Coverage Information from Medicare Part BIndications:
General Procedure Requirements:
Diagnostic Facet Joint Injections
Therapeutic Injections
Thermal Medial Branch Radiofrequency Neurotomy (includes RF and microwave technologies):
Limitations of Coverage: A maximum of five (5) facet joint injection sessions inclusive of medial branch blocks, intraarticular injections, facet cyst rupture and RF ablations may be performed per year in the cervical/thoracic spine and five (5) in the lumbar spine.
Let's describe the CPT codes 64633-64636 CPT CODE 64633 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); CERVICAL OR THORACIC, SINGLE FACET JOINT CPT CODE +64634 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); CERVICAL OR THORACIC, EACH ADDITIONAL FACET JOINT (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) CPT CODE 64635 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); LUMBAR OR SACRAL, SINGLE FACET JOINT CPT CODE +64636 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); LUMBAR OR SACRAL, EACH ADDITIONAL FACET JOINT (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) Source reference: LCD ID L35936 Facet Joint Injections, Medial Branch Blocks, and Facet Joint Radiofrequency Neurotomy NGS Medicare Part B National Government Services, Inc. MAC - Part A 06101 - MAC A J - 06 Illinois National Government Services, Inc. MAC - Part B 06102 - MAC B J - 06 Illinois National Government Services, Inc. MAC - Part A 06201 - MAC A J - 06 Minnesota National Government Services, Inc. MAC - Part B 06202 - MAC B J - 06 Minnesota National Government Services, Inc. MAC - Part A 06301 - MAC A J - 06 Wisconsin National Government Services, Inc. MAC - Part B 06302 - MAC B J - 06 Wisconsin National Government Services, Inc. A and B and HHH MAC 13101 - MAC A J - K Connecticut National Government Services, Inc. A and B and HHH MAC 13102 - MAC B J - K Connecticut National Government Services, Inc. A and B and HHH MAC 13201 - MAC A J - K New York - Entire State National Government Services, Inc. A and B and HHH MAC 13202 - MAC B J - K New York - Downstate National Government Services, Inc. A and B and HHH MAC 13282 - MAC B J - K New York - Upstate National Government Services, Inc. A and B and HHH MAC 13292 - MAC B J - K New York - Queens National Government Services, Inc. A and B and HHH MAC 14111 - MAC A J - K Maine National Government Services, Inc. A and B and HHH MAC 14112 - MAC B J - K Maine National Government Services, Inc. A and B and HHH MAC 14211 - MAC A J - K Massachusetts National Government Services, Inc. A and B and HHH MAC 14212 - MAC B J - K Massachusetts National Government Services, Inc. A and B and HHH MAC 14311 - MAC A J - K New Hampshire National Government Services, Inc. A and B and HHH MAC 14312 - MAC B J - K New Hampshire National Government Services, Inc. A and B and HHH MAC 14411 - MAC A J - K Rhode Island National Government Services, Inc. A and B and HHH MAC 14412 - MAC B J - K Rhode Island National Government Services, Inc. A and B and HHH MAC 14511 - MAC A J - K Vermont National Government Services, Inc. A and B and HHH MAC 14512 - MAC B J - K Vermont How to Document radiofrequency ablation (RFA) of nerves CPT (64635, +64636) Radiofrequency ablation (RFA), also called radiofrequency neurotomy is an interventional pain management procedure that involves heating a part of a pain-transmitting nerve with a radiofrequency needle to create a heat lesion. Some of our pain physicians offices are asking the question - How to Document radiofrequency ablation (RFA) of nerves CPT (64635, +64636. What is the proper way of reporting this kind of procedure on the medical record when performed? Here's a guidance from CPT Assistant Article published on May 2020, quotes: Question: When performing radiofrequency ablation (RFA) of nerves (64635, 64636), is it necessary that the operative report documents the specific facet joints at which the RFA with imaging occurred as well as the nerves treated or denervated? Answer: Yes, RFA procedures should clearly state which nerves were ablated and which joints were treated. Codes 64635, Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); lumbar or sacral, single facet joint, and 64636, Destruction by neurolytic agent, paravertebral facet joint nerve(s), with imaging guidance (fluoroscopy or CT); lumbar or sacral, each additional facet joint (List separately in addition to code for primary procedure), are reported for each joint treated, not each nerve treated. Stating the specific nerve and the level it innervates eliminates confusion and ensures accurate reporting. Reference: CPT Assistant Published on May 2020 The World Health Organization or the WHO made a code for ICD-10 (not ICD-10-CM) which is the U07.2, COVID-19, virus not identified, intended to give the ability to capture suspected uncertain patients.
The reason you are getting errors in billing this code is that because U07.2 Covid-19, virus not identified has not been imported into ICD-10-CM (not yet) and its coming up as invalid. It is actually a valid code. So the guidance is to code the signs and/or symptoms and/or (for example) reporting ICD-10-CM Code Z20.828 - this code is a very code that we can report. Z20.828, Contact with and (suspected) exposure to other viral communicable diseases. I always suggest that if you have cases where you only see one code such as the U07.2 Covid-19, virus not identified , we need to go back the our providers and let them if they can give you a more appropriate codes based on signs and symptoms and as documented on their medical record. Can I Bill for a Bilateral Trigger Point Injection using CPT 20552-20553? The answer is NO. See reasons below: I know it has always been a challenge on how do we properly bill and code for Trigger Point Injections using 20552 and 20553. Because these codes are being reported based on the number of muscles.
Let's describe these 2 injection codes:
Many are still so confused on how to bill for Trigger Points. Here are my Coding and Billing Tips: 1. There is NO anatomical modifier; these 2 codes are not unilateral - so modifier 50, LT or RT is not applicable; 2. Code and bill based on the number of muscles (not number of injections!) 3. You can append modifier 59 if it meets the guideline and necessity 4. Possible Imaging Used (may be any of the following): 76942 Ultrasonic guidance for needle placement (eg, biopsy, aspiration, injection, localization device), imaging supervision and interpretation 77002 Fluoroscopic guidance for needle placement (eg, biopsy, aspiration, injection, localization device) (List separately in addition to code for primary procedure) 77021 Magnetic resonance guidance for needle placement (eg, for biopsy, needle aspiration, injection, or placement of localization device) radiological supervision and interpretation How to Bill for Multiple EKG Performed by the Same Physician on the Same Day You can append the Modifier 76 - same service performed on the same day by the same physician. We apply this Modifier on the second line. The first line DO NOT require a modifier. The second line of the same CPT code will be appended with modifier 76.
|

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
||||||
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985





























 RSS Feed
RSS Feed