|
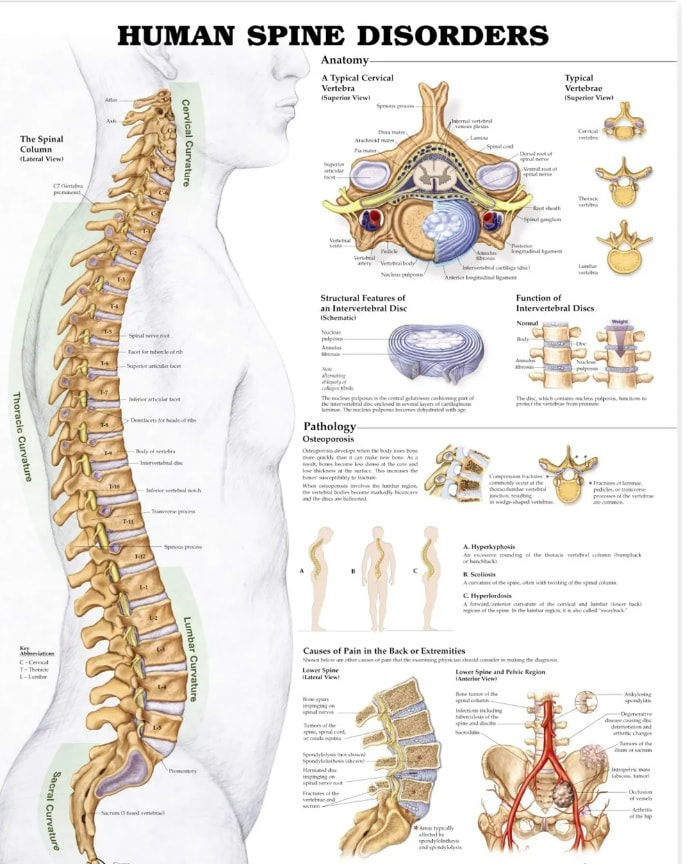
Billing and coding for Minimally Invasive Lumbar Decompression (MILD) procedures is a complex process requiring detailed understanding of procedural codes, diagnosis codes, documentation requirements, and adherence to clinical guidelines. This comprehensive guide will cover these aspects in depth, ensuring a clear understanding of the entire process. Introduction to MILD Procedures Minimally Invasive Lumbar Decompression (MILD) is a surgical technique used to treat lumbar spinal stenosis. This condition involves the narrowing of the spinal canal, which can compress nerves and lead to pain, numbness, or weakness in the lower back and legs. The MILD procedure aims to relieve this pressure with minimal tissue disruption, making it a preferred option for many patients. Billing and Coding for MILD Procedures CPT Codes for MILD Procedures The Current Procedural Terminology (CPT) codes are essential for accurately billing medical procedures. For MILD procedures, the primary CPT code is:
ICD-10 Codes for Diagnoses In addition to procedural codes, International Classification of Diseases, Tenth Revision (ICD-10) codes must be used to identify the patient’s diagnosis. Common ICD-10 codes for conditions treated with MILD procedures include:
Documentation Requirements for MILD Procedure Accurate and thorough documentation is critical for successful billing and reimbursement. The documentation should provide a clear and comprehensive picture of the patient’s condition, the necessity of the procedure, and the details of the procedure itself. Key Components of Documentation
Clinical Guidelines and Resources Adhering to clinical guidelines is essential to ensure that the MILD procedure is medically necessary and performed according to best practices. Here are some relevant guidelines and resources: Medicare Local Coverage Determinations (LCDs) Local Coverage Determinations (LCDs) are policies developed by Medicare Administrative Contractors (MACs) that provide guidance on the coverage of specific procedures. These policies can vary by region, so it’s important to refer to the LCDs applicable to the provider’s location. LCDs typically include information on covered indications, documentation requirements, and billing guidelines for the MILD procedure. National Coverage Determinations (NCDs) National Coverage Determinations (NCDs) provide national policy on whether Medicare will pay for an item or service. Although there may not be a specific NCD for the MILD procedure, general guidelines for spine surgery can be helpful. For instance, the NCD for Lumbar Spinal Fusion Surgery provides criteria that can be relevant for determining the medical necessity of procedures addressing spinal stenosis.
The ASIPP provides guidelines for interventional pain procedures, including those for lumbar spinal stenosis. These guidelines offer evidence-based recommendations on patient selection, procedural techniques, and post-procedure care. Clinical Guidelines on the Management of Lumbar Spinal Stenosis Clinical guidelines on the management of lumbar spinal stenosis offer comprehensive information on the diagnosis and treatment options for this condition. These guidelines are often developed by professional organizations and can be accessed through medical journals or databases like PubMed. Medicare and CMS Guidelines Compliance with Medicare and CMS guidelines is crucial for accurate billing and reimbursement. Providers should familiarize themselves with the following resources: CMS Manual SystemThe CMS Manual System includes the Medicare Claims Processing Manual and the Medicare Program Integrity Manual. These manuals provide detailed information on billing and coding practices, including specific instructions for surgical procedures like the MILD procedure.
The NCCI edits are designed to promote correct coding methodologies and prevent improper coding that leads to inappropriate payment. Providers should ensure that they are in compliance with these edits to avoid claim denials. Detailed Explanation of the MILD Procedure Understanding the clinical aspects of the MILD procedure helps in accurate documentation and justification of its medical necessity. Indications for MILD Procedure The primary indication for the MILD procedure is lumbar spinal stenosis causing neurogenic claudication. Patients typically present with symptoms such as:
A thorough preoperative evaluation is essential to confirm the diagnosis and assess the suitability of the patient for the MILD procedure. This includes:
The MILD procedure is performed using specialized instruments to remove small portions of bone and ligament through a tiny incision, relieving pressure on the spinal nerves. The key steps include:
Postoperative care involves monitoring the patient for complications, managing pain, and providing instructions for activity modification. Follow-up appointments are essential to assess the patient’s recovery and address any concerns. Importance of Compliance and Accurate Coding Compliance with billing and coding guidelines is not only crucial for reimbursement but also for avoiding legal and financial repercussions. Accurate coding ensures that the healthcare provider is appropriately compensated for the services rendered, while also preventing issues such as:
Challenge 1: Staying Updated with Coding ChangesCoding guidelines and reimbursement policies are subject to frequent changes. Keeping up with these changes can be challenging but is essential for compliance. Solution: Regularly subscribe to updates from professional organizations, CMS newsletters, and coding resources. Attend workshops and webinars to stay informed about the latest changes in billing and coding practices. Challenge 2: Ensuring Thorough DocumentationIncomplete or inaccurate documentation can lead to claim denials and compliance issues. Solution: Implement standardized documentation templates that include all necessary components such as patient history, imaging studies, procedural details, and post-operative care. Regular training sessions for staff on documentation best practices can also help. Challenge 3: Proper Use of CPT and ICD-10 CodesSelecting the correct CPT and ICD-10 codes for the MILD procedure and associated diagnoses is crucial for accurate billing. Solution: Use coding software and tools that assist in selecting the appropriate codes based on the documented procedure and diagnosis. Regularly review coding guidelines and ensure that coders are certified and well-trained. Challenge 4: Meeting Medical Necessity RequirementsProving medical necessity is essential for reimbursement. Insufficient evidence can result in denied claims. Solution: Ensure that the documentation includes detailed information about the patient’s condition, previous treatments, and why the MILD procedure is necessary. Adhere to clinical guidelines and payer policies when determining medical necessity. Best Practices for Successful Billing and Coding Following best practices can significantly enhance the accuracy and efficiency of billing and coding for MILD procedures. 1. Use Detailed and Clear Documentation Comprehensive documentation should include the following:
Continuous education and training for coding staff, physicians, and administrative personnel are crucial. This includes:
Utilize technology to streamline the billing and coding process:
Establish a compliance program to monitor and enforce adherence to coding and billing guidelines. This includes:
Medicare and CMS Resources Medicare and CMS offer various resources that can assist in the billing and coding process for MILD procedures. CMS Manual System The CMS Manual System includes several manuals that provide detailed information on billing and coding practices. These manuals are essential for understanding Medicare policies and ensuring compliance.
NCCI edits are designed to promote correct coding methodologies and prevent improper coding that leads to inappropriate payment. Providers should ensure compliance with these edits to avoid claim denials.
American Society of Interventional Pain Physicians (ASIPP) GuidelinesThe ASIPP provides evidence-based guidelines for interventional pain procedures, including those for lumbar spinal stenosis. These guidelines offer recommendations on patient selection, procedural techniques, and post-procedure care.
These guidelines provide comprehensive information on the diagnosis and treatment options for lumbar spinal stenosis. They are often developed by professional organizations and can be accessed through medical journals or databases like PubMed.
0 Comments
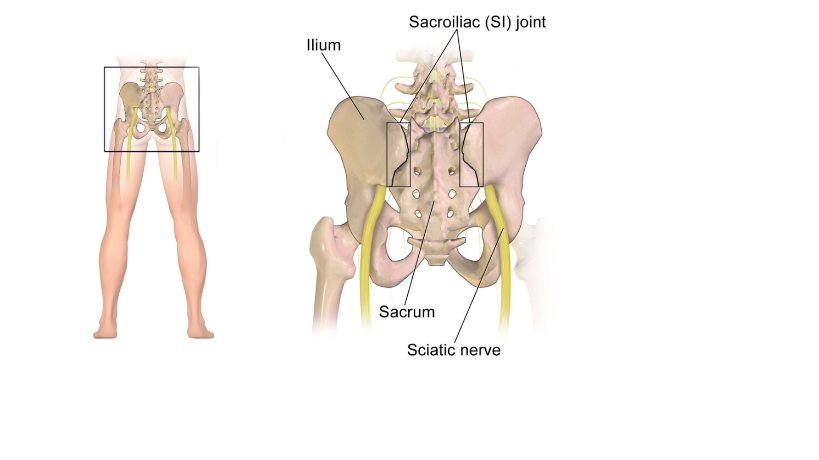
Here's a sample of a Letter of Medical Necessity for Minimally Invasive SI (SacroIliac) Joint Fusion. This is not perfect, so it is important that your Provider will spend time to review the letter. Hopefully this helps. This sample medical necessity letter outlines the benefits of Minimally-Invasive SI Joint Fusion as a treatment for chronic low back pain. It includes detailed patient history, physical examination, and imaging results to support the request for prior authorization. Written in a professional tone, this letter provides a compelling case for the minimally invasive procedure and can serve as a helpful reference for healthcare providers seeking authorization from insurance companies. Sample Letter of Medical Necessity for Minimally Invasive SI Joint Fusion[Date] [Recipient's Name] [Insurance Company Name] [Address] [City, State, ZIP Code] Patient: [Patient's Full Name] Date of Birth: [DOB] Policy Number: [Policy Number] Group Number: [Group Number] Re: Medical Necessity for Minimally-Invasive SI Joint Procedure Procedure Code: [ CPT Code ] Diagnosis Code: [ DX Code ] Dear [Recipient's Name], I am writing to request pre-authorization for a minimally-invasive sacroiliac (SI) joint procedure for my patient, [Patient's Full Name]. As the rendering physician, I have been treating [Patient's Full Name] for chronic SI joint pain and dysfunction. This letter is intended to provide you with the relevant information about [his/her/their] condition and the rationale for the proposed procedure. History: [Patient's Full Name] has been experiencing persistent lower back and buttock pain for the past [number of months/years]. The pain is particularly aggravated by activities such as prolonged sitting, standing, and walking, which has severely limited [his/her/their] ability to perform daily activities and maintain a satisfactory quality of life. [Patient's Full Name] has also reported sleep disturbances due to the pain. Physical Examination: A thorough physical examination revealed localized tenderness and pain over the SI joint, positive FABER test, and positive compression test. These findings, in conjunction with the patient's history, are consistent with SI joint dysfunction. MRI and Imaging Results: An MRI scan was performed on [Date] and confirmed the presence of SI joint inflammation and degeneration. Additional imaging, including X-rays and CT scans, also revealed irregular joint surfaces and sclerosis, which are indicative of SI joint dysfunction. Failed Conservative Treatments: [Patient's Full Name] has undergone numerous conservative treatment options without adequate relief from the symptoms. These treatments have included but are not limited to:
Based on [Patient's Full Name]'s clinical history, physical examination findings, and imaging results, it is my medical opinion that a minimally-invasive SI joint procedure is medically necessary. This procedure has a high success rate in reducing pain and improving functionality for patients with SI joint dysfunction who have failed conservative treatments. Impact on Quality of Life: [Patient's Full Name]'s chronic SI joint pain has not only affected [his/her/their] physical well-being, but also [his/her/their] emotional and mental health. The persistent pain and limited mobility have led to social isolation, increased stress levels, and feelings of depression. This procedure is crucial to help [Patient's Full Name] regain [his/her/their] quality of life and prevent further deterioration of [his/her/their] overall well-being. Minimally-Invasive Procedure Benefits: The minimally-invasive SI joint procedure offers several advantages compared to traditional open surgery. These benefits include:
Economic Impact: It is also important to consider the economic impact of [Patient's Full Name]'s chronic SI joint pain. Due to the severity of [his/her/their] condition, [Patient's Full Name] has been unable to work and maintain a consistent income. Authorizing this procedure will likely enable [Patient's Full Name] to return to work sooner, reducing the financial burden on [him/her/them] and [his/her/their] family. Minimally Invasive SI Joint Surgery: Overview and Benefits: Minimally invasive sacroiliac (SI) joint surgery, also known as SI joint fusion or stabilization, is a cutting-edge procedure that aims to alleviate pain and restore function in patients suffering from chronic SI joint dysfunction. This innovative technique has emerged as a reliable and effective treatment option for patients who have not experienced adequate relief from conservative therapies. The sacroiliac joint is the connection between the sacrum (the triangular bone at the base of the spine) and the ilium (the large, wing-shaped bone that forms the pelvis). Dysfunction in the SI joint can lead to debilitating pain and reduced mobility. Minimally invasive SI joint surgery involves the use of specialized instruments and techniques to stabilize the affected joint, thus alleviating pain and allowing the patient to regain their quality of life. Benefits of Minimally Invasive SI Joint Surgery:
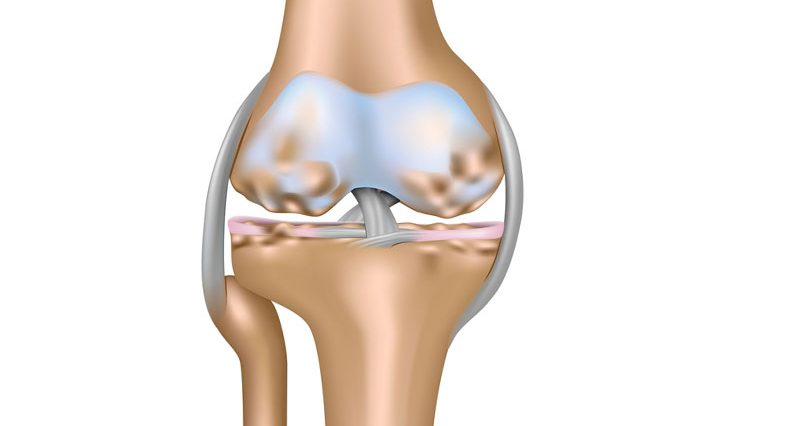
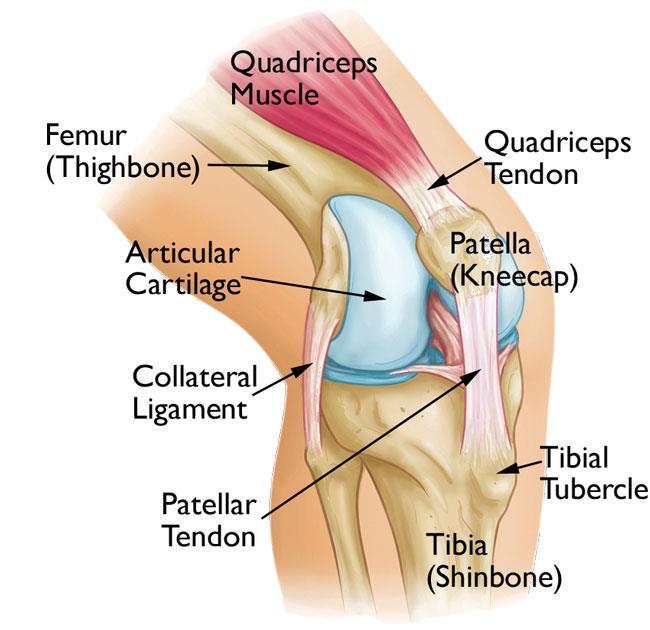
Billing Coding Knee Injection Hyalgan, Supartz, Visco, Genvisc, Synvisc - J7325, J7321, J7328 206107/13/2022 BILLING CODING KNEE INJECTION HYALGAN, SUPARTZ, VISCO, GENVISC, SYNVISC - J7325, J7321, J7328 20610 To all my blog readers that still are confused on how to properly bill, code and report these services. BILLING CODING KNEE INJECTION HYALGAN, SUPARTZ, VISCO, GENVISC, SYNVISC - J7325, J7321, J7328 20610 and more J-codes! HCPCS Code Billing Unit Drug Name(s)Dosing frequency per series (per knee) *Dose (per knee) *Units per dose (per knee) The following HCPCS codes are per dose codes: J7321 per dose Hyalgan 3 to 5 weekly injections 20 mg once weekly ( 1 unit per knee ) J7321 per dose Supartz 3 to 5 weekly injections 25 mg once weekly ( 1 unit per knee ) J7321 per dose Visco-3 3 weekly injections 25 mg once weekly ( 1 unit per knee ) J7323 per dose Euflexxa 3 weekly injections 20 mg once weekly ( 1 unit per knee ) J7324 per dose Orthovisc 3 to 4 weekly injections 30 mg once weekly ( 1 unit per knee ) J7326 per dose Gel-One Single injection** 30 mg x 1 dose ( 1 unit per knee ) J7327 per dose Monovisc Single injection** 88 mg x 1 dose ( 1 unit per knee ) HCPCS Code Billing Unit Drug Name(s)Dosing frequency per series (per knee) *Dose (per knee) *Units per dose (per knee) The following HCPCS codes are per mg codes (not per dose): J7328 per 0.1 Gelsyn-3 3 weekly injections 16.8 mg once ( 168 units per knee ) J7329 per 1 mg TriVisc 3 weekly injections 25 mg once weekly( 25 units per knee ) J7318 per 1 mg Durolane Single Injection** 60 mg x 1 dose ( 60 units per knee ) J7320 per 1 mg Genvisc 850 3 to 5 weekly injections 25 mg once weekly ( 25 units per knee ) J7325 per 1 mg Synvisc 3 weekly injections 16 mg once weekly ( 16 units per knee ) J7325 per 1 mg Synvisc-One Single injection** 48 mg x 1 dose ( 48 units per knee ) J7322 per 1 mg Hymovis 2 weekly injections 24 mg once weekly ( 24 units per knee ) J7331 per 1 mg Synojoynt 3 weekly injections 20 mg once weekly ( 20 units per knee ) J7332 per 1 mg Triluron 3 weekly injections 20 mg once weekly ( 20 units per knee ) These injections are crossing over to primary: OA (eg. M17.0) and secondary: Knee Joint Pain (M25.561, M25.562) CPT Codes: 20610 (unilateral), add 77002 if you perform under Fluoroscopy 20611 (unilateral) - if you perform under ultrasound If the injection is for Therapy. Make sure you document your notes as follows (example): 1/3 - 1st Injection 2/3 - 2nd Injection (append modifier EJ) for the drug code 3/3 - 3rd Injection (append modifier EJ) for the drug code Reference Source: https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleId=55036&ver=59
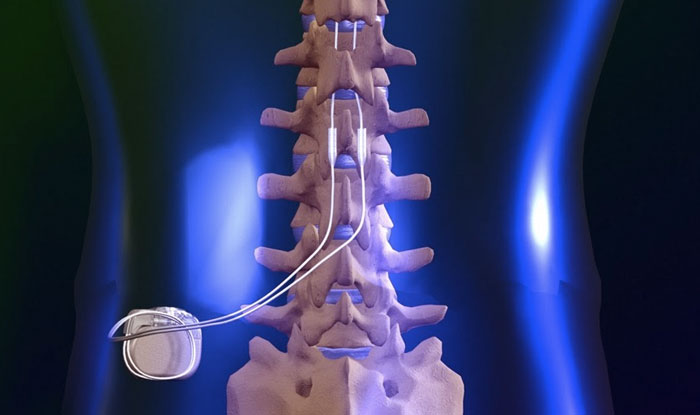
Billing and Coding: Hyaluronan Acid Therapies for Osteoarthritis of the Knee CPT 2022. CPT is a trademark and owned by the AMA - American Medical Association. CPT Codes to Report (based on Medical Necessity and Service(s) Performed: 63650 PERCUTANEOUS IMPLANTATION OF NEUROSTIMULATOR ELECTRODE ARRAY, EPIDURAL 63655 LAMINECTOMY FOR IMPLANTATION OF NEUROSTIMULATOR ELECTRODES, PLATE/PADDLE, EPIDURAL 63663 REVISION INCLUDING REPLACEMENT, WHEN PERFORMED, OF SPINAL NEUROSTIMULATOR ELECTRODE PERCUTANEOUS ARRAY(S), INCLUDING FLUOROSCOPY, WHEN PERFORMED 63664 REVISION INCLUDING REPLACEMENT, WHEN PERFORMED, OF SPINAL NEUROSTIMULATOR ELECTRODE PLATE/PADDLE(S) PLACED VIA LAMINOTOMY OR LAMINECTOMY, INCLUDING FLUOROSCOPY, WHEN PERFORMED 63685 INSERTION OR REPLACEMENT OF SPINAL NEUROSTIMULATOR PULSE GENERATOR OR RECEIVER, DIRECT OR INDUCTIVE COUPLING REMEMBER: to always review documentations and medical necessity when performing these services. According to CMS Utilization Guidelines: Utilization Guidelines (most commercial payers also follow this guidelines): 63650 - Two temporary spinal cord stimulator trials per anatomic spinal region (two per DOS) or (four units) per patient per lifetime (with exceptions allowed for technical limitations for the initial trials or for use of different modalities of stimulation, including new technology), in place of service office, ASC, out-patient hospital, or hospital. Since permanent neurostimulator arrays can also be placed percutaneously, code 63650 can be covered more often in place of service ASC, out-patient hospital, or hospital. 63655 - One permanent spinal cord stimulator per patient per lifetime and must be performed in an ASC, out-patient hospital or hospital. 63663 - Will not be reimbursed in the office setting since they are included in 63650. Remember: The imaging guidance is NON-BILLABLE! Common ICD-10 Codes Cross-over meeting Medical Necessity: M51.16 Intervertebral disc disorders with radiculopathy, lumbar region M51.17 Intervertebral disc disorders with radiculopathy, lumbosacral region M51.24 Other intervertebral disc displacement, thoracic region M51.25 Other intervertebral disc displacement, thoracolumbar region M51.26 Other intervertebral disc displacement, lumbar region M51.27 Other intervertebral disc displacement, lumbosacral region M54.11 Radiculopathy, occipito-atlanto-axial region M54.12 Radiculopathy, cervical region M54.13 Radiculopathy, cervicothoracic region M54.14 Radiculopathy, thoracic region M54.15 Radiculopathy, thoracolumbar region M54.16 Radiculopathy, lumbar region M54.17 Radiculopathy, lumbosacral region M54.18 Radiculopathy, sacral and sacrococcygeal region M96.1 Postlaminectomy syndrome, not elsewhere classified Medicare and Most PAYERS DO NOT reimburse for the Leads. So be careful not to report the L-Code not unless you know your payer will pay for it! Reference: https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleId=57792&ver=6 CPT CODE BOOK: 2021 and 2022 ICD-10 GUIDELINE: 2021 CPT is a Trademark and Owned by the American Medical Association SCS Vendors Useful Links: Boston Scientific Interventional Pain Management Products Medtronic Spinal Stimulation Systems NALU NeuroStimulation St. Jude Medical NeuroStimulation Systems (Abbott) CPT CODES for NERVE BLOCK INDICATED FOR CHRONIC PAIN MANAGEMENT (SEE LIST BELOW) 62281 INJECTION/INFUSION OF NEUROLYTIC SUBSTANCE (EG, ALCOHOL, PHENOL, ICED SALINE SOLUTIONS), WITH OR WITHOUT OTHER THERAPEUTIC SUBSTANCE; EPIDURAL, CERVICAL OR THORACIC 62320 INJECTION(S), OF DIAGNOSTIC OR THERAPEUTIC SUBSTANCE(S) (EG, ANESTHETIC, ANTISPASMODIC, OPIOID, STEROID, OTHER SOLUTION), NOT INCLUDING NEUROLYTIC SUBSTANCES, INCLUDING NEEDLE OR CATHETER PLACEMENT, INTERLAMINAR EPIDURAL OR SUBARACHNOID, CERVICAL OR THORACIC; WITHOUT IMAGING GUIDANCE 62321 INJECTION(S), OF DIAGNOSTIC OR THERAPEUTIC SUBSTANCE(S) (EG, ANESTHETIC, ANTISPASMODIC, OPIOID, STEROID, OTHER SOLUTION), NOT INCLUDING NEUROLYTIC SUBSTANCES, INCLUDING NEEDLE OR CATHETER PLACEMENT, INTERLAMINAR EPIDURAL OR SUBARACHNOID, CERVICAL OR THORACIC; WITH IMAGING GUIDANCE (IE, FLUOROSCOPY OR CT) 62324 INJECTION(S), INCLUDING INDWELLING CATHETER PLACEMENT, CONTINUOUS INFUSION OR INTERMITTENT BOLUS, OF DIAGNOSTIC OR THERAPEUTIC SUBSTANCE(S) (EG, ANESTHETIC, ANTISPASMODIC, OPIOID, STEROID, OTHER SOLUTION), NOT INCLUDING NEUROLYTIC SUBSTANCES, INTERLAMINAR EPIDURAL OR SUBARACHNOID, CERVICAL OR THORACIC; WITHOUT IMAGING GUIDANCE 62325 INJECTION(S), INCLUDING INDWELLING CATHETER PLACEMENT, CONTINUOUS INFUSION OR INTERMITTENT BOLUS, OF DIAGNOSTIC OR THERAPEUTIC SUBSTANCE(S) (EG, ANESTHETIC, ANTISPASMODIC, OPIOID, STEROID, OTHER SOLUTION), NOT INCLUDING NEUROLYTIC SUBSTANCES, INTERLAMINAR EPIDURAL OR SUBARACHNOID, CERVICAL OR THORACIC; WITH IMAGING GUIDANCE (IE, FLUOROSCOPY OR CT) Do not report the imaging separately if the description says "with imaging guidance (i.e. Fluoroscopy or CT). Do not separate the code with any modifier, it won't work! you will not get paid and its non-compliant for lack of medical necessity! 64405 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; GREATER OCCIPITAL NERVE 64408 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; VAGUS NERVE 64415 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; BRACHIAL PLEXUS 64417 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; AXILLARY NERVE 64418 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; SUPRASCAPULAR NERVE 64420 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; INTERCOSTAL NERVE, SINGLE LEVEL 64421 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; INTERCOSTAL NERVE, EACH ADDITIONAL LEVEL (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64425 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; ILIOINGUINAL, ILIOHYPOGASTRIC NERVES 64430 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; PUDENDAL NERVE 64435 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; PARACERVICAL (UTERINE) NERVE 64445 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; SCIATIC NERVE 64446 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; SCIATIC NERVE, CONTINUOUS INFUSION BY CATHETER (INCLUDING CATHETER PLACEMENT) 64447 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; FEMORAL NERVE 64448 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; FEMORAL NERVE, CONTINUOUS INFUSION BY CATHETER (INCLUDING CATHETER PLACEMENT) 64449 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; LUMBAR PLEXUS, POSTERIOR APPROACH, CONTINUOUS INFUSION BY CATHETER (INCLUDING CATHETER PLACEMENT) Reader's Question: How do I code and Bill for Cluneal Nerve Block and Cluneal Nerve Ablation or RFA? According to the AMA, the code series for medial branch blocks and the facet joint injections are the same (i.e., CPT series 64490-64495), with reporting based on the number of facet joints injected, not the number of nerves injected. For example: If three (3) medial branch nerves are injected only two (2) facet joint injection codes would be reported despite the fact that three nerves were injected, since each facet joint is connected to two medial nerves. The lateral branch nerve is a peripheral nerve and would be reported with CPT code 64450, Injection, anesthetic agent; other peripheral nerve or branch, when a lateral branch / peripheral nerve block is performed. So therefore, since the Cluneal Nerve are considered Lateral, Peripheral Nerves – it is just appropriate to assign CPT Code 64450 when blocking these nerves and CPT Code 64640 for the Destruction. 64450 INJECTION, ANESTHETIC AGENT; OTHER PERIPHERAL NERVE OR BRANCH 64640 DESTRUCTION BY NEUROLYTIC AGENT; OTHER PERIPHERAL NERVE OR BRANCH CPT code 64450 should only be reported per nerve or branch and not per injection. Make sure you read your Physician’s Op-report.Documentation must clearly indicate the nerve injected and the substance administered. Guidance: 76942 ULTRASONIC GUIDANCE FOR NEEDLE PLACEMENT (EG, BIOPSY, ASPIRATION, INJECTION, LOCALIZATION DEVICE), IMAGING SUPERVISION AND INTERPRETATION How about the Fluoroscopic Guidance? Can you bill for the CPT Code 77002? – NO. The CPT Code 77002 is now an ADD-On code per AMA’s CPT Guideline. There are codes that you can only bill with CPT 77002. According to the AMA CPT: CPT Code 77002 – Fluoroscopic guidance for needle place (eg. biopsy, aspiration, injection, localization device) (List separately in addition to code for Primary Procedure). (See appropriate Surgical Code for Procedure and Anatomic Location) Use 77002 as an “add-on” code with 10022, 10160, 20206, 20220, 20225, 20520, 20525, 20526, 20550, 20551, 20552, 20553, 20555, 20600, 20605, 20610, 20612, 20615, 21116, 21550, 23350. 24220, 25246, 27093, 27095, 27370, 27648, 32400, 32405, 32553, 36002, 38220, 38221, 38505, 38794, 41019, 42400, 42405, 47000, 47001, 48102, 49180, 49411, 50200, 50390, 51100, 51101, 51102, 55700, 55876, 60100, 62268, 62269, 64505, 64508, 64600, 64505) The cluneal nerves are sensory, not motor, and are divided into three lateral branches: inferior, medial, and superior (see below) 64450 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; OTHER PERIPHERAL NERVE OR BRANCH 64451 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; NERVES INNERVATING THE SACROILIAC JOINT, WITH IMAGE GUIDANCE (IE, FLUOROSCOPY OR COMPUTED TOMOGRAPHY) 64461 PARAVERTEBRAL BLOCK (PVB) (PARASPINOUS BLOCK), THORACIC; SINGLE INJECTION SITE (INCLUDES IMAGING GUIDANCE, WHEN PERFORMED) 64462 PARAVERTEBRAL BLOCK (PVB) (PARASPINOUS BLOCK), THORACIC; SECOND AND ANY ADDITIONAL INJECTION SITE(S) (INCLUDES IMAGING GUIDANCE, WHEN PERFORMED) (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64463 PARAVERTEBRAL BLOCK (PVB) (PARASPINOUS BLOCK), THORACIC; CONTINUOUS INFUSION BY CATHETER (INCLUDES IMAGING GUIDANCE, WHEN PERFORMED) 64479 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; TRANSFORAMINAL EPIDURAL, WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT), CERVICAL OR THORACIC, SINGLE LEVEL 64480 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; TRANSFORAMINAL EPIDURAL, WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT), CERVICAL OR THORACIC, EACH ADDITIONAL LEVEL (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64505 INJECTION, ANESTHETIC AGENT; SPHENOPALATINE GANGLION 64510 INJECTION, ANESTHETIC AGENT; STELLATE GANGLION (CERVICAL SYMPATHETIC) 64517 INJECTION, ANESTHETIC AGENT; SUPERIOR HYPOGASTRIC PLEXUS 64520 INJECTION, ANESTHETIC AGENT; LUMBAR OR THORACIC (PARAVERTEBRAL SYMPATHETIC) 64530 INJECTION, ANESTHETIC AGENT; CELIAC PLEXUS, WITH OR WITHOUT RADIOLOGIC MONITORING 64620 DESTRUCTION BY NEUROLYTIC AGENT, INTERCOSTAL NERVE 64640 DESTRUCTION BY NEUROLYTIC AGENT; OTHER PERIPHERAL NERVE OR BRANCH Sharing to you all pain management billing codes we have been utilizing helping our pain practice offices, surgery centers and our physicians clients! Let me know if you have any questions, concerns or confusion on how to report these codes properly. We have been in this world of Pain Management Practice Operations and Documentation for more than 20 years! The truth is, Pain Management billing codes are not easy to utilize if you don't know how to use them. It is always useful that you understand your physicians documentations and their procedures. Most of these codes are unilateral. Most of these codes are based on utilization and frequency guidance. So make sure you know all your payers guidelines for clinical and reimbursement. Let me know if you need me! But here are you codes! Epidural Steroid Injections for Pain Management Billing Codes: 62321 INJECTION(S), OF DIAGNOSTIC OR THERAPEUTIC SUBSTANCE(S) (EG, ANESTHETIC, ANTISPASMODIC, OPIOID, STEROID, OTHER SOLUTION), NOT INCLUDING NEUROLYTIC SUBSTANCES, INCLUDING NEEDLE OR CATHETER PLACEMENT, INTERLAMINAR EPIDURAL OR SUBARACHNOID, CERVICAL OR THORACIC; WITH IMAGING GUIDANCE (IE, FLUOROSCOPY OR CT) 62323 INJECTION(S), OF DIAGNOSTIC OR THERAPEUTIC SUBSTANCE(S) (EG, ANESTHETIC, ANTISPASMODIC, OPIOID, STEROID, OTHER SOLUTION), NOT INCLUDING NEUROLYTIC SUBSTANCES, INCLUDING NEEDLE OR CATHETER PLACEMENT, INTERLAMINAR EPIDURAL OR SUBARACHNOID, LUMBAR OR SACRAL (CAUDAL); WITH IMAGING GUIDANCE (IE, FLUOROSCOPY OR CT) Epidural Steroid Injections for Pain Management Billing Codes: 64479 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; TRANSFORAMINAL EPIDURAL, WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT), CERVICAL OR THORACIC, SINGLE LEVEL +64480 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; TRANSFORAMINAL EPIDURAL, WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT), CERVICAL OR THORACIC, EACH ADDITIONAL LEVEL (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64483 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; TRANSFORAMINAL EPIDURAL, WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT), LUMBAR OR SACRAL, SINGLE LEVEL +64484 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; TRANSFORAMINAL EPIDURAL, WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT), LUMBAR OR SACRAL, EACH ADDITIONAL LEVEL (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) Facet Joint Injections and Medial Branch Blocks Pain Management Billing Codes 64490 INJECTION(S), DIAGNOSTIC OR THERAPEUTIC AGENT, PARAVERTEBRAL FACET (ZYGAPOPHYSEAL) JOINT (OR NERVES INNERVATING THAT JOINT) WITH IMAGE GUIDANCE (FLUOROSCOPY OR CT), CERVICAL OR THORACIC; SINGLE LEVEL +64491 INJECTION(S), DIAGNOSTIC OR THERAPEUTIC AGENT, PARAVERTEBRAL FACET (ZYGAPOPHYSEAL) JOINT (OR NERVES INNERVATING THAT JOINT) WITH IMAGE GUIDANCE (FLUOROSCOPY OR CT), CERVICAL OR THORACIC; SECOND LEVEL (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) +64492 INJECTION(S), DIAGNOSTIC OR THERAPEUTIC AGENT, PARAVERTEBRAL FACET (ZYGAPOPHYSEAL) JOINT (OR NERVES INNERVATING THAT JOINT) WITH IMAGE GUIDANCE (FLUOROSCOPY OR CT), CERVICAL OR THORACIC; THIRD AND ANY ADDITIONAL LEVEL(S) (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64493 INJECTION(S), DIAGNOSTIC OR THERAPEUTIC AGENT, PARAVERTEBRAL FACET (ZYGAPOPHYSEAL) JOINT (OR NERVES INNERVATING THAT JOINT) WITH IMAGE GUIDANCE (FLUOROSCOPY OR CT), LUMBAR OR SACRAL; SINGLE LEVEL +64494 INJECTION(S), DIAGNOSTIC OR THERAPEUTIC AGENT, PARAVERTEBRAL FACET (ZYGAPOPHYSEAL) JOINT (OR NERVES INNERVATING THAT JOINT) WITH IMAGE GUIDANCE (FLUOROSCOPY OR CT), LUMBAR OR SACRAL; SECOND LEVEL (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) +64495 INJECTION(S), DIAGNOSTIC OR THERAPEUTIC AGENT, PARAVERTEBRAL FACET (ZYGAPOPHYSEAL) JOINT (OR NERVES INNERVATING THAT JOINT) WITH IMAGE GUIDANCE (FLUOROSCOPY OR CT), LUMBAR OR SACRAL; THIRD AND ANY ADDITIONAL LEVEL(S) (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) Facet Joint Radiofrequency Neurotomy Pain Management Billing Codes 64633 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); CERVICAL OR THORACIC, SINGLE FACET JOINT +64634 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); CERVICAL OR THORACIC, EACH ADDITIONAL FACET JOINT (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64635 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); LUMBAR OR SACRAL, SINGLE FACET JOINT +64636 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); LUMBAR OR SACRAL, EACH ADDITIONAL FACET JOINT (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) Peripheral Nerve Blocks Pain Management Billing Codes 64400 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; TRIGEMINAL NERVE, EACH BRANCH (IE, OPHTHALMIC, MAXILLARY, MANDIBULAR) 64405 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; GREATER OCCIPITAL NERVE 64415 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; BRACHIAL PLEXUS 64416 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; BRACHIAL PLEXUS, CONTINUOUS INFUSION BY CATHETER (INCLUDING CATHETER PLACEMENT) 64417 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; AXILLARY NERVE 64418 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; SUPRASCAPULAR NERVE 64420 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; INTERCOSTAL NERVE, SINGLE LEVEL +64421 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; INTERCOSTAL NERVE, EACH ADDITIONAL LEVEL (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64425 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; ILIOINGUINAL, ILIOHYPOGASTRIC NERVES 64430 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; PUDENDAL NERVE 64445 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; SCIATIC NERVE 64446 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; SCIATIC NERVE, CONTINUOUS INFUSION BY CATHETER (INCLUDING CATHETER PLACEMENT) 64447 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; FEMORAL NERVE 64448 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; FEMORAL NERVE, CONTINUOUS INFUSION BY CATHETER (INCLUDING CATHETER PLACEMENT) 64449 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; LUMBAR PLEXUS, POSTERIOR APPROACH, CONTINUOUS INFUSION BY CATHETER (INCLUDING CATHETER PLACEMENT) 64450 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; OTHER PERIPHERAL NERVE OR BRANCH 64454 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; GENICULAR NERVE BRANCHES, INCLUDING IMAGING GUIDANCE, WHEN PERFORMED 64455 INJECTION(S), ANESTHETIC AGENT(S) AND/OR STEROID; PLANTAR COMMON DIGITAL NERVE(S) (EG, MORTON'S NEUROMA) 64624 DESTRUCTION BY NEUROLYTIC AGENT, GENICULAR NERVE BRANCHES INCLUDING IMAGING GUIDANCE, WHEN PERFORMED 64620 DESTRUCTION BY NEUROLYTIC AGENT, INTERCOSTAL NERVE 64640 DESTRUCTION BY NEUROLYTIC AGENT; OTHER PERIPHERAL NERVE OR BRANCH 64999 UNLISTED PROCEDURE, NERVOUS SYSTEM Related Imaging Pain Management Billing Codes: 76881 ULTRASOUND, COMPLETE JOINT (IE, JOINT SPACE AND PERI-ARTICULAR SOFT-TISSUE STRUCTURES), REAL-TIME WITH IMAGE DOCUMENTATION 76882 ULTRASOUND, LIMITED, JOINT OR OTHER NONVASCULAR EXTREMITY STRUCTURE(S) (EG, JOINT SPACE, PERI-ARTICULAR TENDON[S], MUSCLE[S], NERVE[S], OTHER SOFT-TISSUE STRUCTURE[S], OR SOFT-TISSUE MASS[ES]), REAL-TIME WITH IMAGE DOCUMENTATION 76942 ULTRASONIC GUIDANCE FOR NEEDLE PLACEMENT (EG, BIOPSY, ASPIRATION, INJECTION, LOCALIZATION DEVICE), IMAGING SUPERVISION AND INTERPRETATION 76999 UNLISTED ULTRASOUND PROCEDURE (EG, DIAGNOSTIC, INTERVENTIONAL) 97032 APPLICATION OF A MODALITY TO 1 OR MORE AREAS; ELECTRICAL STIMULATION (MANUAL), EACH 15 MINUTES 97139 UNLISTED THERAPEUTIC PROCEDURE (SPECIFY) G0282 ELECTRICAL STIMULATION, (UNATTENDED), TO ONE OR MORE AREAS, FOR WOUND CARE OTHER THAN DESCRIBED IN G0281 G0283 ELECTRICAL STIMULATION (UNATTENDED), TO ONE OR MORE AREAS FOR INDICATION(S) OTHER THAN WOUND CARE, AS PART OF A THERAPY PLAN OF CARE Pain Management Billing Codes for Spinal Cord Stimulators for Chronic Pain 63650 PERCUTANEOUS IMPLANTATION OF NEUROSTIMULATOR ELECTRODE ARRAY, EPIDURAL 63655 LAMINECTOMY FOR IMPLANTATION OF NEUROSTIMULATOR ELECTRODES, PLATE/PADDLE, EPIDURAL 63663 REVISION INCLUDING REPLACEMENT, WHEN PERFORMED, OF SPINAL NEUROSTIMULATOR ELECTRODE PERCUTANEOUS ARRAY(S), INCLUDING FLUOROSCOPY, WHEN PERFORMED 63664 REVISION INCLUDING REPLACEMENT, WHEN PERFORMED, OF SPINAL NEUROSTIMULATOR ELECTRODE PLATE/PADDLE(S) PLACED VIA LAMINOTOMY OR LAMINECTOMY, INCLUDING FLUOROSCOPY, WHEN PERFORMED 63685 INSERTION OR REPLACEMENT OF SPINAL NEUROSTIMULATOR PULSE GENERATOR OR RECEIVER, DIRECT OR INDUCTIVE COUPLING Pay Attention to Medicare's Utilization Guidelines. This is also being utilized by most payers! 63650 - Two temporary spinal cord stimulator trials per anatomic spinal region (two per DOS) or (four units) per patient per lifetime (with exceptions allowed for technical limitations for the initial trials or for use of different modalities of stimulation, including new technology), in place of service office, ASC, out-patient hospital, or hospital. Since permanent neurostimulator arrays can also be placed percutaneously, code 63650 can be covered more often in place of service ASC, out-patient hospital, or hospital. 63655 - One permanent spinal cord stimulator per patient per lifetime and must be performed in an ASC, out-patient hospital or hospital. 63663 - Will not be reimbursed in the office setting since they are included in 63650. Pain Management Billing Codes for Kyphoplasty and Vertebroplasty 22510 PERCUTANEOUS VERTEBROPLASTY (BONE BIOPSY INCLUDED WHEN PERFORMED), 1 VERTEBRAL BODY, UNILATERAL OR BILATERAL INJECTION, INCLUSIVE OF ALL IMAGING GUIDANCE; CERVICOTHORACIC 22511 PERCUTANEOUS VERTEBROPLASTY (BONE BIOPSY INCLUDED WHEN PERFORMED), 1 VERTEBRAL BODY, UNILATERAL OR BILATERAL INJECTION, INCLUSIVE OF ALL IMAGING GUIDANCE; LUMBOSACRAL +22512 PERCUTANEOUS VERTEBROPLASTY (BONE BIOPSY INCLUDED WHEN PERFORMED), 1 VERTEBRAL BODY, UNILATERAL OR BILATERAL INJECTION, INCLUSIVE OF ALL IMAGING GUIDANCE; EACH ADDITIONAL CERVICOTHORACIC OR LUMBOSACRAL VERTEBRAL BODY (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 22513 PERCUTANEOUS VERTEBRAL AUGMENTATION, INCLUDING CAVITY CREATION (FRACTURE REDUCTION AND BONE BIOPSY INCLUDED WHEN PERFORMED) USING MECHANICAL DEVICE (EG, KYPHOPLASTY), 1 VERTEBRAL BODY, UNILATERAL OR BILATERAL CANNULATION, INCLUSIVE OF ALL IMAGING GUIDANCE; THORACIC 22514 PERCUTANEOUS VERTEBRAL AUGMENTATION, INCLUDING CAVITY CREATION (FRACTURE REDUCTION AND BONE BIOPSY INCLUDED WHEN PERFORMED) USING MECHANICAL DEVICE (EG, KYPHOPLASTY), 1 VERTEBRAL BODY, UNILATERAL OR BILATERAL CANNULATION, INCLUSIVE OF ALL IMAGING GUIDANCE; LUMBAR +22515 PERCUTANEOUS VERTEBRAL AUGMENTATION, INCLUDING CAVITY CREATION (FRACTURE REDUCTION AND BONE BIOPSY INCLUDED WHEN PERFORMED) USING MECHANICAL DEVICE (EG, KYPHOPLASTY), 1 VERTEBRAL BODY, UNILATERAL OR BILATERAL CANNULATION, INCLUSIVE OF ALL IMAGING GUIDANCE; EACH ADDITIONAL THORACIC OR LUMBAR VERTEBRAL BODY (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) Botox and ChemoDenervation Pain Management Billing Codes 64612 CHEMODENERVATION OF MUSCLE(S); MUSCLE(S) INNERVATED BY FACIAL NERVE, UNILATERAL (EG, FOR BLEPHAROSPASM, HEMIFACIAL SPASM)
64615 CHEMODENERVATION OF MUSCLE(S); MUSCLE(S) INNERVATED BY FACIAL, TRIGEMINAL, CERVICAL SPINAL AND ACCESSORY NERVES, BILATERAL (EG, FOR CHRONIC MIGRAINE) 64616 CHEMODENERVATION OF MUSCLE(S); NECK MUSCLE(S), EXCLUDING MUSCLES OF THE LARYNX, UNILATERAL (EG, FOR CERVICAL DYSTONIA, SPASMODIC TORTICOLLIS) 64617 CHEMODENERVATION OF MUSCLE(S); LARYNX, UNILATERAL, PERCUTANEOUS (EG, FOR SPASMODIC DYSPHONIA), INCLUDES GUIDANCE BY NEEDLE ELECTROMYOGRAPHY, WHEN PERFORMED 64640 DESTRUCTION BY NEUROLYTIC AGENT; OTHER PERIPHERAL NERVE OR BRANCH 64642 CHEMODENERVATION OF ONE EXTREMITY; 1-4 MUSCLE(S) 64643 CHEMODENERVATION OF ONE EXTREMITY; EACH ADDITIONAL EXTREMITY, 1-4 MUSCLE(S) (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64644 CHEMODENERVATION OF ONE EXTREMITY; 5 OR MORE MUSCLES 64645 CHEMODENERVATION OF ONE EXTREMITY; EACH ADDITIONAL EXTREMITY, 5 OR MORE MUSCLES (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) 64646 CHEMODENERVATION OF TRUNK MUSCLE(S); 1-5 MUSCLE(S) 64647 CHEMODENERVATION OF TRUNK MUSCLE(S); 6 OR MORE MUSCLES HCPCS Pain Management Billing Codes for Botox and Chemodenervation J0585 INJECTION, ONABOTULINUMTOXINA, 1 UNIT J0586 INJECTION, ABOBOTULINUMTOXINA, 5 UNITS J0587 INJECTION, RIMABOTULINUMTOXINB, 100 UNITS J0588 INJECTION, INCOBOTULINUMTOXIN A, 1 UNIT What is CPT Code 64451? This is for the Block 64451, Injection(s), anesthetic agent(s) and/or steroid; nerves innervating the sacroiliac joint, with image guidance (ie, fluoroscopy or CT computed tomography), should be reported once for this procedure. The fluoroscopic guidance should not be separately reported as it is included in the work described with code 64451.
When you do your RFA or Radio Frequency Ablation, what CPT Code do you need to use? Read below: CPT CODE FOR SACROILIAC SI RFA FOR 2020 CPT 64625 January 1, 2020 - we now have a new Pain Management Code CPT 64625 - SI Ablation Description of CPT Code 64625 Radiofrequency ablation, nerves innervating the sacroiliac joint, with imaging guidance (Fluoroscopic or Computed Tomography). Keypoints to REMEMBER!
|

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985











 RSS Feed
RSS Feed