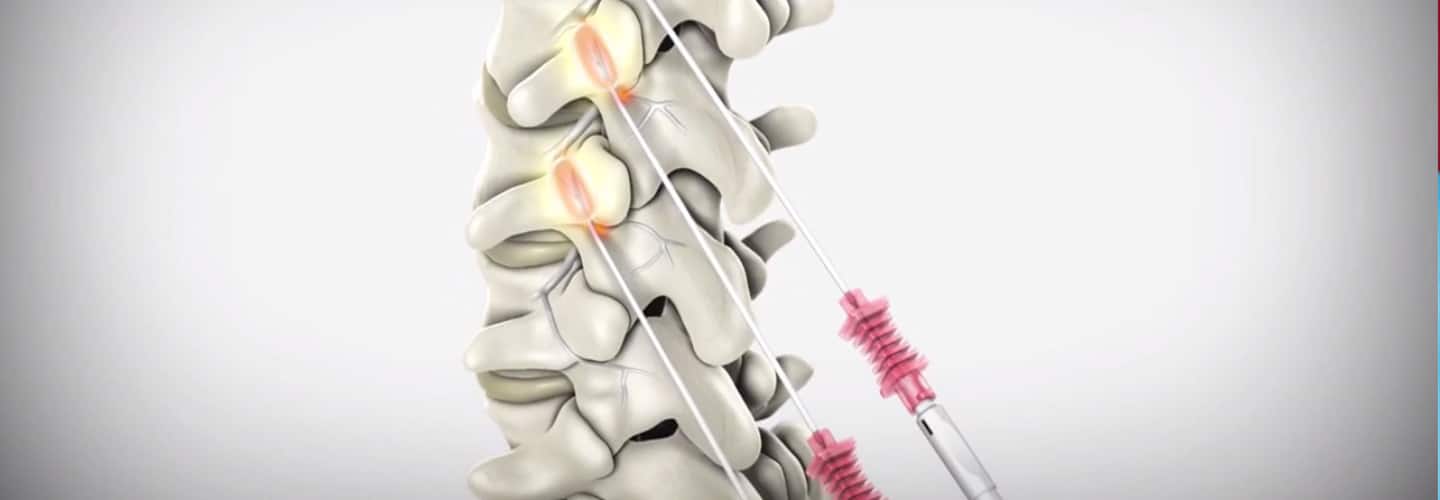
January 1, 2020 - we now have a new Pain Management Code CPT 64625 - SI Ablation Description of CPT Code 64625 Radiofrequency ablation, nerves innervating the sacroiliac joint, with imaging guidance (Fluoroscopic or Computed Tomography). Keypoints to REMEMBER!
Need help? Contact our office today!
0 Comments
The Patients Access plays a very important role in capturing and collection of patient service revenue. Patients Access and a Successful Revenue Cycle Management The Patients Access plays a very important role in capturing and collection of patient service revenue. There are 3 parts of Revenue Cycle where the Patient Access Management is very important and the Patient Access Team plays a very valuable role. 1. Pre-service Phase
2. Time of Service
3. Post-service Phase
Focusing on Customer Service and Patient Satisfaction is very important.  Customer Service and Patient Satisfaction 1. Treating patient with respect and dignity 2. Treating patient as you would want to be treated 3. Communicating in a manner the patient can easily understand 4. Value your patient's time and focus on efficiency 5. Show empathy to your patient What pieces of information do we gather:
Additional Useful information that you can also gather from the patient:
So what's next after obtaining all the necessary information? 1. Patient access team member must start confirming coverage for the patient 2. Verify if the provider is in-network or out-of-network with the patient's plan 3. Check eligibility if the patient is eligible for coverage on the date of service 4. Ask the patient if they have a secondary insurance coverage 5. Complete clarifying the benefits for services with the insurance company 6. Check the patient's copayment or any co-responsibility and if the patient has an out of pocket amount that has to be met (family or individual 7. You can ask the insurance company for specific benefits for specific services. I always suggest giving insurance company specific CPT code(s) or Diagnosis code(s) if available - document everything 8. Collect the copay at the time of service if you are contracted with the patient's insurance plan; 9. Verify if there is a deductible or coinsurance and how much have been met, you can collect them at the time of service as well 10. Make sure you be knowledgeable enough on how to answer the patient about their concern and questions about their copay or any other co-responsibility. Let's look at how the Patient Access team verifies patient who has a Medicaid Coverage: Viewing a patient's ID card alone does not ensure their Medicaid eligibility, nor does having a referral or pre-certification on file. As a member of the Patient Access team, insurance can be verified during pre-service or on the date of service. It is imperative in my opinion that the Patient Access team must verify eligibility during the MONTH that patient is scheduled to be seen or is coming for service. Because their coverage may always change. If you fail to verify eligibility, there is a very high risk of claim denial for sure. Possible scenarios? the patient may not be eligible at the time of service, or the HMO was not contracted with your practice at that time of service. Result? claim may not get paid. Resulting in lose of revenue. What happens if we did not correctly verify the patient identity?
About 40% of data used for revenue cycle management are gathered by Patients Access Teams. About 40% of data used for revenue cycle management are gathered by Patients Access Teams. Mistakes and errors will greatly affect the billing and coding process thus causing payments delay. Delayed reimbursement will significantly affect your cash flow. Patients satisfaction, prompt payments are the best results of your high quality customer service and are all based on how good your team with their communication skills. Let's decribe this code: CPT 76140 Consultation on x-ray examination made elsewhere, written report. (2D reformatting is no longer separately reported. To report 3D rendering, see 76376, 76377) So the question is, can a Provider bill for X-ray review using CPT Code 76140? Sharing to you coding clarification here. (Source are from CPT Assistant as published by the AMA). CPT is a trademark and owned by the American Medical Association. CPT Assistant October 1997
Using CPT Code 76140 76140 Consultation on x-ray examination made elsewhere, written report. You would use this code when a physician's opinion or advice regarding a specific film is requested by another physician and upon examination of the film, the consulting physician renders his or her consultation (ie, or his/her opinion or advice) to the requesting physician in the form of a written report. If a patient presents to an office for a new patient visit and brings to the physician his or her medical records, including x-rays, you should not report code 76140. Although the x-rays may have been taken elsewhere, the physician does not perform a consultation as intended by code 76140. Rather, the review or re-read of the x-rays would be considered part of the face-to-face E/M service provided to the patient. Again, the E/M codes include work done before, during, or after the E/M visit. Review of x-rays is part of the E/M service. Remember, 76140 represents a consultation, in which a physician only renders an opinion or gives advice regarding the film in the form of a written report. In general, when reporting 76140, the physician is not concurrently providing an E/M face-to-face service to the patient. CPT CODE 20552, 20553 TRIGGER POINT INJECTIONS. Medicare guideline. CPT Codes and Description
Understanding Trigger Point Injection Trigger point injection is one of many modalities utilized in the management of chronic pain. Myofascial trigger points are self-sustaining hyperirritative foci that may occur in any skeletal muscle in response to strain produced by acute or chronic overload. These trigger points produce a referred pain pattern characteristic for that individual muscle. Each pattern becomes part of a single muscle myofascial pain syndrome (MPS) and each of these single muscle syndromes are responsive to appropriate treatment, which includes injection therapy. An injection is achieved with the insertion of a needle and the administration of agents, such as local anesthetics, steroids and/or local inflammatory drugs. The diagnosis of trigger points requires a detailed history and thorough physical examination. The following clinical symptoms may be present when making the diagnosis:
The goal is to treat the cause of the pain and not just the symptom of pain. Limitations Acupuncture is not a covered service, even if provided for the treatment of an established trigger point. Use of acupuncture needles and/or the passage of electrical current through these needles is not covered (whether an acupuncturist or other provider renders the service). Medicare does not cover Prolotherapy. Its billing under the trigger point injection code is a misrepresentation of the actual service rendered. When a given site is injected, it will be considered one injection service, regardless of the number of injections administered. Utilization Guidelines It is expected that trigger point injections would not usually be performed more often than three sessions in a three month period. If trigger point injections are performed more than three sessions in a three month period, the reason for repeated performance and the substances injected should be evident in the medical record and available to the Contractor upon request. This contractor may request records when it is apparent that patients are requiring a significant number of injections to manage their pain. Documentation in the medical record must support the medical necessity and frequency of the trigger point injection(s). 20552, 20553 DX Crossover based on Medical NecessityM53.82 Other specified dorsopathies, cervical region M54.2 Cervicalgia M54.5 Low back pain M54.6 Pain in thoracic spine M60.80 Other myositis, unspecified site M60.811 Other myositis, right shoulder M60.812 Other myositis, left shoulder M60.819 Other myositis, unspecified shoulder M60.821 Other myositis, right upper arm M60.822 Other myositis, left upper arm M60.829 Other myositis, unspecified upper arm M60.831 Other myositis, right forearm M60.832 Other myositis, left forearm M60.839 Other myositis, unspecified forearm M60.841 Other myositis, right hand M60.842 Other myositis, left hand M60.849 Other myositis, unspecified hand M60.851 Other myositis, right thigh M60.852 Other myositis, left thigh M60.859 Other myositis, unspecified thigh M60.861 Other myositis, right lower leg M60.862 Other myositis, left lower leg M60.869 Other myositis, unspecified lower leg M60.871 Other myositis, right ankle and foot M60.872 Other myositis, left ankle and foot M60.879 Other myositis, unspecified ankle and foot M60.88 Other myositis, other site M60.89 Other myositis, multiple sites M60.9 Myositis, unspecified M75.80 Other shoulder lesions, unspecified shoulder M75.81 Other shoulder lesions, right shoulder M75.82 Other shoulder lesions, left shoulder M79.11 Myalgia of mastication muscle M79.12 Myalgia of auxiliary muscles, head and neck M79.18 Myalgia, other site M79.7 Fibromyalgia Take-away! Remember that these codes CPT 20552, 20553 are NOT billable as unilateral. Modifier 50 (bilateral) will NOT apply. Bill by the number of muscles! POLICY SOURCE: NOVITAS PART B LCD L35010 TRIGGER POINT INJECTIONS
READER'S QUESTION: Does Medicare Cover Radiofrequency Ablation for Pain Management in New York? Here's the Coverage Information from Medicare Part BIndications:
General Procedure Requirements:
Diagnostic Facet Joint Injections
Therapeutic Injections
Thermal Medial Branch Radiofrequency Neurotomy (includes RF and microwave technologies):
Limitations of Coverage: A maximum of five (5) facet joint injection sessions inclusive of medial branch blocks, intraarticular injections, facet cyst rupture and RF ablations may be performed per year in the cervical/thoracic spine and five (5) in the lumbar spine.
Let's describe the CPT codes 64633-64636 CPT CODE 64633 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); CERVICAL OR THORACIC, SINGLE FACET JOINT CPT CODE +64634 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); CERVICAL OR THORACIC, EACH ADDITIONAL FACET JOINT (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) CPT CODE 64635 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); LUMBAR OR SACRAL, SINGLE FACET JOINT CPT CODE +64636 DESTRUCTION BY NEUROLYTIC AGENT, PARAVERTEBRAL FACET JOINT NERVE(S), WITH IMAGING GUIDANCE (FLUOROSCOPY OR CT); LUMBAR OR SACRAL, EACH ADDITIONAL FACET JOINT (LIST SEPARATELY IN ADDITION TO CODE FOR PRIMARY PROCEDURE) Source reference: LCD ID L35936 Facet Joint Injections, Medial Branch Blocks, and Facet Joint Radiofrequency Neurotomy NGS Medicare Part B National Government Services, Inc. MAC - Part A 06101 - MAC A J - 06 Illinois National Government Services, Inc. MAC - Part B 06102 - MAC B J - 06 Illinois National Government Services, Inc. MAC - Part A 06201 - MAC A J - 06 Minnesota National Government Services, Inc. MAC - Part B 06202 - MAC B J - 06 Minnesota National Government Services, Inc. MAC - Part A 06301 - MAC A J - 06 Wisconsin National Government Services, Inc. MAC - Part B 06302 - MAC B J - 06 Wisconsin National Government Services, Inc. A and B and HHH MAC 13101 - MAC A J - K Connecticut National Government Services, Inc. A and B and HHH MAC 13102 - MAC B J - K Connecticut National Government Services, Inc. A and B and HHH MAC 13201 - MAC A J - K New York - Entire State National Government Services, Inc. A and B and HHH MAC 13202 - MAC B J - K New York - Downstate National Government Services, Inc. A and B and HHH MAC 13282 - MAC B J - K New York - Upstate National Government Services, Inc. A and B and HHH MAC 13292 - MAC B J - K New York - Queens National Government Services, Inc. A and B and HHH MAC 14111 - MAC A J - K Maine National Government Services, Inc. A and B and HHH MAC 14112 - MAC B J - K Maine National Government Services, Inc. A and B and HHH MAC 14211 - MAC A J - K Massachusetts National Government Services, Inc. A and B and HHH MAC 14212 - MAC B J - K Massachusetts National Government Services, Inc. A and B and HHH MAC 14311 - MAC A J - K New Hampshire National Government Services, Inc. A and B and HHH MAC 14312 - MAC B J - K New Hampshire National Government Services, Inc. A and B and HHH MAC 14411 - MAC A J - K Rhode Island National Government Services, Inc. A and B and HHH MAC 14412 - MAC B J - K Rhode Island National Government Services, Inc. A and B and HHH MAC 14511 - MAC A J - K Vermont National Government Services, Inc. A and B and HHH MAC 14512 - MAC B J - K Vermont |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985









 RSS Feed
RSS Feed