How to Bill Chronic Care Management 99490 and Complex CCM 99487, 99489  Chronic Care Management Services and the New Changes for 2017 CMS Medicare recognizes the Chronic Care Management (CCM) as a critical component of primary care services that contributes to better health and care for individuals. So in 2015, Medicare began paying separately under the Medicare Physician Fee Schedule for CCM services furnished to Medicare patients with multiple chronic conditions. Beginning January 1, 2017, the CCM codes are: Code 99490 Chronic care management services, at least 20 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month, with the following required elements:
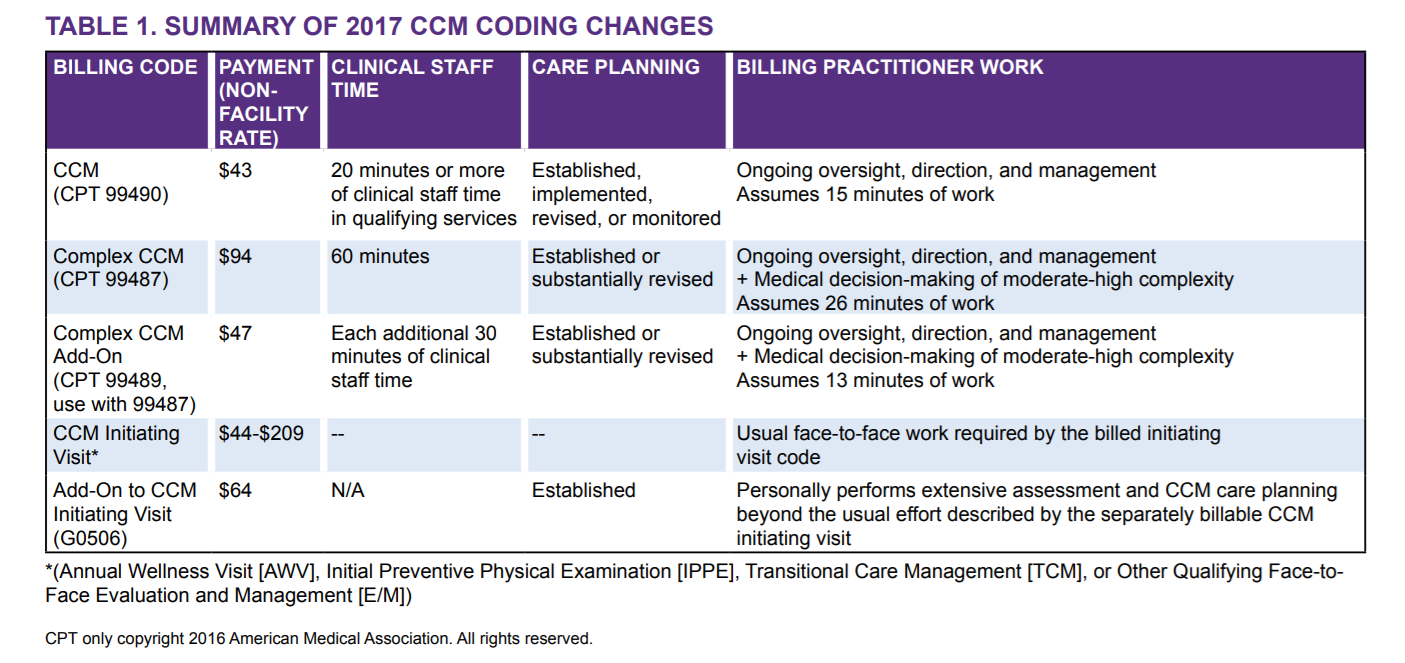
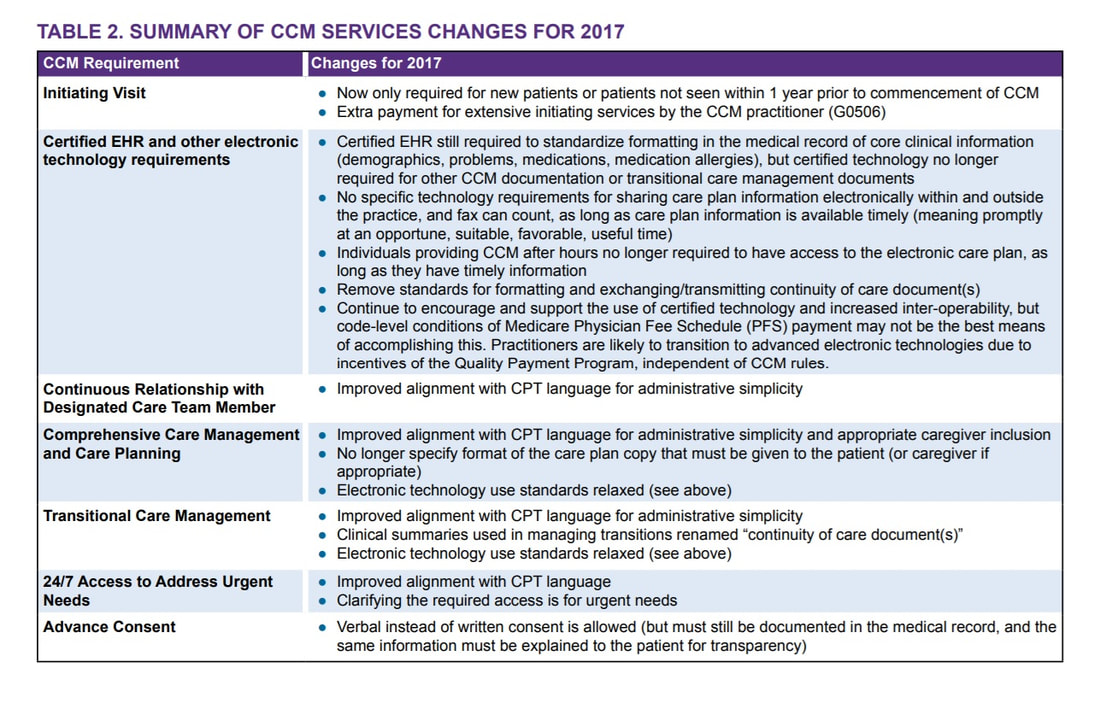
Keys to Remember: Let’s try to describe what CCM is or Chronic Care Management Services. These are services rendered by a Physician or Non-Physician Practitioners such as Nurse Practitioners, Physician Assistants, Clinical Nurse Specialist, Certified Nurse-Midwife and the CLINICAL Staff --- per month, for patients with two or more chronic medical conditions expected to last at least 12 months or until the death of the patient, and that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline. Take note that ONLY (1) One Practitioner can report and bill for Chronic Care Management per month. The included services are: ○ Access and use of a Certified Electronic Health Record (EHR) ○ Continuity of Care with Designated Care Team Member ○ Comprehensive Care Management and Care Planning ○ Transitional Care Management ○ Coordination with Home and Community-Based Clinical Service Providers ○ 24/7 Access to Address Urgent Needs ○ Enhanced Communication (email, and telephone for example) ○ Advance Consent CCM Changes in 2017 are the following:
There is a more complex care and we describe it as Complex Chronic Care Management services; Here are your two new codes for the Complex CCM - Complex Chronic Care Management services: CPT 99487 Complex chronic care management services, with the following required elements: ● Multiple (two or more) chronic conditions expected to last at least 12 months, or until the death of the patient; ● Chronic conditions place the patient at significant risk of death, acute exacerbation/ decompensation, or functional decline; ● Establishment or substantial revision of a comprehensive care plan ● Moderate or high complexity medical decision making ● 60 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month (Novitas Part B NJ North $102.36) CPT +99489 --- (this is an add-code and cannot be billed by itself!) Each additional 30 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month (List separately in addition to code for primary procedure) Complex CCM services of less than 60 minutes in duration, in a calendar month, are not reported separately(Novitas Part B NJ North $50.98) Supervision The CCM codes (CPT 99487, 99489, and 99490) are assigned general supervision under the Medicare PFS. General supervision means when the service is not personally performed by the billing practitioner, it is performed under his or her overall direction and control although his or her physical presence is not required. Patient Eligibility Patients with multiple (two or more) chronic conditions expected to last at least 12 months or until the death of the patient, and that place the patient at signifcant risk of death, acute exacerbation/decompensation, or functional decline are eligible for CCM services. ● Billing practitioners may consider identifying patients who require CCM services using criteria suggested in CPT guidance (such as number of illnesses, number of medications or repeat admissions or emergency department visits) or the profile of typical patients in the CPT prefatory language. ● There is a need to reduce geographic and racial/ethnic disparities in health through provision of CCM services. Table 2 provides a number of resources for identifying and engaging subpopulations to help reduce these disparities. The billing practitioner cannot report both complex and regular (non-complex) CCM for a given patient for a given calendar month. In other words, a given patient receives either complex or non-complex CCM during a given service period, not both. Examples of chronic conditions include, but are not limited to, the following: ● Alzheimer’s disease and related dementia ● Arthritis (osteoarthritis and rheumatoid) ● Asthma ● Atrial fbrillation ● Autism spectrum disorders ● Cancer ● Cardiovascular Disease ● Chronic Obstructive Pulmonary Disease ● Depression ● Diabetes ● Hypertension ● Infectious diseases such as HIV/AIDS Initiating Visit For new patients or patients not seen within one year prior to the commencement of CCM, Medicare requires initiation of CCM services during a face-to-face visit with the billing practitioner (an Annual Wellness Visit [AWV] or Initial Preventive Physical Exam [IPPE], or other face-to-face visit with the billing practitioner). This initiating visit is not part of the CCM service and is separately billed. Practitioners who furnish a CCM initiating visit and personally perform extensive assessment and CCM care planning outside of the usual effort described by the initiating visit code may also bill HCPCS code G0506 (Comprehensive assessment of and care planning by the physician or other qualifed health care professional for patients requiring chronic care management services [billed separately from monthly care management services] [Add-on code, list separately in addition to primary service]). G0506 is reportable once per CCM billing practitioner, in conjunction with CCM initiation. Patient Consent Obtaining advance consent for CCM services ensures the patient is engaged and aware of applicable cost sharing. It may also help prevent duplicative practitioner billing. A practitioner must obtain patient consent before furnishing or billing CCM. Consent may be verbal or written but must be documented in the medical record, and includes informing them about: ● The availability of CCM services and applicable cost-sharing ● That only one practitioner can furnish and be paid for CCM services during a calendar month ● The right to stop CCM services at any time (effective at the end of the calendar month)
0 Comments
|

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985


 RSS Feed
RSS Feed