How to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers  Many physician groups or even individual solo practice offices are not happy with their contracted rates or the way they are being reimbursed by the insurance payers? Is it time to negotiate? when is the best time to negotiate your contract? There is no better time than NOW! But there are important steps that you need to do before doing so. Negotiating your contract is not only by picking up the phone and calling the insurance payer's provider services department and asking them that you would like to negotiate your contracted fees. Unfortunately, it doesn't work that way! But there are important steps that you need to do before doing so. Negotiating your contract is not only by picking up the phone and calling the insurance payer's provider services department. It doesn't work that way! Here are my tips: How to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers
You need to present your reasoning why you think its time to negotiate your fees! All of the above, you can present it to the Insurance Payer through the Network Area Manager. Put them all together. Document everything! You can initiate the process by calling, and then by sending a formal letter of intent to renegotiate your contract rates or fee schedule. Don't forget to involve your billers and coders in this project! Let your patients leave feedback, reviews and about their experience in your practice! All these will surely help get you a better deal. It's a bit of a process but just be patient and work on it. Do you need help on how to Negotiate your Physician Group or Individual Provider's Contract with the Insurance Payers? You should contact us today!
0 Comments
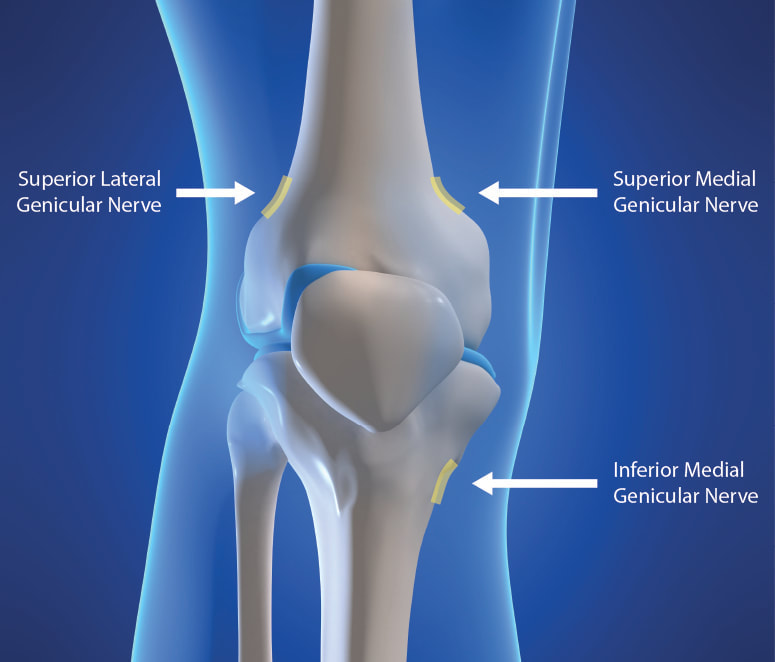
Understanding the Genicular Nerves (image below)Do you remember the struggle when we didn't have the specific code for the Genicular Nerve Knee Block and for the ablation or the RFA? Prior to January 1, 2020, we used to code them using 64450 for the Peripheral Nerve Block and the you used the 64640 for the Ablation. Not only that, you need to know the nerves that were blocked or were RFA'ed. But Effective January 1, 2020, we have now a specific code for the Genicular Nerve Knee Block and the Genicular Nerve Knee Ablation. You can read more about that change in our blog. CLICK HERE. CPT 64454 Genicular Nerve Block Injection(s), anesthetic agent(s) and/or steroid; genicular nerve branches, including imaging guidance, when performed CPT 64624 Genicular Nerve Ablation or RFA Destruction by neurolytic agent, genicular nerve branches including imaging guidance, when performed Unfortunately many of our Pain and Orthopedic Physicians are still struggling getting reimbursed for these services even though we already have these specific codes in place since 2020. And why is that? There are common issues why: 1) Their billing staff are still using the old codes CPT 64450, CPT 64640 instead of the CPT Code 64454 and 64624 for the Genicular Nerve Block and Radiofrequency Ablation; 2) What I found is that, this is considered as Investigational and Experimental based on the following guideline when being reported: Genicular nerve blocks and genicular nerve ablation are considered investigational and not medically necessary for the treatment of chronic knee pain, including but not limited to any of the following:
But I have also read that there are two CMS Contractors who covers for this procedure based on Medical Necessity. See Group 1 Diagnosis Codes Cross Over: Group 1 DX Codes:
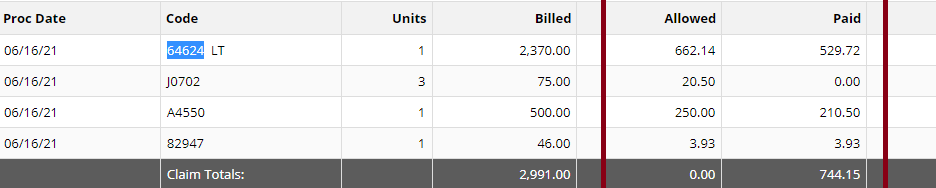
Read more about guidelines: National Government Services Inc Billing and Coding: Peripheral Nerve Blocks (A57452) First Coast Service Options, Inc Billing and Coding: Peripheral Nerve Blocks (A57788) More Guidelines from Payers which consider the procedure to be Investigational: Aetna Healthcare Anthem Blue Cross Blue Shield How do you handle Denial and Appeal for Genicular Nerve Ablation or Genicular Nerve Block? Here are my tips: Avoid the denials in the first place! by knowing your payers' guidelines; If the Provider says its Medically Necessary for the patient to receive the genicular nerve block or genicular nerve ablation, try getting a Predetermination based on Medical Necessity from your Payer! They will not allow you to submit Prior Authorization because for sure, it does not need Prior Authorization because its not a covered benefit based on their policy because the payer considers it "investigational" or "experimental"; Insist on reviewing Predetermination based on Medical Necessity instead! Already having denied claims? - pursue the claims by sending appeals, get your patient get involved with the appeals process. Be prepared with your medical documentation! How's the Patient's Pain Relief? Duration of Pain Relief? Improved ADL? - include that all in your documentation! Searched Keywords: GENICULAR NERVE BLOCK DENIAL AND APPEAL CPT BILLING CODE 64454 This is how it looks like when you get paid for Genicular Nerve Knee RFAgenicular-nerve-block-denial-and-appeal.html. Does this not look nice? HOW TO GET PAID FOR GENICULAR NERVE KNEE INJECTIONS Need help how to Appeal your claims? Contact Us today! Need help how to obtain Pre-determination before you render the Genicular Nerve Block to your patients? You should contact us today! |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985



 RSS Feed
RSS Feed