CLAIMS DENIALS: SOLUTIONS TO MAXIMIZING REVENUE AND MINIMIZING LOSSES Healthcare organizations are facing significant financial pressure due to various factors such as wage inflation, rising costs, declining patient and service volume, and the lingering uncertainty caused by the pandemic. These challenges are further compounded by the prevalence of unresolved claims denials, which lead to substantial annual losses for hospitals and healthcare facilities. In order to alleviate this financial burden, it is essential for organizations to adopt a strategic approach that focuses on preventing denials and effectively managing the claims process. The Rising Denial Rates: Over the past five years, denial rates have been on the rise, with an average increase of over 20 percent. Currently, the average claims denial rate exceeds 10 percent. A recent survey conducted by the Medical Group Management Association (MGMA) reveals that medical practices experienced an average increase in denials of 17 percent in 2021 alone. Industry data indicates that nearly 20 percent of all claims are denied, and a significant portion of returned claims are never resubmitted. The cost of reworking or appealing denials further exacerbates the financial impact, with practices spending an average of $25 per claim, and hospitals facing a staggering $181 per claim. Identifying the Common Causes: Preventing denied claims begins with understanding the most common reasons for claim rejections.
Effective Denial Management and Prevention:To mitigate the financial impact of denied claims, healthcare organizations should prioritize prevention efforts while also implementing effective denial management strategies. This involves:
Best Practices to Combat Denials: Implementing the following best practices can significantly enhance denials management and improve overall outcomes:
Leveraging Technology Solutions: Implementing the right technology resources can significantly enhance denial management efforts. Claim editor or "claim scrubber" software can help identify coding errors, medical necessity issues, and technical errors before claims are submitted. Medical claim scrubber solutions automate the matching of diagnosis and procedure codes, ensuring compliance with coding guidelines. Code check software and encoders validate and improve coding accuracy, saving time and improving efficiency. Mitigating Losses and Protecting the Bottom Line: While it may not be possible to eliminate denials entirely, a strategic and proactive approach, backed by data analysis, automation, and technology tools, can mitigate their impact on the financial bottom line. By continuously monitoring, identifying trends, collaborating with payers, and adhering to best practices, healthcare organizations can reduce write-offs and safeguard their revenues. Efficient denial management requires a comprehensive approach that includes prevention, understanding denial codes, effective correction and appeals, continuous improvement, collaboration with payers, and leveraging technology solutions. By implementing these strategies and practices, healthcare organizations can minimize the financial impact of denied claims, optimize revenue generation, and maintain a stable bottom line while providing quality care to patients. The Role of Staff Training: Investing in staff training is crucial for effective denial management. By equipping employees with the necessary knowledge and skills, organizations can reduce errors and improve the accuracy of claims submissions. Training should cover topics such as coding guidelines, payer requirements, documentation best practices, and effective communication with payers. Continuous Monitoring and Analysis: To stay ahead of denials, it's essential to continuously monitor and analyze denial data. Regularly running reports to identify denial patterns and trends can provide valuable insights into the root causes of denials. By identifying these patterns, organizations can take proactive measures to prevent future denials, implement process improvements, and enhance overall revenue cycle management. Utilizing Outsourced Services: For healthcare organizations that lack the resources or expertise to handle denial management internally, outsourcing services can be a viable solution. Outsourced medical billing and coding companies specialize in managing denials, ensuring efficient claims processing, and optimizing revenue collection. By leveraging the expertise of these external partners, organizations can alleviate the burden on their internal teams and achieve better denial management outcomes. Our company, the GoHealthcare Practice Solutions can easily help you with this! Denial management is a critical component of revenue cycle management in healthcare organizations. By focusing on prevention, utilizing effective denial management strategies, leveraging technology solutions, and investing in staff training, organizations can mitigate the financial impact of denied claims and protect their bottom line. Continuous monitoring, analysis of denial patterns, and collaboration with payers are essential to identify opportunities for improvement and implement proactive measures. By adopting these best practices, healthcare organizations can optimize revenue generation, enhance operational efficiency, and provide quality care to their patients. Reading Sources and References:
Contact us today!
0 Comments
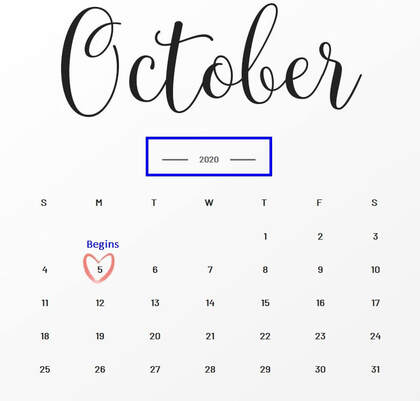
The $20 billion Provider New Phase 3 Relief Funding is now open and you have from October 5, 2020 to November 6, 2020 to submit your application. The HHS through HRSA (Health Resources and Services Administration) had announced the $20 billion New Phase 3 Relief Funding which began yesterday, October 5, 2020. Who are covered? Read Provider Eligibility. HHS is making a large number of providers eligible for Phase 3 General Distribution funding, including:
Understanding the Provider Relief Phase 3 Funding Payment Methodology. All eligible providers will be considered for payment against the below criteria.
All payment recipients will be required to attest to receiving the Phase 3 General Distribution payment and accept the associated Terms and Conditions. Pay Attention with the Deadline. Healthcare Providers will have from October 5, 2020 through November 6, 2020 to apply for Phase 3 General Distribution funding. Funding for this Phase 3 General Distribution was made possible through the bipartisan CARES Act and the Paycheck Protection Program and Health Care Enhancement Act, which allocated $175 billion in relief funds to hospitals and other healthcare providers. Source of Information: https://www.hhs.gov/about/news/2020/10/1/trump-administration-announces-20-billion-in-new-phase-3-provider-relief-funding.html
The Patients Access plays a very important role in capturing and collection of patient service revenue. Patients Access and a Successful Revenue Cycle Management The Patients Access plays a very important role in capturing and collection of patient service revenue. There are 3 parts of Revenue Cycle where the Patient Access Management is very important and the Patient Access Team plays a very valuable role. 1. Pre-service Phase
2. Time of Service
3. Post-service Phase
Focusing on Customer Service and Patient Satisfaction is very important.  Customer Service and Patient Satisfaction 1. Treating patient with respect and dignity 2. Treating patient as you would want to be treated 3. Communicating in a manner the patient can easily understand 4. Value your patient's time and focus on efficiency 5. Show empathy to your patient What pieces of information do we gather:
Additional Useful information that you can also gather from the patient:
So what's next after obtaining all the necessary information? 1. Patient access team member must start confirming coverage for the patient 2. Verify if the provider is in-network or out-of-network with the patient's plan 3. Check eligibility if the patient is eligible for coverage on the date of service 4. Ask the patient if they have a secondary insurance coverage 5. Complete clarifying the benefits for services with the insurance company 6. Check the patient's copayment or any co-responsibility and if the patient has an out of pocket amount that has to be met (family or individual 7. You can ask the insurance company for specific benefits for specific services. I always suggest giving insurance company specific CPT code(s) or Diagnosis code(s) if available - document everything 8. Collect the copay at the time of service if you are contracted with the patient's insurance plan; 9. Verify if there is a deductible or coinsurance and how much have been met, you can collect them at the time of service as well 10. Make sure you be knowledgeable enough on how to answer the patient about their concern and questions about their copay or any other co-responsibility. Let's look at how the Patient Access team verifies patient who has a Medicaid Coverage: Viewing a patient's ID card alone does not ensure their Medicaid eligibility, nor does having a referral or pre-certification on file. As a member of the Patient Access team, insurance can be verified during pre-service or on the date of service. It is imperative in my opinion that the Patient Access team must verify eligibility during the MONTH that patient is scheduled to be seen or is coming for service. Because their coverage may always change. If you fail to verify eligibility, there is a very high risk of claim denial for sure. Possible scenarios? the patient may not be eligible at the time of service, or the HMO was not contracted with your practice at that time of service. Result? claim may not get paid. Resulting in lose of revenue. What happens if we did not correctly verify the patient identity?
About 40% of data used for revenue cycle management are gathered by Patients Access Teams. About 40% of data used for revenue cycle management are gathered by Patients Access Teams. Mistakes and errors will greatly affect the billing and coding process thus causing payments delay. Delayed reimbursement will significantly affect your cash flow. Patients satisfaction, prompt payments are the best results of your high quality customer service and are all based on how good your team with their communication skills. 5 Mindful ways to Improving Patient Access Access is a significant concern in the United States and all over the world when it comes to patient care. We all know that the patients have to wait for months to get the physician they want, and a good doctor has more patients than they can manage. The patients waiting for months to get the physician surely lead to delayed treatment and also can jeopardize their health and their life. On the other hand, it will certainly reduce the patient satisfaction scores for the doctors and the medical service providers. As these scores have to be shared with third parties such as pharmaceuticals and drug companies as well as the insurance companies, managing the scores is extremely significant for the doctors. So here are a few ways that you can make sure your patients are not sitting and waiting for you to give them an appointment for half a year. Step 1: Learn how to Measure The first appointment available is a valuable commodity. So make sure that you have a good system to call people who are on the waiting list. Not just the first appointment available, but the second and third appointments available can also be prescheduled. You should inform the patients that are on the waiting list that they can be called in for a consult at short notice. When a person is coming up for the next available appointment, you can inform them that they are next on the list. That will allow individuals to prepare for showing up without feeling like it was impractical to ask on such short notice. Call people up or have a reminder system in place that will inform people on the list when they are next on the list of first appointment available. There are many openings happening every day, and placing then effectively can reduce overextended waiting lists considerably. Step 2: Denied Appointment Requests The patients who were denied an appointment is also a crucial list that needs to be monitored closely. There are many reasons that a patient is denied care, and those reasons should be listed clearly. If there is no appointment available or the appointment is not given for another reason, the reasons should be listed. That process will allow the nurses and administration to solve the problem and will allow them to develop a system that reduces denied appointments. Step 3: Implementation of the Data The main focus of all of the points mentioned above is to have a system that focuses on developing data sheets on appointment schedules so that you can decide how to have a more productive appointment culture. Here are a few steps you should take in the implementation process:
● Ask your administration about how they feel that they are being pushed too hard in the appointment process. ● Develop a severity scale of the patient’s complaint in the form of a questionnaire. The patient will answer the questionnaire on the phone, and the nurse or staff can decide how urgently they need to see the doctor. Step 4: Effective Ways to Problem Solving Find effective and simple solutions that will increase patient access on a daily basis. A few and simple tips on the matter are as follows: ● Have four backup appointments for every day that the patients have already been informed of. That way, the patient can simply come in if another patient cancels their appointment, and they will already be prepared for it. ● Patients on their second consult or with small concerns can come and see the doctor while the first patient is getting their physical. ● If there is a list of symptoms common in the specialty of the doctor, then nurses can provide that list to the administrator. If a patient complains of these symptoms, then they will be called in by the nursing staff on an urgent basis. ● Avoid letting worthy patients go to waiting lists for chronic complainers. Patients who have a tendency to over complaint can be seen and managed by the nursing staff. Step 5: Execute Now, all it is left is to reorganize these concepts and make sure that they are implemented effectively. You will see amazing results with a small number of initiatives. We are here for any ideas that you want to discuss. We are experts in the field. Share your experiences with us in the comments section, and we would love to get back to you! Modifier 58 Staged or Related Procedure or Service During Postoperative Period by Same Physician  Guideline: The same physician planned, at time of original surgery/procedure, a return trip to operating or procedure room within 10 or 90 day post op days WHEN IT IS APPROPRIATE:
Physicians in same specialty, same group are to bill and are reimbursed as a single physician Key to Remember! Use modifier 78 (not 58!) for treatment problems unplanned requiring return trip to operating room If hardware removed in unplanned surgery return for a complication, (e.g. infection of the wound site or rejection of the hardware itself), modifier 78 appropriate It is NOT APPROPRIATE WHEN:
References:
CMS Medicare Website Coding Books Payers Websites Definition: Bilateral Procedure; procedures/services that occur on identical, opposing structures (such as for example - "LEFT" and "RIGHT" Side)
Many Billers are still really confused on how Modifier 50 really works. APPROPRIATE:
Billed as 64490 -50 1 unit
INAPPROPRIATE:
Coding Tip: Generally speaking, the above information applies when two of the same procedure codes are performed on the same day for the same patient by the same provider. However, there could be instances where two separate procedure codes are used. If so, Medicare's payment or denial would depend on any other type of rules or regulations concerning the individual services in question. This could include the National Correct Coding Initiative (NCCI) that could necessitate additional modifiers, duplicate edits, and global surgery edits. Remember, the Modifier 50 is used as a payment, rather than informational, modifier. The addition of this modifier could affect payment depending on the procedure code and the BILAT SURG indicator. The BILAT SURG indicator for each procedure code can be found on the Medicare Physician Fee Schedule Relative Value File. Following are the indicators and their descriptions. BILAT SURG indicator "0" =150% payment adjustment for bilateral procedures does not apply. If procedure is reported with modifier -50 or with modifiers RT and LT, base the payment for the two sides on the lower of: (a) the total actual charge for both sides and (b) 100% of the fee schedule amount for a single code. Example: The fee schedule amount for code XXXXX is $125. The physician reports code XXXXX-LT with an actual charge of $100 and XXXXX-RT with an actual charge of $100. Payment should be based on the fee schedule amount ($125) since it is lower than the total actual charges for the left and right sides ($200). The bilateral adjustment is inappropriate for codes in this category (a) because of physiology or anatomy, or (b) because the code description specifically states that it is a unilateral procedure and there is an existing code for the bilateral procedure. BILAT SURG Indicator "1" =150% payment adjustment for bilateral procedures applies. If the code is billed with the bilateral modifier or is reported twice on the same day by any other means (e.g., with RT and LT modifiers, or with a 2 in the units field), base the payment for these codes when reported as bilateral procedures on the lower of: (a) the total actual charge for both sides or (b) 150% of the fee schedule amount for a single code. If the code is reported as a bilateral procedure and is reported with other procedure codes on the same day, apply the bilateral adjustment before applying any multiple procedure rules. Reference Manual: The CMS Internet-Only Manual, Publication 100-04, Chapter 12 , Section 40.7.B, indicates "If a procedure is not identified by its terminology as a bilateral procedure (or unilateral or bilateral), physician must report the procedure with modifier "-50". They report such procedure as a single line item." BILAT SURG Indicator "2" =150% payment adjustment does not apply. Relative Value Units (RVUs) are already based on the procedure being performed as a bilateral procedure. If the procedure is reported with modifier -50 or is reported twice on the same day by any other means (e.g., with RT and LT modifiers or with a 2 in the units field), base the payment for both sides on the lower of (a) the total actual charge by the physician for both sides, or (b) 100% of the fee schedule for a single code. Example: The fee schedule amount for code YYYYY is $125. The physician reports code YYYYY-LT with an actual charge of $100 and YYYYY-RT with an actual charge of $100. Payment should be based on the fee schedule amount ($125) since it is lower than the total actual charges for the left and right sides ($200). The RVUs are based on a bilateral procedure because (a) the code descriptor specifically states that the procedure is bilateral, (b) the code descriptor states that the procedure may be performed either unilaterally or bilaterally, or (c) the procedure is usually performed as a bilateral procedure. BILAT SURG Indicator "3" = the usual payment adjustment for bilateral procedures does not apply. If the procedure is reported with modifier -50 or is reported for both sides on the same day by any other means (e.g., with RT and LT modifiers or with a 2 in the units field), base the payment for each side or organ or site of a paired organ on the lower of (a) the actual charge for each side or (b) 100% of the fee schedule amount for each side. If the procedure is reported as a bilateral procedure and with other procedure codes on the same day, determine the fee schedule amount for a bilateral procedure before applying any multiple procedure rules. Services in this category are generally radiology procedures or other diagnostic tests which are not subject to the special payment rules for other bilateral surgeries. BILAT SURG Indicator "9" = The bilateral payment adjustment concept does not apply. Ambulatory Surgical Centers (ASCs) and Modifier 50 Bilateral surgical procedures furnished by certified ASCs may be covered under Part B. While use of the 50 modifier is not prohibited according to Medicare billing instructions, the modifier is not recognized for payment purposes and if used, may result in incorrect payment to ASCs. Bilateral procedures should be reported as a single unit on two separate lines or a single unit with "2" in the unit field on one line, in order for both procedures to be paid correctly. The multiple procedure reduction of 50 percent will apply to all bilateral procedures subject to multiple procedure discounting. Read more examples for appropriate billing procedures in the MLN Matters article, "Revised Payment System for Ambulatory Surgical Centers (ASC) in Calendar Year (CY) 2008" (Revised SE 0742). References: CMS: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf Noridian: https://med.noridianmedicare.com/web/jeb/specialties/surgery/bilateral-surgery American Medical Association Coding Guidelines Insurance Payment Allowed 100% of Charged Amount is not something to celebrate! I asked some of my readers about how they will feel if their claims has an allowed amount that is at 100% of the charged amount, wow! So, meaning, when you bill for $2000.00 and the insurance made their determination at 100% of your charges… you bill $2,000, they allowed $2,000 – would you be happy?
Honestly, if I see EOB like this, I will be very very nervous! Your provider could have been paid more than the practice submitted charges, isn’t it? Interestingly, most of my readers said they’ll be happy if they were paid at 100% of their charges… now, would you? What if the allowed amount could have been $2,500? – how much is the difference? Yep, $500! How can the payer allow $2,500 if you have only submitted a charged amount of $2,000?! Make sense? Ok, now, here’s the deal! — if you got paid at 100% based on your charged amount you should find out about your fee schedule or contracted rate or what is usual and customary if you are out of network provider. Make sure you know you are not under-charging the insurance payer. But what if you have realized that you did under-charge the insurance payer? what will you do? can you recover the money that you could have been paid for? The answer is YES! you can recover that money! Now, don’t wait too long! Take action immediately! Based on my experience, you can go back as far as 3 years from the date the claims were paid. I haven’t tried more than 3 years of claim to recover due to undercharges! After all, just like the insurance payer, they can always go back as far as more than 3 years I think to recover overpayments. Or depending on where state you are located. Pay attention on your EOBs! I think that’s the key. As soon as you discover there is an undercharging and you were paid 100% on your charged amount. Pick up the phone and call that insurance payer immediately. Connect with us today, we will show you better strategies on how to run an effective revenue cycle management! Can you bill a Medicare Patient for Missed Appointment or No-Show? When patients missed their appointments, it does cost you your time and your staff. In this article, you are wondering if you can bill Medicare when their beneficiaries missed and appointment or has no-show. Below you will find clarifications. According to Chapter 1, section 30.3.13 of the Medicare Claims Processing Manual, which is attached to CR5613, CMS policy allows physicians, providers, and suppliers to charge Medicare beneficiaries for missed appointments, provided that they do not discriminate against Medicare beneficiaries but also charge nonMedicare patients for missed appointments and the charges for Medicare and non-Medicare patient are the same. The charge for a missed appointment is not a charge for a service itself (to which the assignment and limiting charge provisions apply), but rather is a charge for a missed business opportunity. Therefore, if a physician's or supplier's missed appointment policy applies equally to all patients (Medicare and non-Medicare), then the Medicare law and regulations do not preclude the physician or supplier from charging the Medicare patient directly. The other key points of CR5613 are:
According to Medicare guideline; "make certain that your billing staff is aware that you may bill the beneficiary directly, that Medicare itself does not make any payments for missed appointments, and that Medicare should not be billed for these charges". "The Centers for Medicare & Medicaid Services (CMS) policy is to allow physicians and suppliers to charge Medicare beneficiaries for missed appointments. However, Medicare itself does not pay for missed appointments, so such charges should not be billed to Medicare." "Providers may not charge ONLY Medicare beneficiaries for missed appointments; they must also charge non-Medicare patients. The amount the physician/supplier charges Medicare beneficiaries for missed appointments must be the same as the amount that they charge non-Medicare patients." Source: MLN: MM5613 Related Change Request Number: 5613 Need our professional consulting advise to run a more efficient Revenue Cycle Management? - call and talk to us at 609-481-3494
10 Common Reasons Claims Gets Denied and Rejected (1) Incorrect demographic information (insurance ID , date of birth, even the gender!)
Always scan a copy of your patient's primary and secondary insurance card. Make sure to get a copy of their new card (if there is a change) (2) Patient's non-coverage or terminated coverage at the time of service may also be the reason of denial. That is why, it is very important that you check on your patient's benefits and eligibility before seeing the patient (unfortunately, I have seen practices who does not check benefits and eligibility on their patients so they end up being not paid for the service they have rendered for the patient (3) Coding Issues (requires 5th digit, outdated codes)--- be careful also with your secondary/additional codes! Claims may be denied even if the problem was just because of the secondary codes!Again as I previously pointed out with my other articles on tracking your claims, with this problem, discuss solving the coding error rather than how much you want to get reimbursed. Most of the insurance companies will help you with codes (in fairness!!) and they also inform you on outdated codes, or codes that requires a 5th digit. You can also clarify by asking them more information on their reimbursement and utilization guidelines (4) Improper use of modifiers (be careful with bilateral procedures!, modifiers for professional and technical component, modifiers for multiple procedures, postoperative period, etc.) (5) No precertification or preauthorization obtained. It is so hard to file an appeal when the claim or service was non-precertified. Avoid this from happening! So be careful with your Surgical Procedures, Therapy Services and DME Services. (6) No referral on file. HMOs or the Managed Care normally requires a referral! (remember that!). Most Therapy Services would require a an order or script from the referring provider. Make sure the referring provider's NPI appears on Box 17 on your HCFA 1500 Claim Form (7) The patient has other primary insurance, the patient turn out to be a Workman's Comp case or an MVA case. Call our office, we can give you an example of our template of benefits eligibility verification. Remember, WC/MVA cases services are normally always require Prior Auth so make sure you have the claim information, connect with the Adjustor and the Nurse Case Manager (8) Claim requires documentation, require additional notes to support medical necessity. A well documented medical records is a good practice! (9) Claim requires referring physician's information (very common for Therapy Services and DME Billing requirements) (10) Untimely filing. So how can you prove that you did submit the claims in a timely manner? When unfortunately, most of the insurances does not accept your billing records on your practice management software that shows that date(s) you billed the insurance! They want a receipt from your electronic receipt or for postal mail, obviously they want a receipt too! a tracking number maybe? certified letter receipt? If you are submitting claims by electronic, make sure you generate transmission reports/receipts. Your reports must read "accepted" or "in process" and not "rejected". If you are sending claims by paper or postal mail, it is a good idea to send your claims as certified mail with tracking number, keep your transmission receipts! Need our professional consulting advise to run a more efficient Revenue Cycle Management? - call and talk to us at 609-481-3494 |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985













 RSS Feed
RSS Feed