CPT Codes for Sphenopalatine Ganglion Blocks in Pain Management Sphenopalatine ganglion blocks are an effective pain management intervention for patients with chronic head and facial pain. However, healthcare providers and insurance companies must understand the appropriate CPT codes for pain management procedures to ensure accurate billing and insurance coverage. In this article, we will provide a comprehensive guide to CPT codes for sphenopalatine ganglion blocks in pain management, including the most commonly used codes and their significance. What are Sphenopalatine Ganglion Blocks? Sphenopalatine ganglion blocks involve injecting a local anesthetic into the sphenopalatine ganglion, a collection of nerve cells located in the back of the nose. The procedure is performed to block pain signals transmitted by the trigeminal nerve, which can cause chronic head and facial pain. Sphenopalatine ganglion blocks are a minimally invasive procedure and can be performed in an outpatient setting. Why are CPT Codes for Pain Management Procedures Important? CPT codes for pain management procedures are essential because they determine how healthcare providers are reimbursed for their services. Each CPT code represents a specific procedure or service and has a corresponding fee schedule that providers use to determine the cost of the service. Healthcare providers must use the appropriate CPT codes for pain management procedures to ensure accurate billing and insurance coverage. Most Common CPT Codes for Sphenopalatine Ganglion Blocks in Pain Management There are several CPT codes used for sphenopalatine ganglion blocks in pain management, depending on the specific procedure performed and the number of levels treated. The most commonly used CPT codes for sphenopalatine ganglion blocks include: 64405 - Injection, anesthetic agent and/or steroid, sphenopalatine ganglion. 64999 - Unlisted procedure, nervous system. It is essential to consult with your healthcare provider and insurance carrier to determine the appropriate CPT code for your specific procedure, as the codes may vary depending on the specific procedure performed and the insurance carrier. CPT codes for sphenopalatine ganglion blocks in pain management are essential to ensure accurate medical billing and insurance coverage. The most commonly used CPT codes for sphenopalatine ganglion blocks include 64405 and 64999. Healthcare providers and insurance companies must be familiar with these codes to ensure that patients receive the care they need without financial burden. If you're experiencing chronic head or facial pain, talk to your healthcare provider to see if sphenopalatine ganglion blocks are a viable treatment option. And for healthcare providers, make sure that you use the proper CPT codes for pain management procedures to ensure proper billing and reimbursement. By following the proper guidelines for medical billing, we can ensure that patients receive the care they need while minimizing financial hardship.
0 Comments
CPT Codes for Percutaneous Adhesiolysis in Pain Management: A Comprehensive Guide Pain management is a crucial aspect of healthcare, and percutaneous adhesiolysis is one of the interventions commonly used to alleviate chronic pain conditions. However, healthcare providers and insurance companies must understand the appropriate CPT codes for pain management procedures to ensure accurate billing and insurance coverage. In this article, we will provide a comprehensive guide to CPT codes for percutaneous adhesiolysis in pain management, including the most commonly used codes and their significance. What is Percutaneous Adhesiolysis? Percutaneous adhesiolysis is a minimally invasive procedure used in pain management to treat chronic pain conditions caused by scar tissue or adhesions. The procedure involves inserting a needle into the epidural space and injecting a solution to dissolve or break up adhesions causing pain. The procedure is often performed under fluoroscopy guidance to ensure accurate placement of the needle and avoid complications. Why are CPT Codes for Pain Management Procedures Important? CPT codes for pain management procedures are essential because they determine how healthcare providers are reimbursed for their services. Each CPT code represents a specific procedure or service and has a corresponding fee schedule that providers use to determine the cost of the service. Healthcare providers must use the appropriate CPT codes for pain management procedures to ensure accurate billing and insurance coverage. Most Common CPT Codes for Percutaneous Adhesiolysis in Pain Management There are several CPT codes used for percutaneous adhesiolysis in pain management, depending on the specific procedure performed and the number of levels treated. The most commonly used CPT codes for percutaneous adhesiolysis include: 62311 - Percutaneous injection of substance into the spinal canal of thoracic, lumbar, or sacral spine. 62318 - Injection(s), including indwelling catheter placement, continuous infusion or intermittent bolus, of diagnostic or therapeutic substance(s) (e.g., anesthetic, antispasmodic, opioid, steroid, other solution), not including neurolytic substances, including needle or catheter placement, interlaminar epidural or subarachnoid, cervical or thoracic; lumbar or sacral (caudal). 62287 - Injection(s), including indwelling catheter placement, continuous infusion or intermittent bolus, of neurolytic substance(s) (e.g., alcohol, phenol, 10% dextrose) including neuraxial facet joint nerve; lumbar or sacral (caudal). It is essential to consult with your healthcare provider and insurance carrier to determine the appropriate CPT code for your specific procedure, as the codes may vary depending on the specific procedure performed and the insurance carrier. CPT codes for percutaneous adhesiolysis in pain management are essential to ensure accurate medical billing and insurance coverage. The most commonly used CPT codes for percutaneous adhesiolysis include 62311, 62318, and 62287. Healthcare providers and insurance companies must be familiar with these codes to ensure that patients receive the care they need without financial burden. If you're experiencing chronic pain, talk to your healthcare provider to see if percutaneous adhesiolysis is a viable treatment option. And for healthcare providers, make sure that you use the proper CPT codes for pain management procedures to ensure proper billing and reimbursement. By following the proper guidelines for medical billing, we can ensure that patients receive the care they need while minimizing financial hardship. CPT Codes for Discography in Pain Management Discography is a diagnostic procedure commonly used in pain management to determine the source of back pain. It involves injecting a contrast dye into the discs of the spine and imaging the results. CPT codes are used to report medical procedures and services. In this article, we will discuss the CPT codes for discography in pain management. CPT Code 62290: CPT code 62290 is used to report discography performed on one to three spinal levels. This code is commonly used when performing lumbar discography. CPT Code 62291: CPT code 62291 is used to report discography performed on four or more spinal levels. This code is commonly used when performing thoracic or cervical discography. CPT Code 77002: CPT code 77002 is used to report fluoroscopic guidance for procedures performed in the spine. This code is often reported with discography procedures to provide guidance during the injection process. CPT Code 77003: CPT code 77003 is used to report radiological supervision and interpretation for procedures performed in the spine. This code is often reported with discography procedures to provide radiological interpretation of the results. CPT codes play a critical role in reporting medical procedures and services, including discography in pain management. CPT codes 62290 and 62291 are used to report discography procedures performed on one to three spinal levels and four or more spinal levels, respectively. CPT codes 77002 and 77003 are used to report fluoroscopic guidance and radiological supervision and interpretation for discography procedures. Healthcare providers should ensure accurate coding and documentation to ensure appropriate reimbursement and compliance with coding guidelines. By understanding the CPT codes for discography in pain management, healthcare providers can ensure accurate reporting and optimize their revenue cycle management. 5 Ways Medical Billing Software Can Help You Address Denials and Appeals Denials and appeals are common challenges in medical billing. They can be time-consuming and frustrating for healthcare providers and can have a significant impact on the financial performance of healthcare practices. Medical billing software can be a valuable tool in addressing denials and appeals. In this article, we will discuss five ways medical billing software can help you address denials and appeals. Automated Denial Management: Medical billing software can help healthcare providers automate the denial management process. This includes tracking denials, identifying trends, and generating reports to help healthcare providers address the root cause of denials and implement corrective actions. Real-Time Claim Tracking: Medical billing software provides real-time claim tracking, allowing healthcare providers to monitor the status of claims and identify potential issues before they become denials. This can help to improve the chances of first-pass claim acceptance and reduce the number of denials. Advanced Reporting: Medical billing software provides advanced reporting capabilities, allowing healthcare providers to generate custom reports on denial rates, claim rejections, and other key performance indicators. This can help to identify trends and areas for improvement, allowing healthcare providers to take corrective actions. Appeals Management: Medical billing software can help healthcare providers manage the appeals process by providing a centralized platform for tracking and managing appeals. This can help to improve the efficiency and effectiveness of the appeals process and reduce the time and resources required to address appeals. Integrated Analytics: Medical billing software can provide integrated analytics, allowing healthcare providers to identify patterns and trends in claim denials and appeals. This can help healthcare providers to develop proactive strategies for addressing denials and appeals and optimizing their revenue cycle management. Medical billing software can be a valuable tool in addressing denials and appeals in medical billing. By automating denial management, providing real-time claim tracking, offering advanced reporting, managing appeals, and providing integrated analytics, medical billing software can help healthcare providers improve their financial performance and streamline their operations. Healthcare providers should consider investing in medical billing software to optimize their revenue cycle management and improve their financial performance. The US Healthcare Consulting Services Market - A Comprehensive Guide for the Modern Healthcare Professional In today's rapidly evolving healthcare landscape, the US Healthcare Consulting Services Market is gaining significant traction. This market offers a wide range of services that cater to various healthcare professionals, including surgeons, physicians, medical billers, and even hospital CEOs. This blog post aims to provide a comprehensive overview of the US Healthcare Consulting Services Market, touching upon its key players, services offered, and the benefits it brings to the healthcare sector. By the end of this post, you'll have a better understanding of how the US Healthcare Consulting Services Market can positively impact your organization. Understanding the US Healthcare Consulting Services Market The US Healthcare Consulting Services Market consists of numerous consulting firms that provide a variety of services tailored to the unique needs of healthcare professionals. These services range from strategic planning and operational improvements to financial management and IT solutions. The main goal of the US Healthcare Consulting Services Market is to help healthcare organizations stay competitive and deliver high-quality patient care by optimizing their processes, cutting costs, and implementing innovative solutions. Key Players in the US Healthcare Consulting Services Market Several prominent firms dominate the US Healthcare Consulting Services Market, offering specialized services to healthcare professionals. Some of the key players include:
Services Offered in the US Healthcare Consulting Services Market The US Healthcare Consulting Services Market offers a diverse range of services to cater to various healthcare professionals. These include:
Benefits of Leveraging the US Healthcare Consulting Services Market By partnering with a consulting firm in the US Healthcare Consulting Services Market, healthcare organizations can reap several benefits:
The US Healthcare Consulting Services Market offers a valuable resource for healthcare professionals looking to optimize their organizations and stay competitive in today's fast-paced industry. By partnering with experienced consulting firms, healthcare organizations can benefit from specialized expertise, enhanced operational efficiency, and improved patient care. Don't hesitate to explore the US Healthcare Consulting Services Market and unlock your organization's full potential. Understanding CPT Codes for Implantable Pain Pumps in Pain Management Implantable pain pumps are a type of medical device used to manage chronic pain. These devices are implanted under the skin and deliver medication directly to the spinal cord. Proper coding of implantable pain pump procedures is essential for accurate reimbursement and revenue cycle management. In this article, we will discuss CPT codes for implantable pain pumps in pain management. CPT Code 62350: CPT code 62350 is used to report the implantation of an intrathecal catheter for drug delivery systems, including implantable pain pumps. This code covers the placement of a catheter into the spinal cord for medication delivery. CPT Code 62351: CPT code 62351 is used to report the implantation of a subcutaneous or submuscular drug delivery system, including implantable pain pumps. This code covers the placement of a device under the skin or muscle for medication delivery. CPT Code 62355: CPT code 62355 is used to report the replacement or revision of an intrathecal catheter for drug delivery systems, including implantable pain pumps. This code covers the replacement or revision of a catheter that has already been implanted. CPT Code 62362: CPT code 62362 is used to report the removal of an intrathecal catheter for drug delivery systems, including implantable pain pumps. This code covers the removal of a catheter from the spinal cord. Proper coding of implantable pain pump procedures is essential for accurate reimbursement and revenue cycle management in pain management practices. CPT codes 62350, 62351, 62355, and 62362 are used to report the implantation, replacement or revision, and removal of intrathecal catheters and drug delivery systems, including implantable pain pumps. Pain management practices should ensure they are using the correct CPT codes for implantable pain pumps to ensure accurate reimbursement and optimize their revenue cycle management. The Growing US Healthcare Consulting Services Market: Key Trends and Opportunities The US Healthcare Consulting Services Market has been experiencing significant growth in recent years. This is due, in part, to the increasing complexity of the healthcare landscape and the need for expert guidance to navigate the challenges faced by healthcare providers. In this blog post, we will explore the driving forces behind the expansion of the US Healthcare Consulting Services Market and discuss the opportunities this presents for Surgeons, Physicians, Medical Billers, Medical Coders, IT Healthcare Professionals, Hospital CEOs, Healthcare Executives, Nurse Case Managers, Office Managers, Revenue Cycle Management Directors, Hospital CEOs, Hospital CFOs, Office Administrators, Healthcare Consultants, IT Consultants, Chief Nursing Officers, Medical Office Staff, Clinicians, and Medical Directors. Increasing regulations and compliance requirements One of the primary drivers of growth in the US Healthcare Consulting Services Market is the ever-changing regulatory environment. As healthcare providers face new rules and regulations, they often require the expertise of healthcare consultants to ensure compliance and avoid costly penalties. This creates a continuous demand for consulting services, as providers need guidance on how to navigate these complex requirements. Shift towards value-based care The transition to value-based care models has led to significant changes in the US Healthcare Consulting Services Market. Healthcare providers are now seeking the assistance of consulting firms to optimize patient outcomes while reducing costs. This transformation has created a need for consulting services that can help providers adapt their practices to align with new payment models and performance metrics. Technological advancements and digitalization As technology continues to evolve, the US Healthcare Consulting Services Market has seen an increased demand for IT consulting services. Healthcare organizations require assistance in implementing new technologies, such as electronic health records (EHRs), telemedicine platforms, and data analytics tools. Additionally, there is a growing need for cybersecurity consulting as healthcare providers face an increasing number of cyber threats. Mergers and acquisitions The US Healthcare Consulting Services Market has also been impacted by the growing trend of mergers and acquisitions within the healthcare industry. As healthcare providers consolidate, they often require the services of healthcare consultants to assist with integration, financial planning, and operational efficiencies. Workforce challenges The US Healthcare Consulting Services Market is poised to benefit from the ongoing challenges faced by healthcare providers in managing their workforce. Issues such as clinician burnout, staff turnover, and the need for ongoing training and education create opportunities for healthcare consultants to offer valuable expertise and support. Revenue cycle management and financial optimization The US Healthcare Consulting Services Market continues to thrive as healthcare providers seek assistance with revenue cycle management and financial optimization. Consultants can offer guidance on improving billing and coding processes, negotiating payer contracts, and identifying new revenue streams, all of which contribute to financial stability and growth for healthcare organizations. The US Healthcare Consulting Services Market offers numerous opportunities for professionals within the healthcare industry. As the landscape continues to evolve, the demand for expert guidance and support will only continue to grow. By staying informed of these key trends and challenges, Surgeons, Physicians, Medical Billers, Medical Coders, IT Healthcare Professionals, Hospital CEOs, Healthcare Executives, Nurse Case Managers, Office Managers, Revenue Cycle Management Directors, Hospital CEOs, Hospital CFOs, Office Administrators, Healthcare Consultants, IT Consultants, Chief Nursing Officers, Medical Office Staff, Clinicians, and Medical Directors can position themselves to take advantage of the expanding US Healthcare Consulting Services Market and improve the overall quality of care for their patients.
CPT Codes for Psychological Testing in Pain Management: A Comprehensive Guide Psychological testing is a crucial aspect of pain management, especially when it comes to chronic pain conditions. It helps physicians understand the underlying psychological factors that contribute to pain and develop a comprehensive treatment plan. Proper coding of psychological testing procedures is important for accurate billing and reimbursement. In this article, we will discuss the CPT codes used for psychological testing in pain management. CPT Code 96130: CPT code 96130 is used for psychological testing evaluation services by a physician or other qualified healthcare professional. This code includes the administration and interpretation of standardized tests and measures, and the integration of the data into a diagnostic and treatment plan. CPT Code 96131: CPT code 96131 is used for psychological testing evaluation services by a technician or other qualified healthcare professional. This code includes the administration and scoring of standardized tests and measures, with subsequent communication of results and integration of data into a diagnostic and treatment plan by a physician or other qualified healthcare professional. CPT Code 96136: CPT code 96136 is used for psychological or neuropsychological testing administered by a computer with qualified healthcare professional interpretation and report. This code includes the administration of the test, the interpretation of the results, and the preparation of a report. CPT Code 96137: CPT code 96137 is used for psychological or neuropsychological testing administered by a technician with qualified healthcare professional interpretation and report. This code includes the administration of the test, the scoring of the results, and subsequent communication of results and integration of data into a diagnostic and treatment plan by a physician or other qualified healthcare professional. Proper coding of psychological testing procedures is critical for accurate billing and reimbursement in pain management. Healthcare providers should be familiar with the CPT codes used for psychological testing and ensure that they are coded accurately to avoid potential claim denials. By using the correct CPT codes, healthcare providers can ensure accurate billing and reimbursement for psychological testing procedures. It is important to note that these codes may vary depending on the type of psychological testing performed and the specific circumstances of the patient. Therefore, it is recommended that healthcare providers consult the latest coding guidelines and seek professional coding advice as needed to ensure accurate billing and reimbursement. The Benefits of Medical Billing Software for Solo Practitioners: A Comprehensive Guide Medical billing is a crucial aspect of any healthcare practice, including solo practitioners. However, the process can be time-consuming and prone to errors. Medical billing software can help streamline the process and improve efficiency, accuracy, and revenue. In this article, we will discuss the benefits of medical billing software for solo practitioners. Improved Efficiency: Medical billing software automates many of the tasks involved in the billing process, such as claim submissions, payment posting, and patient billing. This frees up time for solo practitioners to focus on patient care and other important tasks. Increased Accuracy: Medical billing software reduces the risk of errors in the billing process, such as coding mistakes, claim denials, and incorrect billing. This helps to ensure accurate and timely reimbursement, which is critical for the financial health of solo practices. Enhanced Revenue: Medical billing software can help solo practitioners increase their revenue by reducing the number of claim denials, improving collections, and optimizing reimbursement rates. This can have a significant impact on the bottom line of solo practices. Improved Patient Experience: Medical billing software can improve the patient experience by providing easy-to-understand billing statements and offering online payment options. This can help to reduce patient frustration and improve patient satisfaction, which is important for patient retention and practice growth. Medical billing software offers numerous benefits for solo practitioners, including improved efficiency, increased accuracy, enhanced revenue, and improved patient experience. Solo practitioners should consider investing in medical billing software to streamline their billing process, reduce errors, and improve financial performance. With the right medical billing software, solo practitioners can focus on providing quality patient care while ensuring accurate and timely reimbursement. 5 Steps for Effective Prior Authorization Appeals Prior authorization is a process used by insurance companies to determine whether they will cover a specific medical procedure, test, or medication. Unfortunately, prior authorization requests are often denied, which can be frustrating and time-consuming for both healthcare providers and patients. In this article, we will discuss five steps for effective prior authorization appeals. Understand the Denial Before appealing a prior authorization denial, it's essential to understand why the request was denied. This includes reviewing the insurance company's reason for denial and any documentation they provided. Gather Information To appeal a prior authorization denial, it's crucial to gather all relevant information. This includes the patient's medical records, the specific procedure or medication being requested, and any other relevant documentation. Submit a Detailed Appeal When submitting a prior authorization appeal, it's essential to provide a detailed explanation of why the procedure, test, or medication is necessary. This includes providing any relevant medical literature or studies that support the request. Follow Up After submitting a prior authorization appeal, it's essential to follow up with the insurance company regularly. This includes calling to check on the status of the appeal and providing any additional information they may request. Consider Outside Help If prior authorization appeals are becoming a significant issue for your medical practice, it may be worth considering outside help. This can include hiring a third-party vendor or consultant to manage prior authorization appeals on your behalf. Prior authorization denials can be frustrating and time-consuming for healthcare providers and patients. By following these five steps for effective prior authorization appeals, healthcare providers can increase their chances of receiving approval for necessary procedures, tests, and medications. Remember to understand the denial, gather information, submit a detailed appeal, follow up, and consider outside help if necessary. By doing so, you can ensure that your patients receive the care they need, while minimizing the administrative burden on your medical practice. Enhance Your Practice with Full-Spectrum RCM Services for Interventional Pain Management Interventional pain management is a growing field in healthcare, offering patients relief from chronic pain through minimally invasive procedures. However, managing the revenue cycle for an interventional pain management practice can be complex and time-consuming. Full-Spectrum RCM Services for Interventional Pain Management, like those offered by GoHealthcare Practice Solutions, are designed to help practices streamline their revenue cycle management, allowing physicians to focus on providing exceptional patient care. The Importance of Full-Spectrum RCM Services for Interventional Pain Management Full-Spectrum RCM Services for Interventional Pain Management are essential to the financial success and stability of a practice. These services encompass every aspect of the revenue cycle, from patient registration and eligibility verification to billing, coding, and collections. By utilizing Full-Spectrum RCM Services for Interventional Pain Management, practices can ensure that their revenue cycle is optimized for maximum efficiency and profitability. Key Components of Full-Spectrum RCM Services for Interventional Pain Management
In conclusion, Full-Spectrum RCM Services for Interventional Pain Management are essential to the success of any interventional pain management practice. GoHealthcare Practice Solutions offers comprehensive, tailored solutions to help practices navigate the complexities of the revenue cycle, allowing physicians to focus on providing exceptional patient care. By partnering with GoHealthcare Practice Solutions for your Full-Spectrum RCM Services for Interventional Pain Management needs, you can be confident that your practice is in capable hands, ensuring financial stability and success for years to come. Mastering Healthcare Financial Management for Orthopedic Surgeons: The Key to a Successful Practice3/22/2023 Mastering Healthcare Financial Management for Orthopedic Surgeons: The Key to a Successful Practice In today's competitive healthcare landscape, effective Healthcare Financial Management for Orthopedic Surgeons is more critical than ever. Balancing quality patient care with the complexities of medical billing, insurance navigation, and revenue cycle management can be challenging. This article explores the importance of Healthcare Financial Management for Orthopedic Surgeons and how GoHealthcare Practice Solutions can support your practice's financial success. The Importance of Healthcare Financial Management for Orthopedic Surgeons Healthcare Financial Management for Orthopedic Surgeons plays a significant role in the overall success of a practice. As an orthopedic surgeon, you are responsible for providing exceptional patient care while ensuring that your practice remains financially viable. Effective Healthcare Financial Management for Orthopedic Surgeons allows you to focus on what you do best—delivering outstanding care to your patients—while your practice remains profitable and compliant with ever-changing healthcare regulations. Challenges in Healthcare Financial Management for Orthopedic Surgeons Navigating the complexities of Healthcare Financial Management for Orthopedic Surgeons can be a daunting task. Some common challenges include managing billing and coding, coordinating insurance benefits, handling out-of-network and in-network providers, and staying compliant with HIPAA and other regulations. These challenges can be time-consuming and may detract from your primary focus: providing excellent patient care. The GoHealthcare Practice Solutions Advantage GoHealthcare Practice Solutions specializes in Healthcare Financial Management for Orthopedic Surgeons, offering comprehensive and customized solutions to help your practice thrive. Our experienced team understands the unique financial needs of orthopedic surgery practices and provides a wide range of services, including revenue cycle management, medical billing and coding, insurance navigation, and more. Customized Solutions for Healthcare Financial Management for Orthopedic Surgeons At GoHealthcare Practice Solutions, we know that no two practices are alike. That's why we tailor our Healthcare Financial Management for Orthopedic Surgeons services to meet your practice's specific needs. Our customized solutions help you optimize your revenue cycle, streamline your workflow, and ensure compliance with healthcare regulations. Expert Support for Healthcare Financial Management for Orthopedic Surgeons Partnering with GoHealthcare Practice Solutions means you'll have a team of experts by your side, dedicated to the success of your practice. Our knowledgeable staff has extensive experience in Healthcare Financial Management for Orthopedic Surgeons and is committed to helping you overcome the financial challenges that come with running a successful practice. A Comprehensive Approach to Healthcare Financial Management for Orthopedic Surgeons At GoHealthcare Practice Solutions, we believe that effective Healthcare Financial Management for Orthopedic Surgeons requires a comprehensive approach. We offer a wide range of services, from patient registration and eligibility verification to insurance benefit coordination and payment plan setup. Our commitment to comprehensive Healthcare Financial Management for Orthopedic Surgeons ensures that your practice is well-equipped to navigate the complex world of healthcare finance. In conclusion, effective Healthcare Financial Management for Orthopedic Surgeons is essential for the success of your practice. By partnering with GoHealthcare Practice Solutions, you can focus on providing exceptional patient care while we handle the financial complexities. Our customized solutions, expert support, and comprehensive approach to Healthcare Financial Management for Orthopedic Surgeons make us the ideal partner for your practice. To learn more about how GoHealthcare Practice Solutions can help you achieve financial success, visit our website at https://www.gohealthcarellc.com. Enhancing Patient Care with Interventional Pain Management Practice Support Interventional pain management has become a rapidly growing field, offering relief to millions of patients suffering from chronic pain. To effectively serve patients and streamline operations, practices need access to specialized Interventional Pain Management Practice Support. GoHealthcare Practice Solutions is at the forefront of providing comprehensive, tailored services designed to enhance patient care and optimize practice performance. Understanding the Need for Interventional Pain Management Practice Support In recent years, the demand for non-surgical, minimally invasive treatments for pain has skyrocketed, increasing the need for dedicated Interventional Pain Management Practice Support. GoHealthcare Practice Solutions understands that a well-functioning practice is essential to providing the best possible patient care. Our Interventional Pain Management Practice Support services cater to the unique needs of pain management clinics. We work closely with your practice to identify areas of improvement and implement strategies that streamline processes, reduce overhead, and optimize patient outcomes. Comprehensive Services Offered by GoHealthcare Practice Solutions GoHealthcare Practice Solutions' Interventional Pain Management Practice Support includes a wide array of services to enhance your practice's performance:
The GoHealthcare Practice Solutions Advantage Choosing GoHealthcare Practice Solutions for your Interventional Pain Management Practice Support means partnering with a team of experienced professionals who understand the intricacies of your field. Our specialized knowledge and commitment to innovation make us the ideal choice for Interventional Pain Management Practice Support. With our help, your practice can thrive and continue to provide exceptional patient care. In conclusion, GoHealthcare Practice Solutions is your one-stop solution for comprehensive Interventional Pain Management Practice Support. With a focus on enhancing patient care and optimizing practice performance, our team is dedicated to helping your practice achieve and maintain success. Experience the difference of working with industry experts by choosing GoHealthcare Practice Solutions for your Interventional Pain Management Practice Support needs. Best EHR Software for a Small Practice in 2023: Top Choices for Your Healthcare Team As a healthcare professional, finding the best EHR software for a small practice in 2023 is crucial to streamline your workflow and enhance the patient experience. At GoHealthcare Practice Solutions, we understand the challenges faced by small practices. With this comprehensive list, we aim to simplify your decision-making process and help you choose the best EHR software for small practices that meet your unique needs. AmazingCharts AmazingCharts is a user-friendly EHR system designed to cater to small practices. With its intuitive interface and robust features, it is an excellent choice for clinicians seeking the best EHR software for a small practice in 2023. AmazingCharts offers customizable templates, integrated practice management software, and secure patient communication portals to streamline your workflow. Kareo Kareo is another top contender for the best EHR software for small practices in 2023. This cloud-based platform offers a complete solution, combining EHR, practice management software, and medical billing services. Kareo's user-friendly interface and customizable features make it suitable for various medical specialties and staff roles, including office administrators and nurse case managers. Athenahealth Athenahealth is a popular choice for the best EHR software for a small practice in 2023, as it offers a comprehensive suite of cloud-based services, including EHR, practice management, and patient engagement tools. With its revenue cycle management capabilities, Athenahealth is well-suited for medical billers, coders, and revenue cycle management directors. eClinicalWorks As one of the best EHR software for small practices, eClinicalWorks provides a comprehensive suite of EHR and practice management solutions. Its robust features cater to various healthcare professionals, including office managers, healthcare consultants, and chief nursing officers. With its patient engagement tools and interoperability capabilities, eClinicalWorks can improve care coordination and patient satisfaction. Greenway Health Greenway Health's EHR, Intergy, is an excellent choice for the best EHR software for a small practice in 2023. With its intuitive interface and comprehensive features, Intergy is suitable for various medical specialties and roles, such as clinicians, surgery schedulers, and prior authorization experts. Additionally, Greenway Health offers revenue cycle management services and practice analytics to optimize your financial performance. Selecting the best EHR software for a small practice in 2023 can be a daunting task, but this list aims to make the decision easier for you and your team. By considering factors like ease of use, customization, and integration with other systems, you can find the best EHR software for small practices that fit your unique needs. At GoHealthcare Practice Solutions, we are committed to helping healthcare professionals succeed in their practice. Whether you're a physician, office administrator, or medical director, our goal is to provide you with the resources and support you need to thrive. You are going to love our amazing team! So visit our website at https://www.gohealthcarellc.com to learn more about our services and how we can help your practice reach new heights in 2023. 10 Proven Strategies for Boosting Interventional Pain Management Practice Revenue As the demand for interventional pain management continues to increase, so does the need for pain management practices to find ways to boost revenue. If you own or manage a pain management practice, you're probably always on the lookout for effective strategies to increase your bottom line. Here are ten proven strategies for boosting interventional pain management practice revenue: Improve patient engagement: Engaged patients are more likely to follow through with treatment plans and refer others to your practice, which can ultimately lead to increased revenue. Consider implementing patient education programs, offering incentives for referrals, and ensuring that your staff provides excellent customer service. Expand your services: Offer additional services, such as physical therapy or acupuncture, to attract new patients and increase revenue from existing patients. This can help differentiate your practice from competitors and provide additional revenue streams. Implement technology solutions: Adopt technology solutions that streamline administrative tasks, such as electronic medical records (EMRs), online appointment scheduling, and patient portals. This can help reduce staff workload and increase efficiency, ultimately boosting revenue. Focus on marketing: Invest in marketing efforts that reach your target audience, such as social media advertising, search engine optimization, and targeted email campaigns. A well-executed marketing strategy can increase patient volume and boost revenue. Optimize billing and collections: Ensure that your billing and collections processes are efficient and effective. This can include streamlining processes, optimizing collections, and leveraging technology solutions. Leverage data analytics: Use data analytics tools to gain insights into your practice's revenue drivers, patient demographics, and more. This can help you make data-driven decisions to optimize revenue. Develop referral partnerships: Establish referral partnerships with other healthcare providers, such as primary care physicians or surgeons. This can help increase patient volume and revenue. Implement telehealth services: Offer telehealth services to expand your reach beyond your local area and provide convenient care to patients. This can help increase patient volume and revenue. Develop a cash-pay program: Consider developing a cash-pay program that offers discounted rates for patients who pay in full at the time of service. This can provide a new revenue stream and incentivize patients to choose your practice. Partner with GoHealthcare Practice Solutions: GoHealthcare Practice Solutions is a healthcare consulting firm that can help pain management practices optimize revenue through a range of services, including revenue cycle management, billing and coding, and practice management consulting. Their expertise can help your practice improve revenue and reduce administrative burdens, ultimately leading to increased profitability. In conclusion, boosting interventional pain management practice revenue requires a multifaceted approach that includes improving patient engagement, expanding services, adopting technology solutions, optimizing billing and collections, leveraging data analytics, developing referral partnerships, implementing telehealth services, developing a cash-pay program, and partnering with a healthcare consulting firm like GoHealthcare Practice Solutions. By implementing these strategies, you can achieve long-term financial stability and success for your practice. The Top Benefits of Implementing Prior Authorization in Interventional Pain Management As healthcare costs continue to rise, it's essential to find ways to reduce expenses without sacrificing patient care. One effective strategy is to implement prior authorization in interventional pain management. Prior authorization is a process that requires healthcare providers to get approval from an insurance company before performing specific treatments or procedures. In this blog post, we'll discuss the top benefits of implementing prior authorization in interventional pain management and how GoHealthcare Practice Solutions can help. Reduces Cost: One of the most significant benefits of prior authorization is the reduction in healthcare costs. By implementing this process, healthcare providers can ensure that only necessary treatments are performed, which can prevent unnecessary procedures and associated costs. GoHealthcare Practice Solutions can assist with prior authorization by streamlining the process and reducing administrative burden, allowing healthcare providers to focus on patient care. Ensures Quality of Care: Prior authorization can help ensure that patients receive appropriate care. Insurance companies have established criteria that must be met before approving a treatment or procedure. These criteria ensure that patients receive the right treatment at the right time, improving patient outcomes. GoHealthcare Practice Solutions provides access to expert medical professionals who can provide guidance on appropriate treatment options and help navigate the prior authorization process. Improves Communication: Prior authorization requires communication between healthcare providers and insurance companies. This process can help improve communication and collaboration between healthcare providers and insurers, leading to better patient outcomes. GoHealthcare Practice Solutions offers a cloud-based platform that allows healthcare providers and insurers to communicate efficiently, reducing delays and improving patient care. Minimizes Errors: Prior authorization can help minimize errors by ensuring that patients receive the right treatment at the right time. Insurance companies have established guidelines for treatments and procedures, reducing the risk of errors or complications. GoHealthcare Practice Solutions offers an advanced analytics platform that helps identify potential errors and risks, allowing healthcare providers to proactively address them. Reduces Administrative Burden: Prior authorization can be a time-consuming and complex process that can take away from patient care. GoHealthcare Practice Solutions offers a range of administrative services, including prior authorization support, allowing healthcare providers to focus on patient care rather than administrative tasks. In conclusion, implementing prior authorization in interventional pain management offers many benefits, including reducing costs, ensuring quality of care, improving communication, minimizing errors, and reducing administrative burden. GoHealthcare Practice Solutions offers a range of services to assist with prior authorization, streamlining the process and allowing healthcare providers to focus on patient care. EHR Software Designed for Billing and Coding Accuracy: Top Benefits for Your Medical Practice3/22/2023 EHR Software Designed for Billing and Coding Accuracy: Top Benefits for Your Medical Practice The success of any medical practice depends on the efficiency and accuracy of its billing and coding system. One of the most effective ways to achieve this is by utilizing EHR software designed for billing and coding accuracy. In this blog post, we will explore the top benefits of using EHR software designed for billing and coding accuracy for a wide range of professionals, including surgeons, physicians, medical billers, coders, and hospital CEOs. Improved Accuracy and Efficiency EHR software designed for billing and coding accuracy helps minimize human errors, which can lead to billing discrepancies and claim denials. By automating the process, these specialized EHR systems reduce the likelihood of incorrect codes being used, resulting in faster and more accurate claims processing. This ultimately improves the overall revenue cycle management and ensures that your practice gets paid faster. Enhanced Compliance Healthcare providers must adhere to strict regulations, such as HIPAA and ICD-10, to avoid penalties and maintain patient trust. EHR software designed for billing and coding accuracy helps providers stay compliant with industry standards by streamlining the entire billing and coding process. This ensures that your practice remains compliant, reducing the risk of audits and fines. Increased Patient Satisfaction By streamlining the billing and coding process, EHR software designed for billing and coding accuracy allows healthcare professionals to focus more on patient care. This results in a better patient experience, which can lead to increased patient satisfaction and loyalty. Better Decision-Making With EHR software designed for billing and coding accuracy, healthcare professionals have access to real-time data, which is crucial for making informed decisions. This data can be used by clinicians, medical directors, and nurse case managers to improve patient care and optimize workflow efficiency. Additionally, hospital CEOs and CFOs can use the data to make strategic financial decisions for their organizations. Streamlined Communication EHR software designed for billing and coding accuracy promotes better communication between healthcare professionals, including office managers, medical office staff, and chief nursing officers. These systems provide a centralized platform for sharing information, making it easier to collaborate and coordinate patient care. This leads to a more efficient and effective healthcare system. Customization and Scalability Different medical practices have unique needs, and EHR software designed for billing and coding accuracy is no exception. These systems offer customization options to fit the specific requirements of your practice, whether you are a small private clinic or a large hospital. As your practice grows, the software can be easily scaled to meet your expanding needs, ensuring a seamless transition. Comprehensive Training and Support Implementing a new EHR system can be challenging, especially for IT healthcare professionals. EHR software designed for billing and coding accuracy providers typically offer comprehensive training and ongoing support to ensure a smooth transition and user adoption. This helps healthcare professionals feel confident and proficient in using the new system. Investing in EHR software designed for billing and coding accuracy is a smart decision for any medical practice. The benefits, such as improved accuracy, enhanced compliance, better decision-making, streamlined communication, customization, scalability, increased patient satisfaction, and comprehensive training and support, make it an essential tool for healthcare professionals. By integrating this software into your practice, you can optimize your billing and coding processes, leading to a more efficient and profitable medical practice. EHR software for improved revenue cycle management: 8 Key Features to Optimize Your Workflow3/22/2023 EHR software for improved revenue cycle management: 8 Key Features to Optimize Your Workflow The healthcare industry is constantly evolving, and so are the tools and technology used to manage patient care and streamline administrative processes. EHR software for improved revenue cycle management has become an essential part of many healthcare organizations, as it provides significant advantages in efficiency and financial performance. This post will discuss eight essential features of EHR software for improved revenue cycle management that can benefit a wide range of healthcare professionals, including surgeons, physicians, medical billers, medical coders, IT healthcare professionals, hospital CEOs, healthcare executives, nurse case managers, office managers, revenue cycle management directors, hospital CFOs, office administrators, chief nursing officers, medical office staff, clinicians, and medical directors. Centralized billing and claims management: One of the primary functions of EHR software for improved revenue cycle management is the ability to centralize billing and claims management. This feature consolidates all billing and claims data in one place, making it easier for medical billers and coders to access, update, and track claims in real-time. The result is a more efficient billing process, with fewer errors and faster reimbursements. Automated coding and charge capture: EHR software for improved revenue cycle management often includes tools to automate coding and charge capture. These tools help ensure that medical coders accurately assign codes to patient encounters and procedures, reducing the risk of coding errors and billing discrepancies. This not only improves the accuracy of your organization's revenue cycle but also reduces the likelihood of claim denials and payment delays. Comprehensive reporting and analytics: EHR software for improved revenue cycle management should include robust reporting and analytics capabilities. This allows healthcare executives, hospital CEOs, and revenue cycle management directors to access detailed financial data and gain valuable insights into their organization's revenue cycle performance. Such information helps identify trends, pinpoint inefficiencies, and develop targeted strategies for improvement. Integration with other healthcare software systems: Integration is essential when selecting EHR software for improved revenue cycle management. The ability to seamlessly connect with other software systems, such as practice management solutions and billing platforms, ensures that all relevant data is readily available when needed. This streamlines the entire revenue cycle process, from patient registration to final payment. Patient portal for online payments and communication: A patient portal is an invaluable feature of EHR software for improved revenue cycle management. Through the portal, patients can securely access their health records, schedule appointments, request prescription refills, and make payments online. This convenience not only improves patient satisfaction but also reduces administrative work for medical office staff and helps ensure timely payments. Payer contract management: Managing payer contracts can be a complex and time-consuming process. EHR software for improved revenue cycle management simplifies this task by providing tools to track and manage payer contracts, fee schedules, and reimbursement rates. This helps hospital CFOs and revenue cycle management directors stay on top of changing payment models and negotiate more favorable terms with insurance companies. Denial management and appeals: EHR software for improved revenue cycle management should offer tools to help healthcare organizations efficiently manage denials and appeals. This includes tracking denied claims, identifying trends in denials, and streamlining the appeal process. By addressing denials proactively, healthcare providers can recover lost revenue and improve their overall financial performance. Security and regulatory compliance: Lastly, EHR software for improved revenue cycle management must prioritize security and regulatory compliance. This includes protecting sensitive patient information, ensuring HIPAA compliance, and staying up to date with evolving industry regulations. By choosing software with robust security features, healthcare organizations can minimize the risk of data breaches and maintain the trust of their patients and partners. Top 8 Advantages of User-friendly EHR with Billing and Coding Automation for Your Healthcare Practice As a healthcare professional, you're always on the lookout for ways to optimize your practice's efficiency, productivity, and patient care. User-friendly EHR with billing and coding automation is a game-changing solution that can address these needs. This blog post will dive into the top 8 advantages of implementing user-friendly EHR with billing and coding automation for various healthcare stakeholders, from surgeons and physicians to hospital CEOs and office administrators. Streamlined Billing and Coding Process User-friendly EHR with billing and coding automation helps simplify the complex billing and coding process, eliminating manual data entry and reducing the likelihood of errors. This efficient system ensures a more accurate and timely submission of claims, reducing claim denials and ensuring your practice receives the reimbursements it deserves. Enhanced Revenue Cycle Management A user-friendly EHR with billing and coding automation integrates seamlessly with revenue cycle management systems, providing greater visibility into the financial aspects of your practice. It enables better tracking of patient accounts and claims, improving cash flow and reducing the time spent on financial tasks. Improved Patient Care User-friendly EHR with billing and coding automation allows healthcare professionals to focus on providing top-notch patient care. By reducing the administrative burden, physicians, nurses, and clinicians can dedicate more time to their patients, ultimately leading to improved patient satisfaction and better health outcomes. Time-saving Features With user-friendly EHR with billing and coding automation, healthcare professionals can access patient information quickly and easily, saving valuable time. Furthermore, automation tools can help reduce the time spent on administrative tasks, such as entering billing codes and managing insurance claims. Seamless Integration with Other Systems User-friendly EHR with billing and coding automation is designed to integrate seamlessly with other systems in your practice, including scheduling, reporting, and patient portals. This enables a more streamlined workflow and ensures that all aspects of your practice are running efficiently. Efficient Medical Documentation The user-friendly EHR with billing and coding automation ensures complete and accurate medical documentation. This can help healthcare providers make well-informed decisions about patient care, as well as facilitate better communication among providers and improve the overall quality of care. Increased Compliance and Security The user-friendly EHR with billing and coding automation adheres to strict security and privacy standards, ensuring that your practice remains compliant with industry regulations. This not only protects your patients' sensitive data but also helps avoid potential legal issues. Customizable to Suit Your Practice Every healthcare practice is unique, and user-friendly EHR with billing and coding automation can be tailored to suit your specific needs. This flexibility allows you to choose the features and integrations that best align with your practice's goals and requirements. In conclusion, investing in a user-friendly EHR with billing and coding automation can offer numerous benefits for your healthcare practice. From streamlining the billing process to improving patient care, this solution can help you achieve greater efficiency, productivity, and satisfaction among your staff and patients alike. Consider implementing user-friendly EHR with billing and coding automation to stay ahead in the ever-evolving healthcare landscape. Top Considerations for Choosing the Best FQHC EMR Software: A Comprehensive Guide As Federally Qualified Health Centers (FQHCs) continue to grow, it's becoming increasingly necessary to have the best EMR software for small practices. EMR (Electronic Medical Record) software is an essential tool for any healthcare organization as it allows for easy management of patient information, improves workflow efficiency, and reduces errors in medical care. In this post, we'll discuss the top considerations for choosing the best FQHC EMR software. Scalability: As your FQHC grows, so will your patient volume. Therefore, it's crucial to choose an EMR system that can scale with your organization's growth. Look for EMR software that offers customizable templates and workflows that can be tailored to your organization's needs. Cloud-based EMR Software Solutions: Cloud-based EMR software solutions provide easy access to patient data and practice management tools from anywhere with an internet connection. This is particularly beneficial for FQHCs with multiple locations as it enables practitioners to access patient data from anywhere at any time. Specialty-specific EMR Software Providers: Every FQHC has different needs when it comes to EMR software. Therefore, it's essential to choose an EMR software provider that specializes in the needs of your particular specialty. For instance, some providers offer EMR software specifically designed for primary care, while others provide solutions for behavioral health. User-friendly interface: The interface of the EMR software should be user-friendly and easy to navigate. The system should be intuitive and easy to learn, reducing the need for extensive training for staff. Security: FQHCs are held to high standards of security compliance, and patient data must be kept secure. Therefore, choose an EMR software that is HIPAA compliant and has robust security features such as two-factor authentication, encryption, and data backup. Integration: An EMR system with integrated billing and coding can streamline billing processes and reduce errors. Look for a system that integrates with your current billing and coding software to reduce double data entry. Mobile accessibility: With the rise of mobile devices in healthcare, it's essential to choose an EMR software that is mobile-friendly. This allows practitioners to access patient data and manage practice workflows from their mobile devices. Customizability: Customization of the EMR software can enhance the user experience by tailoring the system to the organization's specific needs. Look for EMR software that allows customization of templates, workflows, and reporting features. Technical support: The EMR software provider should offer excellent technical support to assist with any issues that may arise. Look for providers that offer 24/7 support and a dedicated customer support team. Pricing: Finally, consider the pricing model of the EMR software. Look for providers that offer transparent pricing and avoid hidden fees. Ensure that the pricing model aligns with your organization's budget and growth plans. Choosing the best EMR software for small practices is a critical decision for FQHCs. By considering the above factors, FQHCs can choose the top-rated electronic medical record systems that best suit their organization's needs. An effective EMR system can improve workflow efficiency, patient care, and billing processes, ultimately enhancing the overall quality of care provided to patients. Top 10 Considerations for Choosing the Best Pain Clinic EMR Software As a pain clinic owner or manager, choosing the right electronic medical record (EMR) software is critical to the success of your practice. The right software can streamline your operations, improve patient care, and increase revenue. However, with so many options available in the market, it can be overwhelming to make the right decision. In this article, we will highlight the top considerations to help you choose the best EMR software for small practices that cater specifically to pain management. Cloud-Based EMR Software Solutions Cloud-based EMR software solutions provide flexibility and accessibility. With cloud-based EMR software, your patient records can be accessed from anywhere, at any time, making it easier for your staff to collaborate on patient care. Additionally, cloud-based software is more cost-effective than traditional software solutions, as you don't have to pay for expensive hardware, software installation, or maintenance. Speciality-Specific EMR Software Providers Specialty-specific EMR software providers cater to specific medical fields, such as pain management. These software providers have a deep understanding of the unique needs of pain clinics, making it easier for you to customize your software to fit your practice's specific requirements. Specialty-specific EMR software providers also ensure that your software is up-to-date with the latest compliance standards and regulations. EMR Software with Integrated Billing and Coding EMR software with integrated billing and coding can help reduce errors and streamline your billing process. By integrating billing and coding into your EMR software, you can automate the billing process, reducing the risk of errors and saving time. Additionally, integrated billing and coding can improve your revenue cycle by reducing the number of denied claims and improving your collection rates. Easy-to-Use EMR Software Choosing an easy-to-use EMR software is essential to ensure that your staff can quickly and easily navigate the software. User-friendly software can reduce the risk of errors, increase staff productivity, and improve patient care. Additionally, easy-to-use software can save you time and money on training costs. Customizable EMR Templates Customizable EMR templates can help improve patient care by ensuring that your staff can quickly and accurately document patient information. Customizable templates can be tailored to fit your practice's specific needs, making it easier for your staff to document patient information accurately. EMR Software with Robust Reporting Features EMR software with robust reporting features can help you track your practice's performance, identify trends, and make informed decisions. Robust reporting features can provide insights into your practice's revenue, patient demographics, and referral sources, helping you optimize your operations and improve patient care. HIPAA Compliance HIPAA compliance is critical to ensure that your patient data is secure and protected. Choosing an EMR software provider that is HIPAA compliant can help you avoid costly fines and penalties. Additionally, HIPAA-compliant software can provide peace of mind, knowing that your patient data is safe and secure. EMR Software with Patient Portal EMR software with a patient portal can help improve patient engagement and satisfaction. Patient portals allow patients to access their medical records, view test results, schedule appointments, and communicate with their healthcare providers. Additionally, patient portals can improve patient compliance and reduce no-show rates. EMR Software with Mobile App EMR software with a mobile app can help your staff access patient information on the go, improving productivity and patient care. With a mobile app, your staff can quickly view patient records, schedule appointments, and communicate with patients and other healthcare providers. EMR Software with Excellent Customer Support Choosing an EMR software provider with excellent customer support can ensure that any issues or concerns are addressed quickly and efficiently. Best EHR Systems with ICD-10 and CPT Code Support: A Comprehensive Guide for Healthcare Professionals Are you looking for the best EHR systems with ICD-10 and CPT code support to streamline your healthcare organization's operations? Look no further, because in this blog post, we have compiled a list of the top EHR systems that cater to the needs of surgeons, physicians, medical billers, medical coders, IT healthcare professionals, hospital CEOs, healthcare executives, nurse case managers, office managers, revenue cycle management directors, hospital CFOs, office administrators, chief nursing officers, medical office staff, clinicians, and medical directors. Read on to discover the best EHR systems with ICD-10 and CPT code support that can revolutionize your healthcare practice! Epic Systems Epic Systems has emerged as one of the best EHR systems with ICD-10 and CPT code support, providing a comprehensive and user-friendly platform for healthcare professionals. With its robust functionality, Epic enables seamless integration of ICD-10 and CPT codes into your daily workflow, facilitating accurate billing and efficient communication with insurance companies. Cerner Cerner is another top contender in the best EHR systems with ICD-10 and CPT code support. Known for its scalability, Cerner is suitable for both small practices and large hospitals. With its intuitive interface, users can quickly search and input ICD-10 and CPT codes, reducing the chances of coding errors and enhancing revenue cycle management. Athenahealth Athenahealth is a cloud-based EHR system, making it a popular choice among the best EHR systems with ICD-10 and CPT code support. Its comprehensive database ensures that users have access to the latest ICD-10 and CPT codes, while its intelligent billing system minimizes claim denials and accelerates the reimbursement process. Allscripts Allscripts is a powerful and flexible EHR solution that ranks among the best EHR systems with ICD-10 and CPT code support. Its robust coding capabilities enable healthcare professionals to easily incorporate the latest ICD-10 and CPT codes into their documentation, ensuring accurate billing and optimal revenue cycle management. Greenway Health Greenway Health's Prime Suite is a highly customizable EHR system that offers one of the best EHR systems with ICD-10 and CPT code support. Its user-friendly interface and advanced code search capabilities allow healthcare professionals to quickly and accurately input ICD-10 and CPT codes, streamlining billing processes and improving overall efficiency. eClinicalWorks eClinicalWorks is an innovative EHR solution that has established itself as one of the best EHR systems with ICD-10 and CPT code support. Its integrated coding module facilitates accurate and efficient coding, reducing the risk of claim denials and enhancing revenue cycle management. NextGen Healthcare NextGen Healthcare is another leading provider of the best EHR systems with ICD-10 and CPT code support. With its advanced coding and billing features, NextGen ensures that healthcare professionals can easily input ICD-10 and CPT codes, streamlining their workflow and maximizing revenue. CareCloud CareCloud is a cloud-based EHR system that has earned its spot among the best EHR systems with ICD-10 and CPT code support. Its innovative coding features and advanced analytics enable healthcare professionals to improve their coding accuracy, optimize their revenue cycle, and enhance overall practice efficiency. Selecting the best EHR systems with ICD-10 and CPT code support is crucial for the success of any healthcare organization. Top Considerations for Choosing the Best EMR Software for Small Ambulatory Surgery Centers3/22/2023 Top Considerations for Choosing the Best EMR Software for Small Ambulatory Surgery Centers Ambulatory Surgery Centers (ASCs) have unique requirements when it comes to electronic medical records (EMR) software. Finding the right EMR software for your ASC can be a daunting task. With so many options available, it can be challenging to know which one will best meet the needs of your practice. In this blog post, we will discuss the top considerations you should keep in mind when choosing the best EMR software for your small Ambulatory Surgery Center. Specialization in ASCs Look for EMR software that specializes in Ambulatory Surgery Centers. These software providers understand the unique needs of ASCs and can tailor their solutions to meet those needs. They have features such as preoperative and postoperative management, inventory management, and scheduling tools that are specific to ASCs. Cloud-based Software Cloud-based EMR software solutions provide several benefits over traditional software. They are accessible from anywhere with an internet connection, secure, and allow for automatic software updates. Cloud-based software can also integrate with other software solutions, making it easier to manage your practice. User-friendly Interface The software should have a user-friendly interface that is easy to navigate. The interface should be intuitive and provide easy access to patient records, scheduling tools, and other essential features. It should also be customizable so that you can configure the software to match your workflow. Specialty-specific EMR Software Providers Specialty-specific EMR software providers are a great option for ASCs. They offer features and templates that are specific to your specialty, making it easier to document patient care. They also understand the unique challenges that your specialty faces and can provide solutions that address those challenges. Customizable Templates Customizable templates can save time and improve the accuracy of documentation. Look for software that allows you to customize templates to match your workflow and specialty. Customizable templates should also be easy to use and make it simple to document patient care. Integrated Billing and Coding EMR software with integrated billing and coding can streamline the billing process, reduce errors, and improve revenue cycle management. Look for software that integrates with your billing software or provides its own billing and coding tools. Mobile Access Mobile access is essential for ASCs. With mobile access, you can access patient records, manage schedules, and document patient care from anywhere. Look for software that has a mobile app or a mobile-friendly web interface. HIPAA Compliance HIPAA compliance is critical for ASCs. Look for software that is HIPAA compliant and provides security features such as data encryption, password protection, and audit logs. Integration with Other Software EMR software should integrate with other software solutions that you use in your practice. Look for software that integrates with your billing software, practice management software, and other tools that you use to manage your practice. Cost Finally, consider the cost of the software. Look for software that fits within your budget while providing all the features you need. Consider the upfront cost, ongoing maintenance costs, and any additional costs such as training or support. Choosing the best EMR software for your small Ambulatory Surgery Center requires careful consideration of several factors. Look for software that specializes in ASCs, is cloud-based, has a user-friendly interface, customizable templates, integrated billing and coding, mobile access, is HIPAA compliant, integrates with other software, and fits within your budget. With the right EMR software, you can streamline your workflow, improve patient care, and increase revenue. Top Considerations for Choosing the Best Dental Clinic EMR Software As a dental professional, you know that efficient management of patient data is essential for providing quality care. Electronic medical record (EMR) systems have become a necessity for dental clinics of all sizes, helping to streamline workflows and improve patient outcomes. However, choosing the best EMR software for small practices can be overwhelming, given the myriad of options available in the market. In this blog post, we will discuss the top considerations for selecting the right EMR software for your dental clinic. Functionality The first consideration when selecting an EMR system is its functionality. You need to ensure that the software is tailored to the needs of a dental practice. Look for top-rated electronic medical record systems that offer features such as scheduling, patient data management, treatment planning, and imaging. Cloud-based EMR software solutions Cloud-based EMR software solutions offer several benefits, including cost savings, automatic updates, and secure data storage. With cloud-based EMR systems, dental practices can access patient data from anywhere, at any time, using any device. Integration One of the critical benefits of an EMR system is its ability to integrate with other software, such as billing and coding software. Look for EMR software with integrated billing and coding to streamline your clinic's financial management. Specialty-specific EMR software providers Dental practices have unique needs that are different from other healthcare specialties. Therefore, it is crucial to choose an EMR software provider that specializes in dental clinics. Specialty-specific EMR software providers understand the unique needs of dental practices and can provide tailored solutions. User-friendliness The usability of an EMR system is essential, especially for dental clinics with limited IT resources. Choose EMR software that is easy to use, with a simple and intuitive interface. Customization Dental clinics have different needs, and it is essential to choose an EMR system that can be customized to meet those needs. Look for software providers that offer customization options, such as the ability to add or remove features based on your clinic's requirements Data security Data security is critical when it comes to patient information. Choose EMR software providers that comply with HIPAA regulations and offer robust security features, such as data encryption and two-factor authentication. Technical support When selecting an EMR software provider, consider the level of technical support they offer. Choose providers that offer 24/7 technical support, regular software updates, and training resources to ensure that your clinic can fully utilize the software. Pricing Pricing is an essential consideration when selecting EMR software. Look for software providers that offer transparent pricing with no hidden costs or long-term contracts. Reputation and reviews Finally, research the reputation of the EMR software provider and read reviews from other dental practices to gauge the quality of their products and services. Look for providers with a proven track record of delivering high-quality and reliable software solutions. In conclusion, choosing the best EMR software for small practices is a critical decision that requires careful consideration. Consider functionality, cloud-based solutions, integration, specialty-specific providers, user-friendliness, customization, data security, technical support, pricing, and reputation when making your decision. By doing so, you can ensure that you select the right EMR software that meets your dental practice's unique needs and helps you deliver quality care to your patients. Top 5 EHR Software for Seamless Medical Coding and Billing In today's fast-paced healthcare industry, the need for EHR software for seamless medical coding and billing has become more vital than ever. By streamlining the process, EHR software for seamless medical coding and billing helps improve efficiency and reduce errors. This ultimately leads to increased revenue and improved patient care. In this blog post, we will explore the top 5 EHR software options for seamless medical coding and billing that cater to the needs of various healthcare professionals. EHR Software for Seamless Medical Coding and Billing: Epic Epic is a comprehensive EHR software for seamless medical coding and billing that is widely used by large hospitals, clinics, and healthcare systems. The software offers a wide range of features, including electronic medical records (EMRs), practice management, and billing, making it a popular choice among healthcare professionals. Epic's interoperability capabilities make it easier to exchange data between different healthcare organizations, thereby increasing efficiency and reducing errors in the billing process. EHR Software for Seamless Medical Coding and Billing: Cerner Cerner is another top contender in the EHR software for seamless medical coding and billing market. This software is designed for both large and small healthcare organizations, making it suitable for a diverse range of healthcare professionals. Cerner's robust medical coding and billing features are complemented by its easy-to-use interface, making it an excellent choice for users seeking an efficient and user-friendly solution. EHR Software for Seamless Medical Coding and Billing: NextGen NextGen is an EHR software for seamless medical coding and billing that focuses on providing an easy-to-use, comprehensive solution for healthcare professionals. The software offers extensive medical coding and billing features, as well as powerful analytics and reporting capabilities. NextGen's intuitive interface makes it simple for users to navigate and manage their medical coding and billing tasks, ensuring a smoother experience for all involved. EHR Software for Seamless Medical Coding and Billing: athenahealth athenahealth is a cloud-based EHR software for seamless medical coding and billing that is known for its easy implementation and scalability. The software is designed to help healthcare professionals manage their medical coding and billing tasks more efficiently, with features such as automated claim scrubbing and real-time eligibility checking. With athenahealth's cloud-based platform, healthcare organizations can easily scale their operations as they grow, making it an excellent choice for those looking for a future-proof solution. EHR Software for Seamless Medical Coding and Billing: Kareo Kareo is an affordable EHR software for seamless medical coding and billing that caters specifically to small practices and independent healthcare providers. The software offers an array of features, including practice management, electronic health records, and billing, all designed to streamline the medical coding and billing process. With Kareo's user-friendly interface and affordable pricing, it's an excellent option for small practices looking to improve their medical coding and billing processes. EHR software for seamless medical coding and billing is a game-changer for healthcare professionals in today's competitive market. By investing in the right EHR software for seamless medical coding and billing, healthcare organizations can significantly improve their operational efficiency, reduce errors, and boost revenue. The top 5 EHR software options mentioned above cater to the needs of a diverse range of healthcare professionals, making it easier than ever to find the perfect solution for your organization. |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985

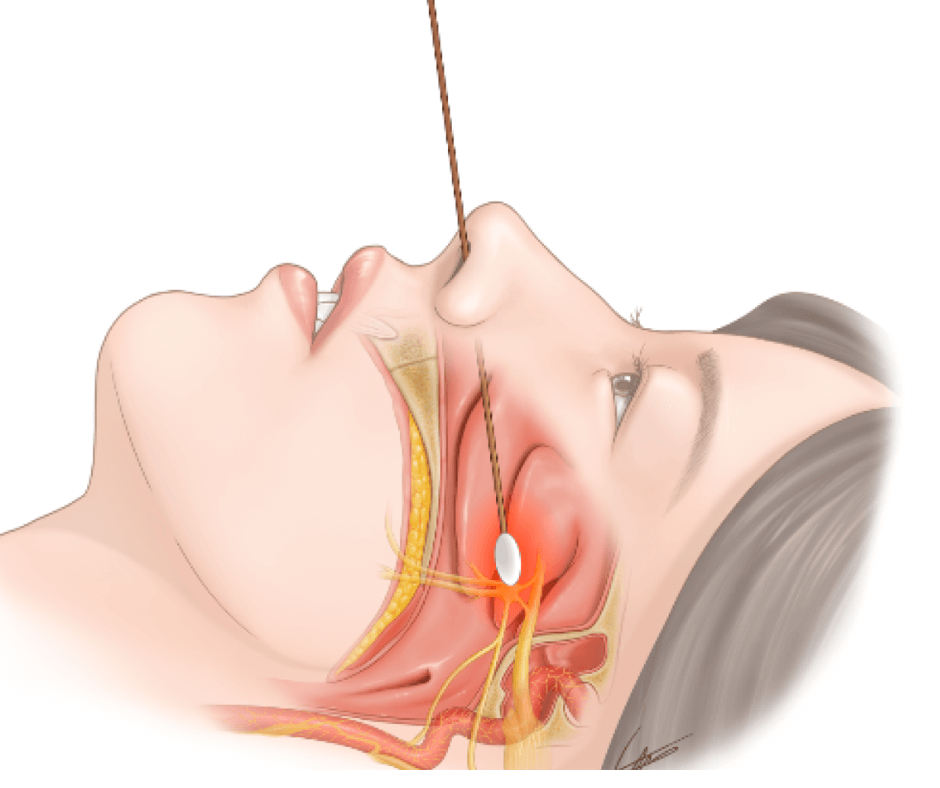



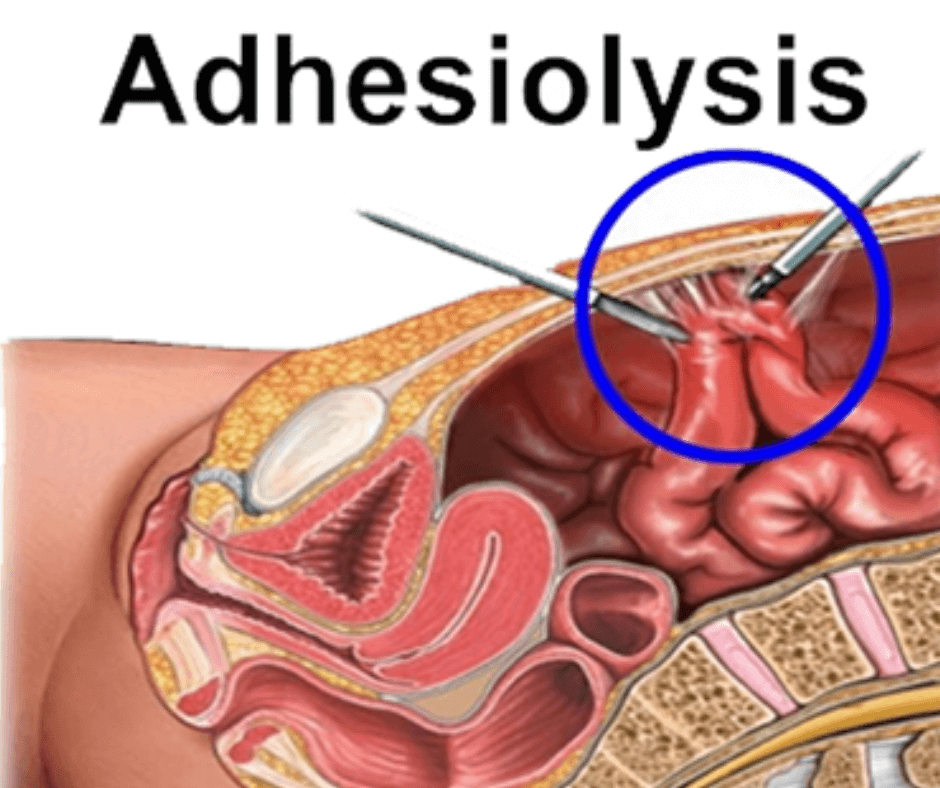




























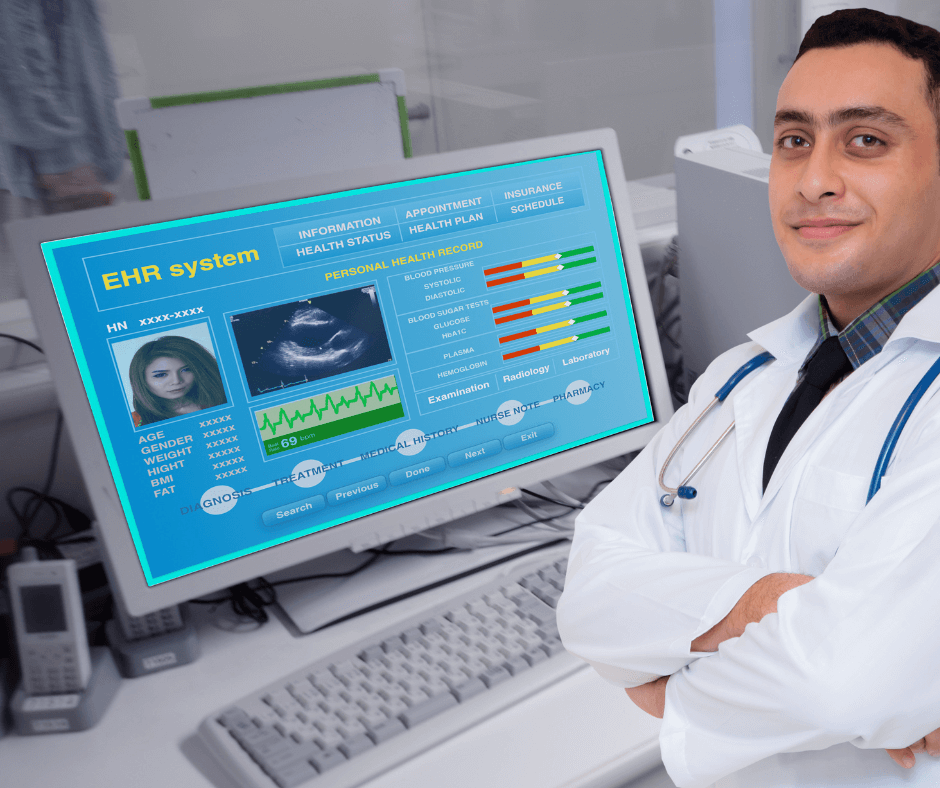






















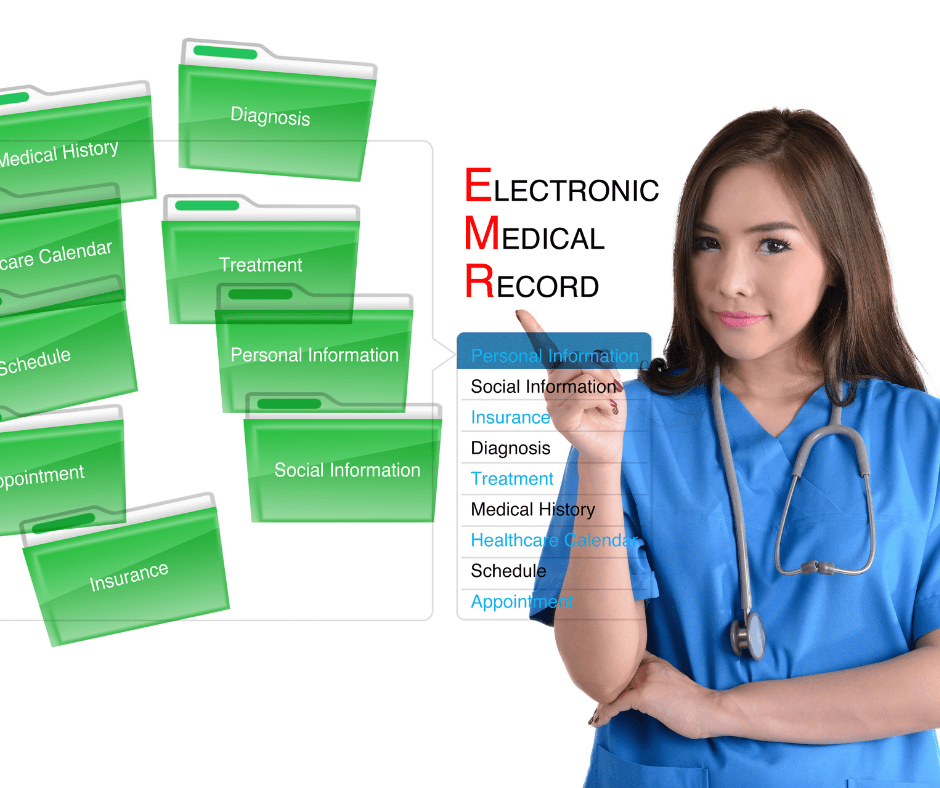
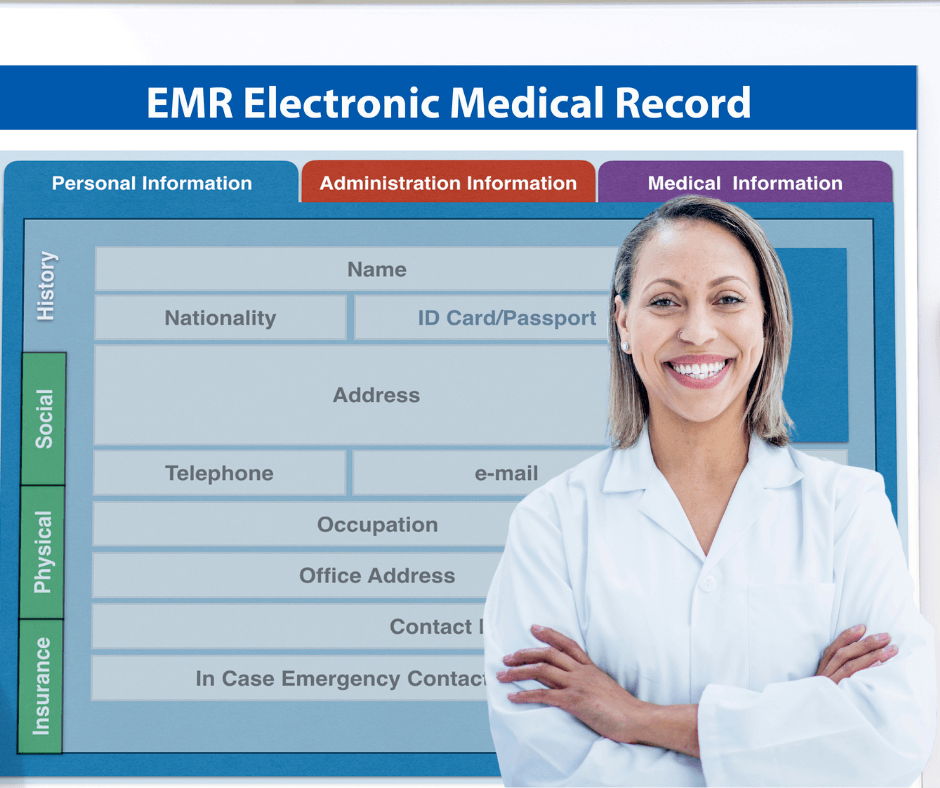



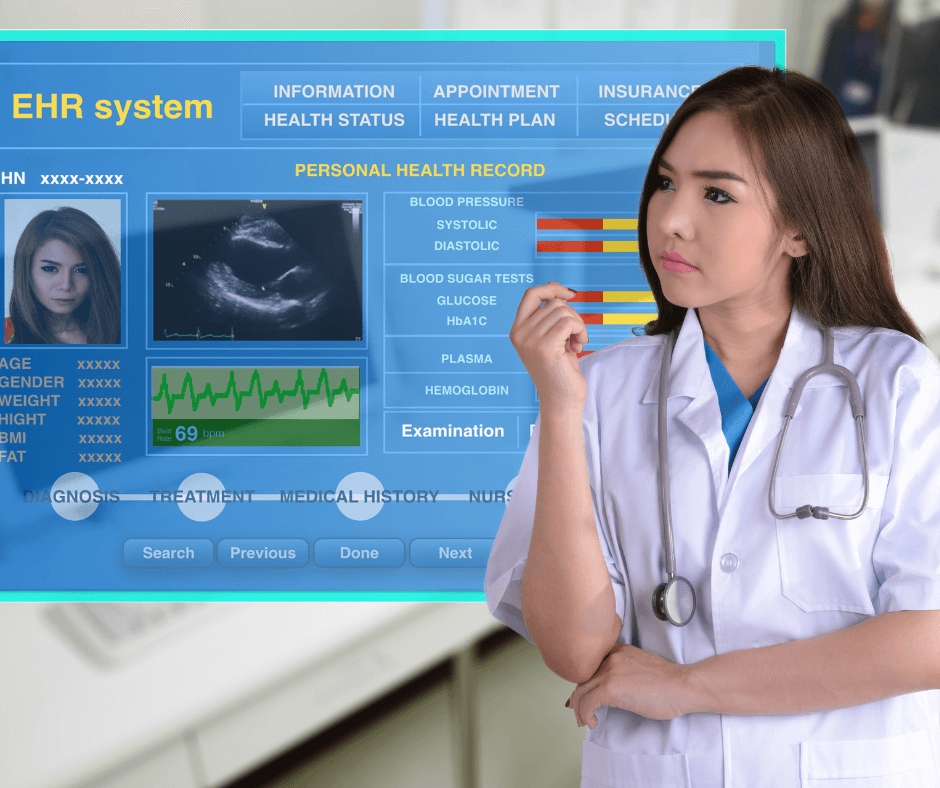

 RSS Feed
RSS Feed