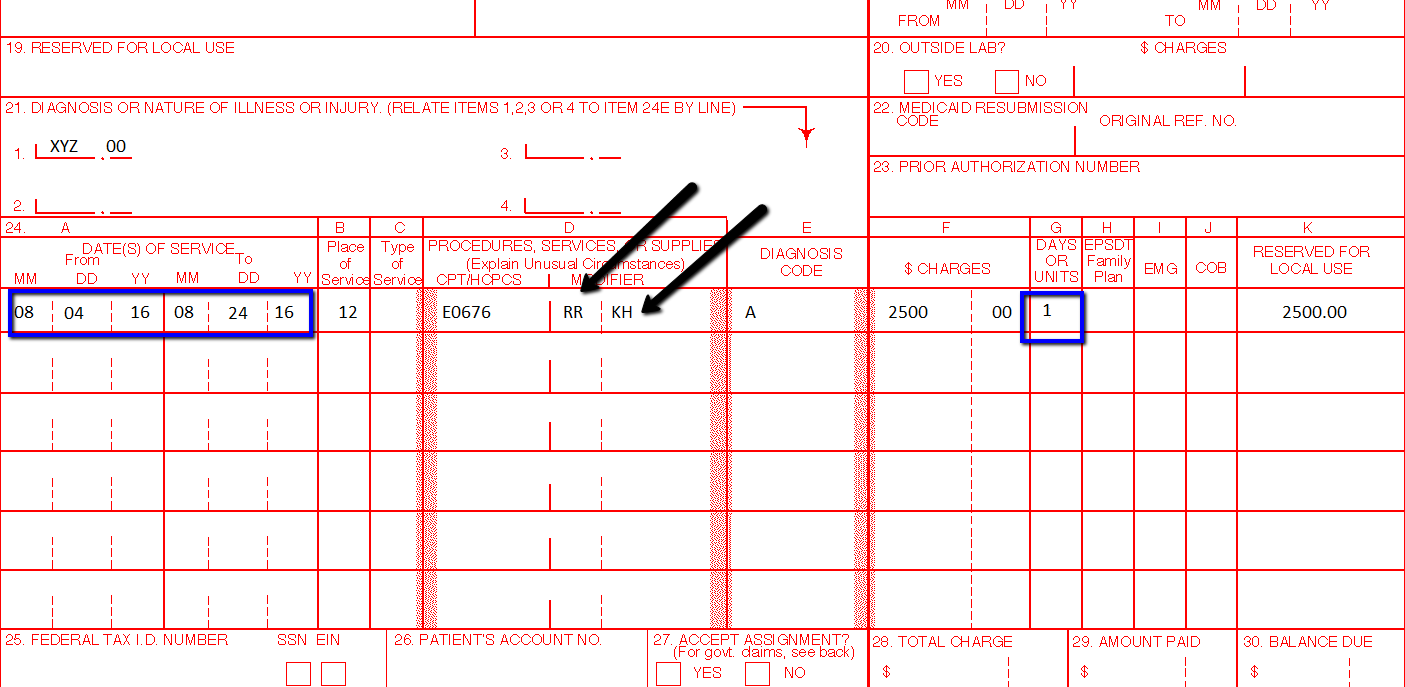
Understanding Billing for DME Services or Durable Medical Equipment Services Many of our blog readers will contact me and ask why is it too complicated to be billing for durable medical equipment? Actually it is not complicated, you just need to understand how it works. Here are some pointers that I would like to point out to you:
Pointers on DME Billing Services and Coding
Other related blog posts:
0 Comments
NEW CPT Code 99072 and CPT Code 86413 DURING COVID19 PANDEMIC These 2 new CPT Codes 99072 and 86413 were published on September 8th 2020 and are effective immediately.  Let's describe these 2 new CPT Codes. CPT Code 99072 Additional supplies, materials, and clinical staff time over and above those usually included in an office visit or other non-facility service(s), when performed during a Public Health Emergency as defined by law, due to respiratory-transmitted infectious disease Take Note: This new code 99072 is reported only during a PHE (Public Health Emergency) and only for additional items required to support a safe in-person provision of evaluation, treatment, or procedural service(s). CPT Code 86413 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Coronavirus disease [COVID-19]) antibody, quantitative According to the AMA: "The first addition, CPT code 99072, was approved in response to sweeping measures adopted by medical practices and health care organizations to stem the spread of the novel coronavirus (SARS-CoV-2), while safely providing patients with access to high-quality care during in-person interactions with health care professionals. The additional supplies and clinical staff time to perform safety protocols described by code 99072 allow for the provision of evaluation, treatment or procedural services during a public health emergency in a setting where extra precautions are taken to ensure the safety of patients as well as health care professionals. The AMA/Specialty Society RVS Update Committee (RUC) worked with 50 national medical specialty societies and other organizations over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency and submitted recommendations today to the Centers for Medicare and Medicaid Services to inform payment of code 99072." "The second addition, CPT code 86413, was approved in response to the development of laboratory tests that provide quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) of SAR-CoV-2 antibodies provided by laboratory tests reported by other CPT codes. By measuring antibodies to SARS-CoV-2, the tests reported by 86413 can investigate a person’s adaptive immune response to the virus and help access the effectiveness of treatments used against the infection." Must be reported only once per in-person! (read more below) Code 99072 is to be reported only once per in-person patient encounter per provider identification number (PIN), regardless of the number of services rendered at that encounter. In the instance in which the noted clinical staff activities are performed by a physician or other qualified health care professional (eg, in practice environments without clinical staff or a shortage of available staff), the activity requirements of this code would be considered as having been met; however, the time spent should not be counted in any other time-based visit or service reported during the same encounter. CPT Guidelines, Q&A from the American Medical Association: Understanding PHE or Public Health Emergency in coordination with CPT Code 99072 Question: Code 99072 is stated as being applicable “during a PHE.” What information should be used to verify when a PHE is in effect? Answer: A PHE is in effect when declared by law by the officially designated relevant public health authority(ies). Understanding Patient Encounters Type for the determination of CPT Code 99072 Question: For what type of patient encounters or services should code 99072 be reported? Answer: Code 99072 may be reported with an in-person patient encounter for an office visit or other non-facility service, in which the implemented guidelines related to mitigating the transmission of the respiratory disease for which the PHE was declared are required. Use of this code is not dependent on a specific patient diagnosis. For a list of POS codes with facility/non-facility designations that are available in the Medicare Claims Processing Manual, visit https://www.cms.gov/Medicare/Coding/place-of-service-codes. Understanding Documentation Requirements when reporting CPT Code 99072 Question: What documentation is required to report code 99072? Answer: Given that code 99072 may only be reported during a PHE, one would not report this code in conjunction with an evaluation and management (E/M) service or procedure when a PHE is not in effect. Therefore, code 99072 is reported justifiably only when health and safety conditions applicable to a PHE require the type of supplies and additional clinical staff time explained in the code descriptor. Documentation requirements may vary among third-party payers and insurers; therefore, they should be contacted to determine their specifications. How about CPT Code 99072 with CPT Code 99070? Question: May code 99072 be reported with code 99070? Answer: Yes, code 99072 may be reported with code 99070 when the requirements for both codes have been met. Note that eligibility for payment, as well as coverage policy, is determined by each individual insurer or third-party payer. Reader's QUESTION - how much are you going to be reimbursed for these 2 new codes?  Reference sources: https://www.ama-assn.org/press-center/press-releases/ama-announces-new-cpt-codes-covid-19-advancements-expand https://www.ama-assn.org/system/files/2020-09/cpt-assistant-guide-coronavirus-september-2020.pdf CPT Assistant September 2020 Special Addition CPT is a trademark and owned by the American Medical Association. One of our blog readers asked why their claim for Trigger Point injection is being denied due to missing modifier. Let's describe these 2 Trigger point injection codes: 20552 Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s) 20553 Injection(s); single or multiple trigger point(s), 3 or more muscles Widely indicated for Myofascial Pain. Key point to remember! - these 2 CPT Codes 20552, 20553 DO NOT NEED A MODIFIER! Denial Reasons for Trigger Point Injection CPT 20553Denials Reasons for Trigger Point Injection CPT 20552, 20553 and what you should be looking for:
Need more help? Call us at 732-982-4800 today!Understanding Shingrix Zoster Vaccine CPT Code 90750Key points to remember in properly billing and coding for Shingrix: Keypoints to remember!
CPT Code Shingrix 90750 What's the reimbursement? CPT Code Shingrix 90750 - What's the reimbursement? I called the manufacturing company of Shingrix at GSK or Global Smith Klein and contacted their Provider Reimbursement support at Phone: 1-855-636-8291. Unfortunately they told me they don't have a national average rate on how much you can get reimbursed per unit for the Shingrix shot. Understandably because it is based on Payer's reimbursement policy. I did some research some more research and found this: From Medicaid North Carolina: ICD-10-CM diagnosis code required for billing is Z23 - Encounter for immunization. Providers must bill with CPT code: 90750 - Zoster (shingles) vaccine, (HZV), recombinant, sub-unit, adjuvanted, for intramuscular injection. One Medicaid unit of coverage is 0.5 mL. The maximum reimbursement rate per unit is $144.20. Providers must bill 11-digit National Drug Codes (NDCs) and appropriate NDC units. The NDCs are 58160-0823-11 and 58160-0819-12. The NDC units should be reported as “UN1.” You can read the complete post here - https://medicaid.ncdhhs.gov/blog/2018/02/07/billing-guidelines-zoster-vaccine-recombinant-adjuvanted-suspension-intramuscular Conclusion: It is always best that your verify your patient's benefits and eligibility for the Shingrix - Zoster Vaccine. As with Medicare, they should be under the beneficiary's Part D benefits. I hope this post helps. |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985










 RSS Feed
RSS Feed