Medicare's Telehealth and Telemedicine Services during Covid-19. Understanding Provider and Non-Provider Services. Understanding “EXPANSION OF TELEHEALTH WITH 1135 WAIVER” So, under this Waiver, Medicare can pay for office, hospital, and other visits furnished via telehealth across the country and including in patient’s places of residence starting March 6, 2020 (date of service). Due to the Coronavirus (COVID-19) Public Health Emergency, doctors and other health care providers can use telehealth services to treat COVID-19 (and for other medically reasonable purposes) from offices, hospitals, and places of residence (like homes, nursing homes, and assisted living facilities) as of March 6, 2020. Medicare will pay for these services for patients who have seen the health care provider or another health care provider in the same practice. These visits are considered as in-person visits and are paid at the rate as regular, in person visits. Starting services rendered on March 6, 2020 and for the duration of the Covid-19 Public Health Emergency, Medicare will make payment for Telehealth Medicine Professional services rendered to Medicare beneficiaries in:
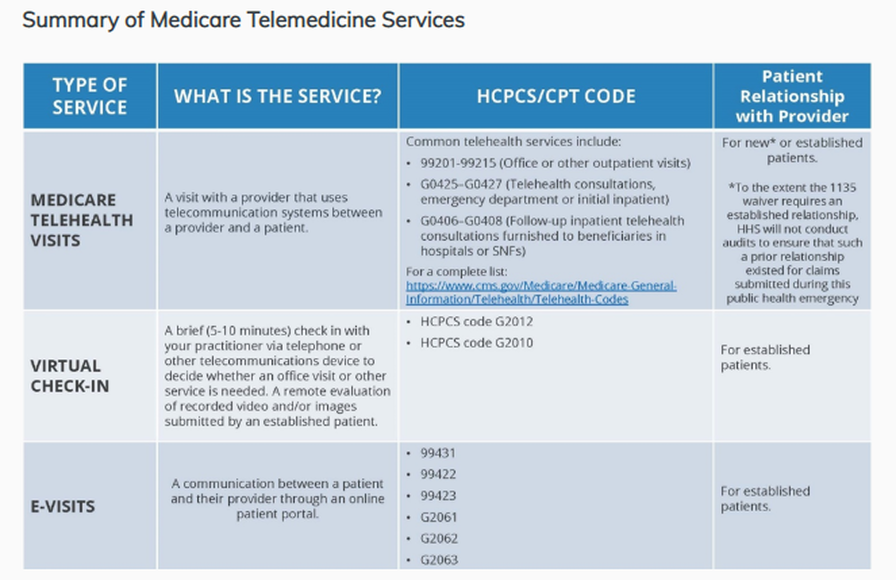
Deductible and Coinsurance will normally apply to these services. But the HHS Office of the Inspector General or the OIG is providing flexibility for healthcare Providers to reduce or waive cost-sharing for telehealth visits paid by the federal healthcare programs. It is imperative during this public health emergency that patients avoid / should not travel, when possible, to physicians’ offices, clinics, hospitals, or other health care facilities where they could risk their own or others’ exposure to further illness. Accordingly, the Department of Health and Human Services (HHS) is announcing a policy of enforcement discretion for Medicare telehealth services furnished pursuant to the waiver under section 1135(b)(8) of the Act. Prior to this Waiver: Medicare could only pay for telehealth on a limited basis: that is; when the person receiving the service is in a designated rural area and when they leave their home and go to a clinic, hospital, or certain other types of medical facilities for the service. Changes in last year (2019), Medicare started reimbursing for brief communications or Virtual Check-Ins, which are short patient-initiated communications with a healthcare practitioner. Medicare Part B separately pays clinicians for E-visits, which are non-face-to-face patient-initiated communications through an online patient portal as well. Effective date of service March 6, 2020: Providers can provide and render Telehealth Medicine including Evaluation and Management visits (E/M common office visits), Mental Health Counseling and Preventive Health Screenings. This will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, are able to visit with their doctor from their home, without having to go to the doctor’s office or hospital which puts themselves and others at risk for Covid-19. Medicare will make payment for professional services furnished to beneficiaries in all areas of the country in all settings. While they must generally travel to or be located in certain types of originating sites such as a physician’s office, skilled nursing facility or hospital for the visit, effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Since the 1135 Waiver requires an established relationship, HHS however will not conduct an audit for all claims submitted during this public health emergency. Question: Will I get Paid? as a Provider? Answer: YES based on MEDICAL NECESSITY! We have 3 types of VIRTUAL SERVICES:
Telehealth Visits: What’s required? The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home. Distant site practitioners and clinicians who can furnish and get reimbursement for covered telehealth services is subject to State Law. REMEMBER! - report using PLACE OF SERVICE is 02 Let’s identify the Providers Billable Services: 3 types of VIRTUAL SERVICES:
Telehealth Visits: What’s required? The provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient at home. Distant site practitioners and clinicians who can furnish and get reimbursement for covered telehealth services (check your State Law as this is subject to State Law) may include the following:
Covered Telehealth Services CY 2020 (Updated 11/01/19) Source: https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes Virtual Check-ins visits may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. Virtual Check-ins visits: Virtual check-ins can be used for the treatment for the Coronavirus (COVID-19) from anywhere, including places of residence (like homes, nursing homes, and assisted living facilities). Virtual check-in services will be initiated by the patient; however, practitioners may need to educate beneficiaries on the availability of the service prior to patient initiation. Must render only to established Medicare patients in their home may have a brief communication service with practitioners via a number of communication technology modalities including synchronous discussion over a telephone or exchange of information through video or image. Services render via:
Here are your billable codes for Virtual Check-ins visits are as follows: HCPCS code G2012 Brief communication technology-based service, e.g. virtual check-in, by a physician or other qualified health care professional who can report evaluation and management services, provided to an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an e/m service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion. Requirements:
*** As being recommended by CMS to use G2012 for telehealth services. More information, click here. HCPCS code G2010 Remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M Evaluation and Management service provided within the previous 7 days nor leading to an e/m service or procedure within the next 24 hours or soonest available appointment. Virtual check-ins can be conducted with a broader range of communication methods, unlike Medicare Telehealth or Telemedicine visits, which require audio and visual capabilities for real-time communication. e-visits services are only rendered via an online patient portal. e-VISITS Services: E-visits services are only rendered via an online patient portal. These services can only be reported when the billing practice has an established relationship with the patient. This is not limited to only rural settings. There are no geographic or location restrictions for these visits. Practitioners who may furnish these services include:
Your Billable Codes for e-visits are as follows: CPT 99421: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes CPT 99422: Online digital evaluation and management service, for an established patient, for up to 7 days cumulative time during the 7 days; 11– 20 minutes CPT 99423: Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes. Clinicians who may not independently bill for evaluation and management visits . For example are:
They can also provide these e-visits and bill using the following codes: HCPCS Code G2061: Qualified non-physician healthcare professional online assessment and management, for an established patient, for up to seven days, cumulative time during the 7 days; 5–10 minutes HCPCS Code G2062: Qualified non-physician healthcare professional online assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 11–20 minutes HCPCS Code G2063: Qualified non-physician qualified healthcare professional assessment and management service, for an established patient, for up to seven days, cumulative time during the 7 days; 21 or more minutes. For more information: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/index.html For Medicare Beneficiaries, you can learn more about telehealth services here - https://www.medicare.gov/coverage/telehealth HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT (HIPAA): Effective immediately, the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency. For more information: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/index.html HEADS-UP! - Use of GT modifier on Medicare claims was eliminated in 2018. According to CMS, the place of service code 02 is sufficient. To read more on Medicare Payment for Telemedicine. - CLICK HERE Medicare Claims Processing Manual Chapter 12 - Physicians/Nonphysician Practitioners 190 - Medicare Payment for Telehealth Services 190.1 - Background 190.2 - Eligibility Criteria 190.3 - List of Medicare Telehealth Services 190.3.1 - Telehealth Consultation Services, Emergency Department or Initial Inpatient versus Inpatient Evaluation and Management (E/M) Visits 190.3.2 - Telehealth Consultation Services, Emergency Department or Initial Inpatient Defined 190.3.3 - Follow-Up Inpatient Telehealth Consultations Defined 190.3.4 – Payment for ESRD-Related Services as a Telehealth Service 190.3.5 – Payment for Subsequent Hospital Care Services and Subsequent Nursing Facility Care Services as Telehealth Services 190.3.6 – Payment for Diabetes Self-Management Training (DSMT) as a Telehealth Service 190.3.7 – Payment for Telehealth for Individuals with Acute Stroke 190.4 - Conditions of Payment 190.5 - Originating Site Facility Fee Payment Methodology 190.6 - Payment Methodology for Physician/Practitioner at the Distant Site 190.6.1 - Submission of Telehealth Claims for Distant Site Practitioners 190.6.2 - Exception for Store and Forward (Non-Interactive) Telehealth 190.7 - A/B MAC (B) Editing of Telehealth Claims Timeline and Important Links: (source: CMS.GOV) For more information on telehealth benefits in the Medicare program, read the fact sheet: https://www.cms.gov/files/document/03052020-medicare-covid-19-fact-sheet.pdf.
Summary of CMS Public Health Action on COVID-19 to date: March 6, 2020, CMS issued frequently asked questions and answers (FAQs) for healthcare providers regarding Medicare payment for laboratory test and other services related to the 2019-Novel Coronavirus (COVID-19). https://www.cms.gov/newsroom/press-releases/covid-19-response-news-alert-cms-issues-frequently-asked-questions-assist-medicare-providers March 5, 2020: CMS issued a second Healthcare Common Procedure Coding System (HCPCS) code for certain COVID-19 laboratory tests, in addition to three fact sheets about coverage and benefits for medical services related to COVID-19 for CMS programs. https://www.cms.gov/newsroom/press-releases/cms-develops-additional-code-coronavirus-lab-tests March 4, 2020: CMS issued a call to action to healthcare providers nationwide and offered important guidance to help State Survey Agencies and Accrediting Organizations prioritize their inspections of healthcare. https://www.cms.gov/newsroom/press-releases/cms-announces-actions-address-spread-coronavirus February 13, 2020: CMS issued a new HCPCS code for providers and laboratories to test patients for COVID-19. https://www.cms.gov/newsroom/press-releases/public-health-news-alert-cms-develops-new-code-coronavirus-lab-test February 6, 2020: CMS gave CLIA-certified laboratories information about how they can test for SARS-CoV-2. https://www.cms.gov/medicareprovider-enrollment-and-certificationsurveycertificationgeninfopolicy-and-memos-states-and/notification-surveyors-authorization-emergency-use-cdc-2019-novel-coronavirus-2019-ncov-real-time-rt February 6, 2020: CMS issued a memo to help the nation’s healthcare facilities take critical steps to prepare for COVID-19. https://www.cms.gov/medicareprovider-enrollment-and-certificationsurveycertificationgeninfopolicy-and-memos-states-and/information-healthcare-facilities-concerning-2019-novel-coronavirus-illness-2019-ncov For the updated information on the range of CMS activities to address COVID-19, visit: https://www.cms.gov/About-CMS/Agency-Information/Emergency/EPRO/Current-Emergencies/Current-Emergencies-page
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
July 2024
Categories
All
BROWSE HERE
All
|
- About
- Leadership
- Contact Us
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985




 RSS Feed
RSS Feed