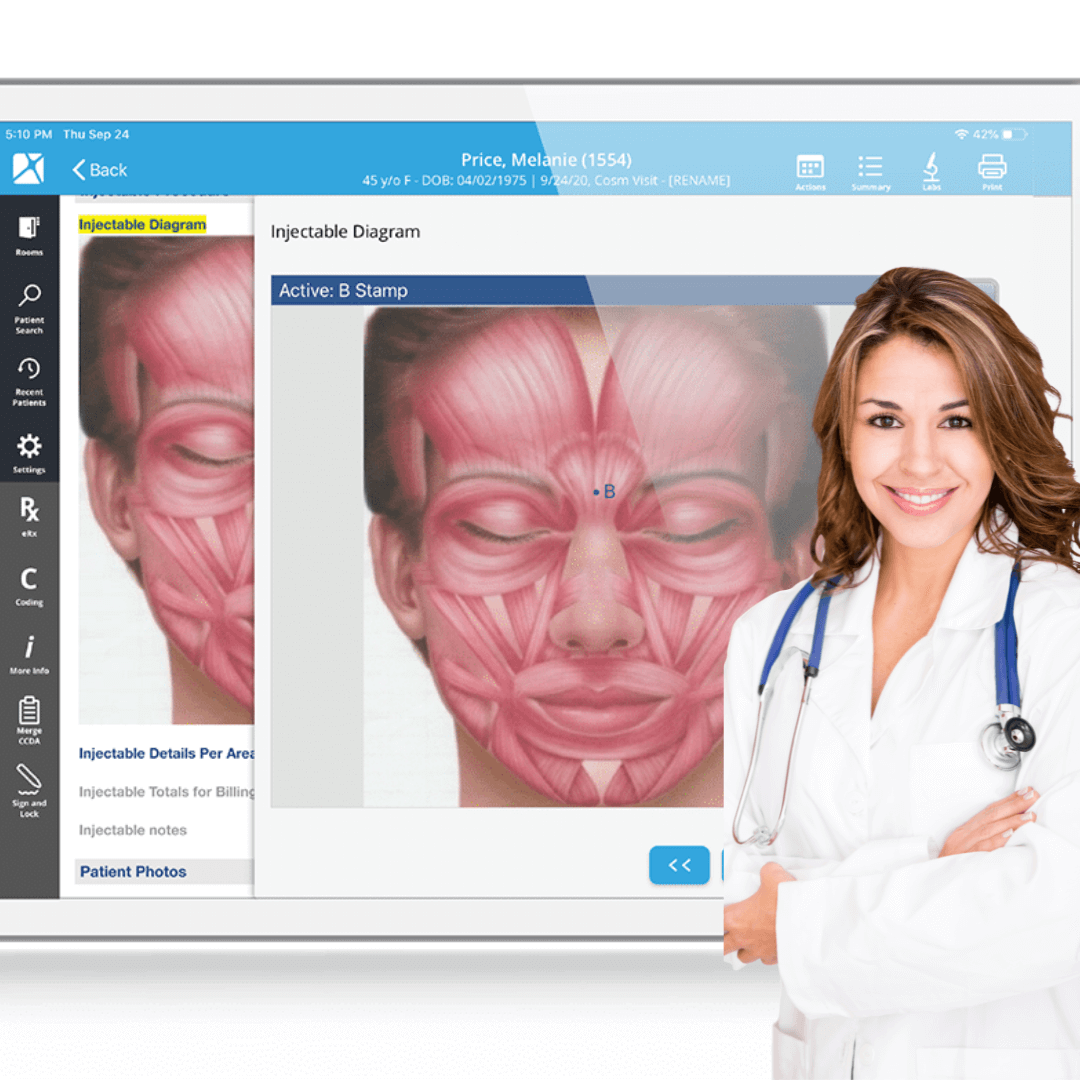
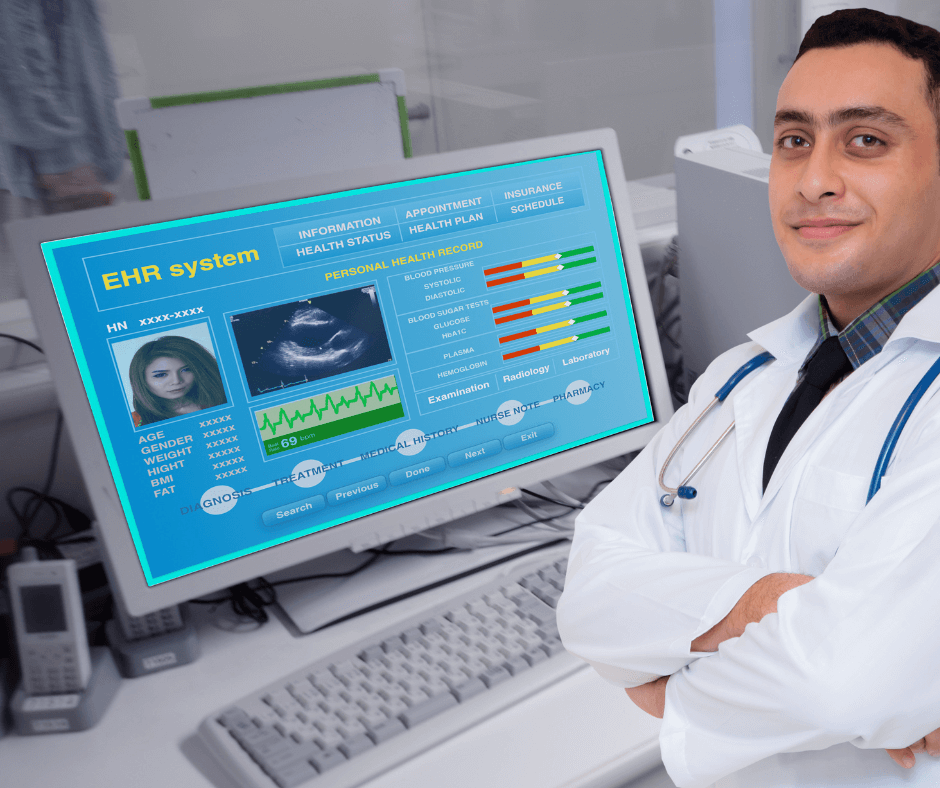
Unlocking the Benefits of Plastic Surgery EHR: A Comprehensive Guide Discover the numerous advantages of incorporating plastic surgery EHR into your practice. Learn how GoHealthcare Practice Solutions for Patients Access Services can help you maximize its potential. Plastic surgery practices around the world are increasingly embracing the power of Electronic Health Records (EHR) to streamline their processes and enhance patient care. With GoHealthcare Practice Solutions for Patients Access Services, we make it easy for you to harness the potential of plastic surgery EHR. In this article, we'll explore the top 12 reasons why adopting plastic surgery EHR is a smart choice for your practice. Improved Patient Care Plastic surgery EHR systems ensure that patient information is easily accessible and up-to-date, allowing for more informed decision-making and better care. Enhanced Communication Plastic surgery EHR systems facilitate seamless communication between healthcare providers, fostering a more collaborative approach to patient care. Increased Efficiency By digitizing patient records, plastic surgery EHR systems eliminate the need for paper files and reduce the time spent on administrative tasks, freeing up more time for patient care. Streamlined Billing and Coding Plastic surgery EHR systems simplify billing and coding processes, reducing errors and ensuring faster reimbursements. Customizable Templates Plastic surgery EHR software often comes with customizable templates tailored to the specific needs of plastic surgery practices, making documentation quicker and more accurate. Easier Compliance Plastic surgery EHR systems help practices stay compliant with regulatory requirements, such as HIPAA and Meaningful Use, by automating the tracking and reporting of necessary data. Enhanced Security The secure storage and encrypted transmission of patient data in plastic surgery EHR systems protect sensitive information from unauthorized access and potential breaches. Remote Access Plastic surgery EHR systems enable providers to access patient records from any location with an internet connection, making it easier to stay up-to-date on patient care. Patient Portal Integration Many plastic surgery EHR solutions offer integrated patient portals, allowing patients to access their records, schedule appointments, and communicate with their providers securely. Advanced Analytics Plastic surgery EHR systems provide advanced analytics that can help practices monitor performance, identify trends, and make data-driven decisions to improve patient outcomes. Scalability As your plastic surgery practice grows, your EHR system can be easily scaled to accommodate more patients, providers, and staff, ensuring a smooth transition. GoHealthcare Practice Solutions for Patients Access Services Our team at GoHealthcare Practice Solutions for Patients Access Services is dedicated to helping you implement and optimize your plastic surgery EHR system. We offer personalized support, training, and ongoing assistance to ensure your practice maximizes the benefits of plastic surgery EHR technology. Investing in a plastic surgery EHR system is a significant step towards enhancing patient care, streamlining processes, and staying competitive in today's healthcare landscape. With GoHealthcare Practice Solutions for Patients Access Services, you can confidently embrace the benefits of plastic surgery EHR and elevate your practice to new heights.
0 Comments
Unlock the Full Potential of Electronic Health Records: 7 Game-Changing Benefits Discover the transformative power of electronic health records in modern healthcare, with insights into their benefits and how they're revolutionizing patient care. As technology continues to revolutionize healthcare, one standout innovation is the adoption of electronic health records (EHRs). These digital versions of traditional paper-based patient records are transforming the way healthcare professionals manage and deliver patient care. Electronic health records have gained traction in recent years, with medical facilities worldwide implementing them to streamline processes and enhance the overall patient experience. In this blog post, we'll explore the game-changing benefits of electronic health records and how they're reshaping the healthcare landscape. Enhanced Patient Care Electronic health records have significantly improved patient care by offering healthcare providers instant access to comprehensive medical histories. EHRs ensure that medical professionals have a clear understanding of a patient's health background, reducing the chances of misdiagnosis or medical errors. This enables physicians to make more informed decisions about treatment plans, ultimately improving the quality of care. Improved Coordination of Care As electronic health records can be shared securely among authorized healthcare providers, they facilitate better communication and coordination of care. EHRs enable seamless collaboration among specialists, primary care physicians, nurses, and other healthcare professionals, ensuring that everyone involved in a patient's care is on the same page. This can lead to more efficient and accurate diagnoses and treatment plans. Increased Patient Engagement Electronic health records have given patients more control over their healthcare, making it easier for them to access their medical information, schedule appointments, and communicate with healthcare providers. This increased engagement empowers patients to make informed decisions about their health and take a more active role in managing their care. Streamlined Workflow and Increased Efficiency The implementation of electronic health records has streamlined various administrative tasks, such as scheduling appointments, managing billing, and updating patient information. This increased efficiency allows healthcare professionals to spend more time on patient care and less on paperwork. Moreover, EHRs reduce the risk of lost or misplaced records, further improving efficiency. Better Data for Public Health Research Electronic health records provide researchers with access to a wealth of accurate and up-to-date health data. This information can be used to analyze trends, identify potential public health risks, and inform policy decisions. The aggregated data from EHRs also enables healthcare providers to identify patterns and make improvements within their own practices. Cost Savings While the initial investment in electronic health records can be substantial, the long-term cost savings are significant. EHRs help to reduce paperwork, minimize the need for storage space, and eliminate the costs associated with locating and transporting paper records. Additionally, the improved efficiency and reduced errors associated with EHRs can lead to decreased malpractice claims and lower insurance premiums. Environmental Benefits By transitioning from paper-based records to electronic health records, healthcare organizations can substantially reduce their environmental impact. EHRs eliminate the need for paper, ink, and physical storage, resulting in a greener and more sustainable healthcare system. The adoption of electronic health records is revolutionizing the healthcare industry, offering numerous benefits for healthcare providers and patients alike. By enhancing patient care, improving coordination, streamlining workflows, and providing valuable data for public health research, EHRs are truly transforming the future of healthcare. Transforming Healthcare: Top 10 Patient Engagement Software Solutions for Modern Organizations4/7/2023 Transforming Healthcare: Top 10 Patient Engagement Software Solutions for Modern Organizations Discover the top 10 patient engagement software solutions that are shaping the future of healthcare organizations, enhancing patient-provider communication, and improving overall care. In today's fast-paced healthcare environment, patient engagement is more crucial than ever. Healthcare organizations must find innovative ways to keep patients informed, involved, and at the center of their care. Patient engagement software for healthcare organizations is making it easier than ever to achieve this goal. This blog post highlights the top 10 patient engagement software solutions that are transforming healthcare organizations and offering unparalleled experiences to both patients and providers. Zocdoc Zocdoc is a leading patient engagement software for healthcare organizations, offering a user-friendly platform for patients to find, book, and manage appointments with medical professionals. Zocdoc simplifies the process of locating in-network providers and streamlines communication between patients and healthcare teams. Phreesia Phreesia is a comprehensive patient engagement software for healthcare organizations, designed to automate various administrative tasks. From appointment scheduling to secure messaging, Phreesia's platform enables providers to focus on delivering exceptional care while improving efficiency. Solutionreach Solutionreach is a cutting-edge patient engagement software solution that empowers healthcare organizations to connect with patients on a deeper level. The platform offers a suite of communication tools, appointment reminders, and patient surveys, enabling providers to enhance the overall patient experience. Luma Health Luma Health is a patient engagement software for healthcare organizations that focuses on simplifying communication and reducing no-shows. The platform offers appointment reminders, two-way messaging, and telehealth solutions to help providers maintain a strong connection with their patients. Welkin Health Welkin Health is a versatile patient engagement software for healthcare organizations that supports care teams in delivering personalized patient experiences. With its flexible care management platform, Welkin Health enables providers to customize workflows and streamline patient communication. Bridge Patient Portal Bridge Patient Portal is a patient engagement software solution that helps healthcare organizations connect with their patients in a secure, user-friendly environment. The platform provides appointment scheduling, prescription refills, and lab results, empowering patients to take control of their healthcare journey. InteliChart InteliChart is a robust patient engagement software for healthcare organizations, offering a comprehensive suite of tools to enhance patient-provider communication. From appointment reminders to secure messaging, InteliChart helps healthcare teams provide better, more personalized care. Updox Updox is a patient engagement software solution designed to streamline communication between healthcare organizations and their patients. Offering features such as video conferencing, appointment reminders, and secure messaging, Updox enables providers to engage with their patients in a more meaningful way. PatientPop PatientPop is a dynamic patient engagement software for healthcare organizations that focuses on attracting, retaining, and delighting patients. With its marketing automation and reputation management tools, PatientPop helps healthcare organizations grow and thrive. Medfusion Medfusion is a patient engagement software solution that simplifies patient-provider communication, enabling healthcare organizations to provide better care. The platform offers appointment scheduling, secure messaging, and patient portal access to make managing healthcare convenient and efficient. These top 10 patient engagement software solutions for healthcare organizations are transforming the way providers and patients connect. By investing in these powerful tools, healthcare organizations can enhance patient-provider communication, improve the overall patient experience, and streamline administrative tasks. Don't miss the opportunity to elevate your healthcare organization with one of these innovative patient engagement software solutions. Enhancing Healthcare Outcomes with Clinical Decision Support Systems for Hospitals Discover the significant benefits of implementing clinical decision support systems for hospitals and how these innovative tools are transforming patient care and medical efficiency. Clinical decision support systems for hospitals are becoming essential tools in the modern healthcare landscape. These advanced technologies offer healthcare professionals vital assistance in making accurate, evidence-based decisions that lead to better patient outcomes. In this article, we will explore the most notable advantages of clinical decision support systems for hospitals and how they are positively impacting the healthcare industry. Improved Diagnostic Accuracy: Clinical decision support systems for hospitals are designed to analyze and integrate patient data to provide medical professionals with evidence-based recommendations. This helps reduce diagnostic errors and improve the overall quality of care. By leveraging these systems, doctors and nurses can make more accurate diagnoses and prescribe the most effective treatment plans. Enhanced Patient Safety: One of the primary benefits of clinical decision support systems for hospitals is their ability to enhance patient safety. By providing healthcare professionals with relevant information and alerts regarding potential drug interactions or allergies, these systems help minimize adverse events and ensure optimal patient care. Streamlined Workflows: Clinical decision support systems for hospitals are invaluable when it comes to streamlining workflows within medical facilities. They enable healthcare providers to access critical patient information quickly and efficiently, which in turn leads to more informed decisions and improved patient outcomes. Cost Savings: Clinical decision support systems for hospitals have been shown to reduce healthcare costs significantly. By facilitating accurate diagnoses and effective treatment plans, these systems minimize the need for unnecessary tests, treatments, or hospitalizations. In the long run, this leads to substantial cost savings for both hospitals and patients. Better Communication and Collaboration: Clinical decision support systems for hospitals foster better communication and collaboration among healthcare professionals. By providing instant access to comprehensive patient data, these systems allow for seamless sharing of information and insights among medical teams, improving coordination and decision-making processes. Continuous Learning and Adaptation: Clinical decision support systems for hospitals are constantly evolving, incorporating the latest medical research and guidelines to ensure that healthcare providers receive the most up-to-date information. This continuous learning and adaptation help hospitals stay ahead in the ever-changing healthcare landscape. Time Savings: Time is a valuable resource in healthcare, and clinical decision support systems for hospitals significantly reduce the time spent searching for patient information or consulting medical resources. This allows healthcare professionals to spend more time with their patients and provide better, more personalized care. Data-Driven Decision Making: Clinical decision support systems for hospitals enable medical professionals to make data-driven decisions. By leveraging artificial intelligence and advanced algorithms, these systems can analyze complex data sets to generate evidence-based recommendations, ultimately leading to improved patient outcomes. Clinical decision support systems for hospitals are transforming the way healthcare professionals make decisions, leading to more accurate diagnoses, better patient safety, and overall improved healthcare outcomes. By implementing these innovative systems, hospitals can enhance their medical efficiency, streamline workflows, and deliver top-notch patient care. As the healthcare industry continues to evolve, clinical decision support systems for hospitals will undoubtedly play a crucial role in shaping the future of medical care. Top 10 Medical Coding Software Solutions Revolutionizing Healthcare in 2023 Discover the top 10 medical coding software solutions that are revolutionizing the healthcare industry in 2023, simplifying billing and streamlining operations. In today's fast-paced healthcare industry, medical coding software has become an essential tool for medical professionals, administrators, and billing specialists alike. These software solutions streamline the coding process, ensuring accurate billing, reducing errors, and increasing overall efficiency. In this blog post, we'll explore the top 10 medical coding software solutions that are revolutionizing healthcare in 2023. 3M Codefinder One of the industry's leading medical coding software solutions, 3M Codefinder, offers comprehensive and accurate coding for ICD-10, CPT, and HCPCS codes. This powerful software improves efficiency, minimizes errors, and helps medical professionals stay up-to-date with the latest coding guidelines. Optum360 EncoderPro Optum360 EncoderPro is a cloud-based medical coding software that provides a user-friendly interface for healthcare professionals. It simplifies the coding process, offers real-time updates, and integrates seamlessly with electronic health record (EHR) systems, making it an excellent choice for any medical practice. AAPC Coder Designed by the American Academy of Professional Coders, AAPC Coder is a reliable medical coding software that boasts an extensive code library and various helpful features. This software is perfect for medical coders and billers who want to enhance their coding accuracy and productivity. Kareo Billing Kareo Billing is a popular medical coding software that simplifies the billing process for small to medium-sized practices. It offers customizable billing workflows and features like automated claim tracking, making it an essential tool for streamlining your practice's operations. TruCode Encoder TruCode Encoder is a versatile medical coding software that ensures quick and accurate coding for inpatient and outpatient services. This software integrates with EHR systems and provides real-time access to coding resources, making it a valuable addition to any healthcare facility. Find-A-Code Find-A-Code is a comprehensive medical coding software solution that offers a user-friendly interface and an extensive library of codes. With features like customizable code lists and an ICD-10 code conversion tool, this software is perfect for busy healthcare professionals. Medicode Medicode is a powerful medical coding software designed to increase productivity and reduce coding errors. Its extensive code library and advanced search features make it an excellent choice for healthcare facilities that require accurate and efficient coding. Nuance Clintegrity Nuance Clintegrity is a cutting-edge medical coding software that combines AI-driven technology with an extensive code library. This software streamlines the coding process and ensures that medical professionals can code accurately and efficiently. Flash Code Flash Code is a user-friendly medical coding software solution that offers rapid access to coding information. With an extensive library of ICD-10, CPT, and HCPCS codes, this software is perfect for healthcare professionals seeking an easy-to-use coding tool. CodoniX E&M Coder CodoniX E&M Coder is a medical coding software that simplifies the evaluation and management coding process. This software is designed to help healthcare professionals accurately code patient encounters, reducing the risk of billing errors and improving overall efficiency. Medical coding software solutions play a crucial role in the modern healthcare industry. With the top 10 medical coding software solutions outlined above, healthcare professionals can streamline their coding processes, ensuring accurate billing, and improving overall efficiency. Don't hesitate to explore these powerful tools and find the perfect fit for your practice. How to Avoid the Top 10 Common Medical Billing Errors Medical billing is a complex and crucial process in healthcare. It involves submitting and processing claims for healthcare services provided to patients. However, medical billing errors are not uncommon and can have a significant impact on healthcare providers' revenue cycle. In this article, we will discuss ten common medical billing errors and provide tips on how to avoid them. Incorrect Patient Information: One of the most common medical billing errors is submitting claims with incorrect patient information. This can include misspelled names, incorrect birthdates, or invalid insurance policy numbers. To avoid this error, ensure that all patient information is verified and updated regularly. Upcoding: Upcoding is the practice of billing for a higher level of service than what was actually provided. This is considered fraudulent and can result in serious consequences. To avoid upcoding, ensure that all billing codes accurately reflect the services provided. Duplicate Billing: Duplicate billing occurs when the same service is billed twice. This can happen if there is a system error or if the provider submits the same claim to multiple insurance companies. To avoid duplicate billing, ensure that all claims are submitted correctly the first time. Lack of Documentation: Insufficient documentation can lead to denied claims or delayed reimbursement. To avoid this error, ensure that all documentation accurately reflects the services provided and is submitted with the claim. Incorrect Coding: Incorrect coding can lead to denied claims or delayed reimbursement. To avoid this error, ensure that all billing codes accurately reflect the services provided. Failure to Follow Up on Denied Claims: Failing to follow up on denied claims can lead to lost revenue. To avoid this error, establish a process for tracking and following up on denied claims. Failure to Bill for All Services Provided: Failure to bill for all services provided can result in lost revenue. To avoid this error, ensure that all services provided are accurately documented and billed. Lack of Staff Training: Lack of staff training can lead to errors in medical billing. To avoid this error, provide training to all staff members involved in the billing process. Medical billing errors can have a significant impact on a healthcare provider's revenue cycle. By avoiding these ten common errors, healthcare providers can ensure that claims are processed accurately and in a timely manner, leading to a more efficient and profitable practice. Remember to always verify patient information, accurately code services provided, and provide staff training to avoid medical billing errors. How Medical Billing Software Can Help You Optimize Your Revenue Cycle Management Revenue cycle management (RCM) is a critical aspect of any healthcare practice. It involves managing the financial process of patient care, from appointment scheduling to payment collection. Optimizing RCM can help healthcare providers improve financial performance and provide better patient care. Medical billing software can be a valuable tool in optimizing RCM. In this article, we will discuss how medical billing software can help you optimize your revenue cycle management. Streamlined Billing Process: Medical billing software can help healthcare providers streamline their billing process by automating many of the tasks involved, such as claim submissions, payment posting, and patient billing. This can help to reduce errors and improve efficiency, which can have a significant impact on the bottom line. Improved Accuracy: Medical billing software can help to improve accuracy in the billing process by reducing the risk of coding mistakes, claim denials, and incorrect billing. This can help to ensure accurate and timely reimbursement, which is critical for the financial health of healthcare practices. Enhanced Revenue: Medical billing software can help healthcare providers enhance their revenue by reducing the number of claim denials, improving collections, and optimizing reimbursement rates. This can have a significant impact on the financial performance of healthcare practices. Better Patient Experience: Medical billing software can also improve the patient experience by providing easy-to-understand billing statements and offering online payment options. This can help to reduce patient frustration and improve patient satisfaction, which is important for patient retention and practice growth. Medical billing software can be a valuable tool in optimizing revenue cycle management for healthcare providers. By streamlining the billing process, improving accuracy, enhancing revenue, and improving the patient experience, medical billing software can help healthcare providers improve financial performance and provide better patient care. Healthcare providers should consider investing in medical billing software to optimize their revenue cycle management and improve their financial performance. CPT Codes for Regenerative Medicine in Pain Management Regenerative medicine offers promising solutions for pain management. However, billing and coding for regenerative medicine procedures can be challenging. Understanding the appropriate Current Procedural Terminology (CPT) codes is critical for accurate billing and reimbursement. In this article, we will discuss CPT codes for regenerative medicine in pain management. 20552 - Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s) CPT code 20552 is used for injection of a single or multiple trigger point(s) in one or two muscles. This code is commonly used in pain management procedures that involve trigger point injections. 20553 - Injection(s); single or multiple trigger point(s), 3 or more muscles CPT code 20553 is used for injection of a single or multiple trigger point(s) in three or more muscles. This code is commonly used in pain management procedures that involve trigger point injections. 20926 - Tissue grafts, other (e.g., paratenon, fat, dermis) CPT code 20926 is used for the placement of tissue grafts, such as paratenon, fat, or dermis. This code may be used in regenerative medicine procedures, such as platelet-rich plasma injections. 20930 - Tissue grafts, other (e.g., paratenon, fat, dermis); cellular implantation, each additional site CPT code 20930 is used for the cellular implantation of tissue grafts in each additional site. This code may be used in regenerative medicine procedures, such as stem cell therapy. 0232T - Percutaneous implantation of biologic implant (e.g., stem cell) into the intervertebral disc space, lumbar CPT code 0232T is used for percutaneous implantation of biologic implants, such as stem cells, into the intervertebral disc space in the lumbar region. This code may be used in regenerative medicine procedures for low back pain. 0234T - Percutaneous implantation of biologic implant (e.g., stem cell) into the intervertebral disc space, cervical CPT code 0234T is used for percutaneous implantation of biologic implants, such as stem cells, into the intervertebral disc space in the cervical region. This code may be used in regenerative medicine procedures for neck pain. 64450 - Injection(s), anesthetic agent and/or steroid, plantar common digital nerve(s) (e.g., Morton's neuroma) CPT code 64450 is used for injection of anesthetic agents and/or steroids into the plantar common digital nerve(s). This code may be used in regenerative medicine procedures for Morton's neuroma. 64640 - Destruction by neurolytic agent, plantar common digital nerve(s) (e.g., Morton's neuroma) CPT code 64640 is used for destruction of the plantar common digital nerve(s) using a neurolytic agent. This code may be used in regenerative medicine procedures for Morton's neuroma. Accurate billing and coding for regenerative medicine procedures in pain management is critical for proper reimbursement. By understanding these CPT codes for pain management procedures, healthcare providers can ensure accurate billing and reimbursement for their services. Remember to use CPT codes 20552 and 20553 for trigger point injections, US Healthcare Consulting Services Market: A Comprehensive Guide for the Modern Healthcare Professional The US Healthcare Consulting Services Market has experienced significant growth in recent years, thanks to the ever-evolving landscape of healthcare in the United States. With ongoing changes in regulations, technology, and patient needs, healthcare organizations are increasingly turning to consultants to navigate these complexities. This blog post will provide an informative guide to the US Healthcare Consulting Services Market for surgeons, physicians, medical billers, IT healthcare professionals, and other stakeholders in the healthcare industry. Understanding the US Healthcare Consulting Services Market: The US Healthcare Consulting Services Market is a dynamic ecosystem of service providers that cater to various aspects of healthcare, such as regulatory compliance, financial management, operations, and technology. These consultants work with healthcare organizations to improve efficiency, increase revenue, and achieve better patient outcomes. Key Drivers of Growth in the US Healthcare Consulting Services Market: The US Healthcare Consulting Services Market has grown due to several factors, including:
Types of Services Offered in the US Healthcare Consulting Services Market: The US Healthcare Consulting Services Market offers a wide range of services, catering to various needs of healthcare organizations. These services include:
Top Players in the US Healthcare Consulting Services Market: Several established firms and emerging companies are making a mark in the US Healthcare Consulting Services Market. Some of the top players include:
Challenges and Opportunities in the US Healthcare Consulting Services Market: As the US Healthcare Consulting Services Market continues to grow, there are both challenges and opportunities that consultants and healthcare organizations must address. These include:
How to Choose the Right Healthcare Consultant: Selecting the right consultant in the US Healthcare Consulting Services Market can be a critical decision for healthcare organizations. Factors to consider when choosing a consultant include:
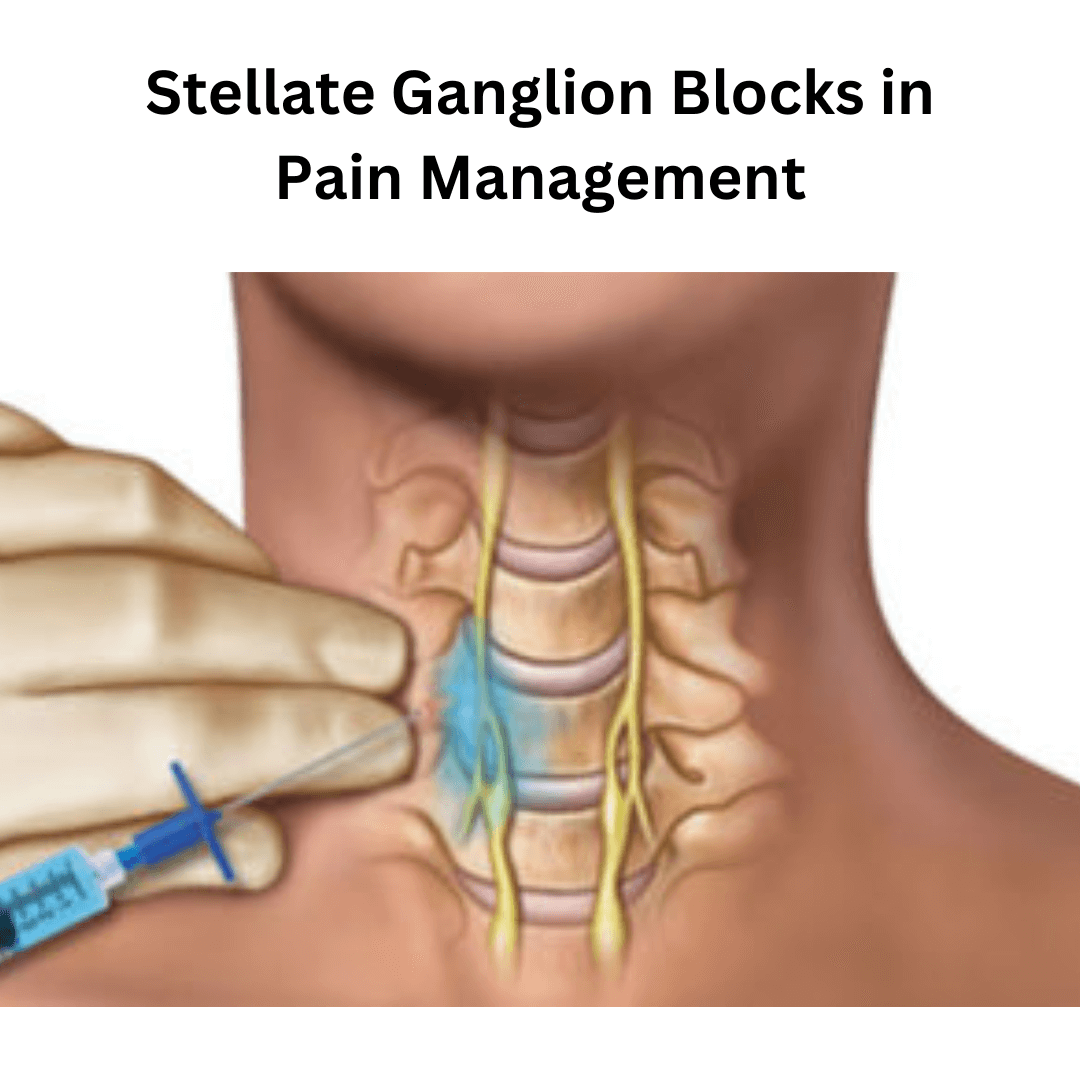
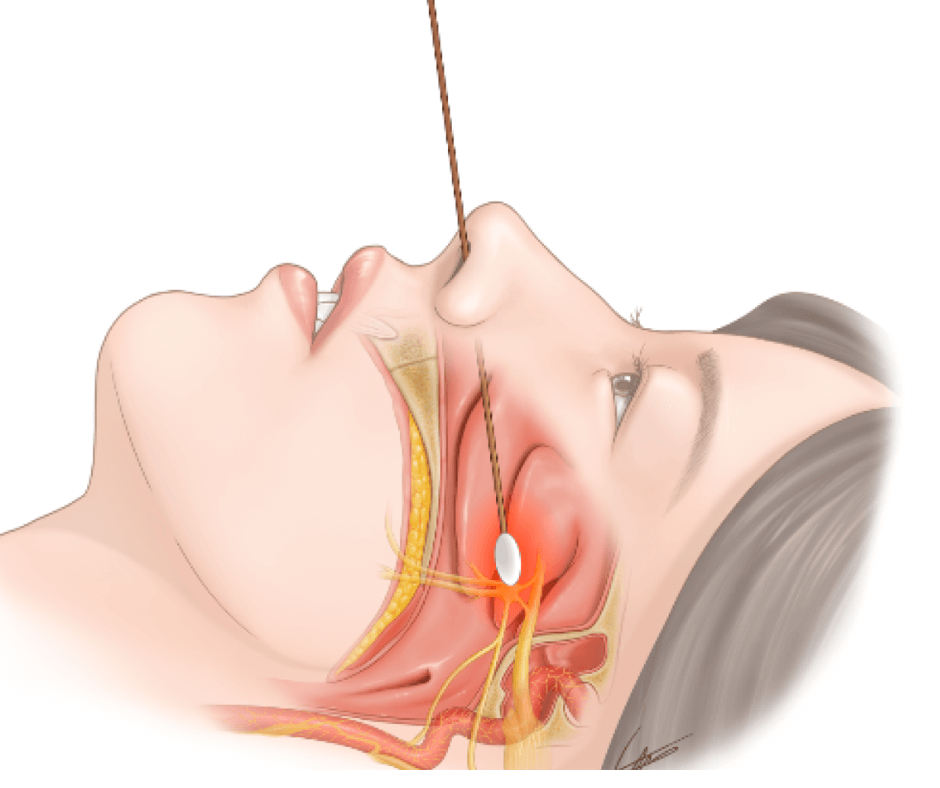
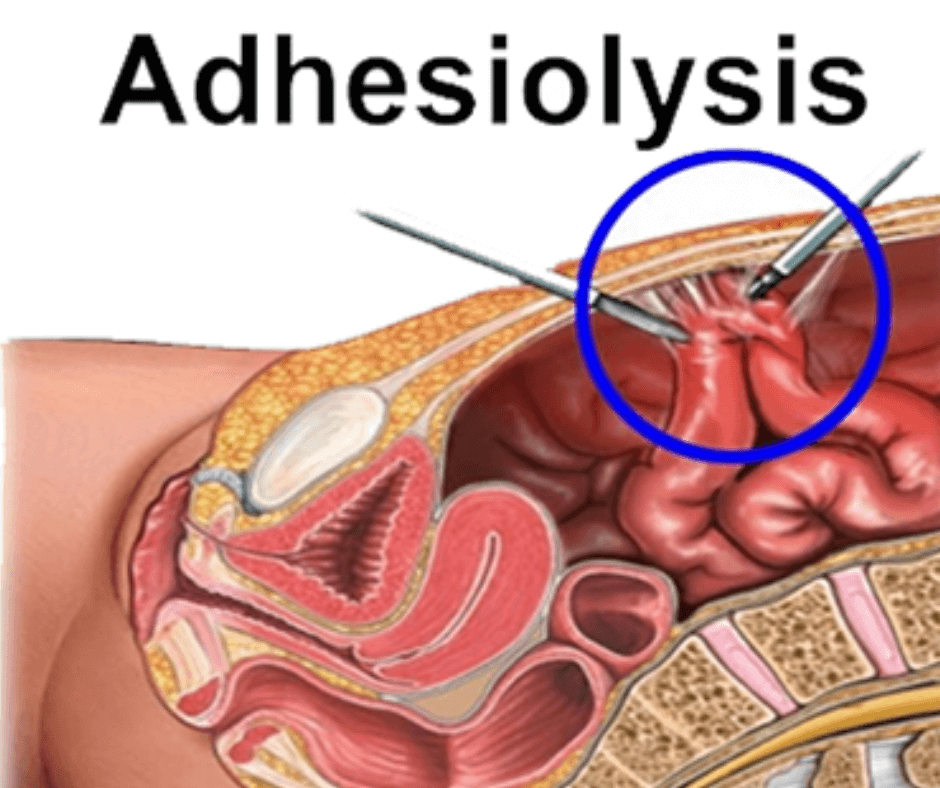
The US Healthcare Consulting Services Market offers healthcare organizations a wealth of resources to improve their operations, finances, and patient care. By understanding the market's key drivers, services offered, top players, challenges, and opportunities, healthcare professionals can make informed decisions about engaging the right consultants to help them achieve their goals. With the continued evolution of healthcare in the United States, the US Healthcare Consulting Services Market will likely remain an essential partner for organizations navigating this complex landscape. CPT Codes for Stellate Ganglion Blocks in Pain Management Stellate ganglion blocks (SGB) are a common procedure used in pain management to alleviate pain in the head, neck, and upper extremities. Accurate coding of SGB procedures is critical for proper reimbursement and revenue cycle management. In this article, we will discuss the CPT codes used for SGB procedures in pain management. CPT Codes for SGB: The CPT codes used for SGB procedures in pain management are: 64415: Injection, anesthetic agent; brachial plexus, single 64416: Injection, anesthetic agent; brachial plexus, continuous infusion by catheter (including catheter placement) 64417: Injection, anesthetic agent; cervical plexus (e.g., stellate ganglion), single 64418: Injection, anesthetic agent; cervical plexus (e.g., stellate ganglion), continuous infusion by catheter (including catheter placement) These codes should be used based on the specific SGB procedure performed, as well as any additional procedures performed during the same session. Code 64415 is used for a single injection of an anesthetic agent into the brachial plexus. Code 64416 is used for a continuous infusion of an anesthetic agent via a catheter placed into the brachial plexus. Code 64417 is used for a single injection of an anesthetic agent into the cervical plexus, specifically the stellate ganglion. Code 64418 is used for a continuous infusion of an anesthetic agent via a catheter placed into the cervical plexus, specifically the stellate ganglion. Accurate coding of SGB procedures in pain management is critical for proper reimbursement and revenue cycle management. The CPT codes used for SGB procedures include 64415, 64416, 64417, and 64418. Healthcare providers should ensure that they use the appropriate code based on the specific procedure performed and any additional procedures performed during the same session. With accurate coding, healthcare providers can optimize their revenue cycle management and provide quality patient care. Boosting Patient-Provider Connections: Top 5 Patient Engagement Software Solutions Explore the top 5 patient engagement software solutions that streamline communication, enhance patient satisfaction, and improve overall healthcare experiences. As the healthcare industry continues to embrace digital transformation, patient engagement software has become increasingly essential for maintaining strong connections between patients and providers. At GoHealthcare Practice Solutions for Patients Access Services, we understand the importance of empowering patients to take control of their healthcare journey. In this blog post, we will highlight the top 5 patient engagement software solutions that are changing the game in patient-provider communication. GoHealthcare Practice Solutions for Patients Access Services Our very own patient engagement software is designed to optimize and simplify the patient experience. Our easy-to-use platform offers appointment scheduling, secure messaging, and personalized education materials, all aimed at increasing patient engagement. By focusing on a user-friendly interface and seamless integration with electronic health records (EHR), we provide healthcare professionals and patients alike with an efficient and effective tool for better communication and improved patient outcomes. Luma Health Luma Health's patient engagement software is a comprehensive solution that streamlines patient communication and helps providers deliver a better healthcare experience. From appointment reminders to telehealth capabilities, this platform offers a wide range of features to keep patients engaged and informed. By automating many time-consuming tasks, Luma Health frees up valuable time for healthcare providers to focus on their patients, ultimately boosting patient satisfaction. Phreesia Phreesia's patient engagement software is known for its exceptional customization options. This versatile platform allows healthcare providers to tailor patient communication and education materials to suit the unique needs of their practice. With features like pre-appointment check-ins, secure messaging, and personalized care plans, Phreesia is a powerful tool for engaging patients and ensuring they have access to the resources they need to manage their health effectively. Medfusion Medfusion's patient engagement software is designed to improve patient access to care through an integrated suite of digital tools. With a focus on patient portal functionality, this platform enables patients to schedule appointments, view test results, and securely message their healthcare providers with ease. Medfusion's commitment to simplifying patient-provider communication makes it a popular choice for healthcare organizations looking to enhance their patient engagement efforts. Solutionreach Solutionreach's patient engagement software is centered on helping healthcare practices foster strong relationships with their patients. Through targeted patient communication, automated reminders, and digital reputation management, this platform helps providers stay connected with patients and encourage ongoing engagement. Solutionreach's focus on relationship-building sets it apart as a valuable tool for healthcare organizations looking to prioritize patient satisfaction and long-term patient loyalty. Patient engagement software is an invaluable tool for healthcare providers seeking to strengthen connections with their patients and improve overall satisfaction. As a leader in patient access services, GoHealthcare Practice Solutions for Patients Access Services is committed to offering the most effective and innovative solutions in the field. By implementing a robust patient engagement software, healthcare organizations can streamline communication, empower patients to take control of their healthcare journey, and ultimately deliver a more positive experience for all involved. CPT Codes for Sphenopalatine Ganglion Blocks in Pain Management Sphenopalatine ganglion blocks are an effective pain management intervention for patients with chronic head and facial pain. However, healthcare providers and insurance companies must understand the appropriate CPT codes for pain management procedures to ensure accurate billing and insurance coverage. In this article, we will provide a comprehensive guide to CPT codes for sphenopalatine ganglion blocks in pain management, including the most commonly used codes and their significance. What are Sphenopalatine Ganglion Blocks? Sphenopalatine ganglion blocks involve injecting a local anesthetic into the sphenopalatine ganglion, a collection of nerve cells located in the back of the nose. The procedure is performed to block pain signals transmitted by the trigeminal nerve, which can cause chronic head and facial pain. Sphenopalatine ganglion blocks are a minimally invasive procedure and can be performed in an outpatient setting. Why are CPT Codes for Pain Management Procedures Important? CPT codes for pain management procedures are essential because they determine how healthcare providers are reimbursed for their services. Each CPT code represents a specific procedure or service and has a corresponding fee schedule that providers use to determine the cost of the service. Healthcare providers must use the appropriate CPT codes for pain management procedures to ensure accurate billing and insurance coverage. Most Common CPT Codes for Sphenopalatine Ganglion Blocks in Pain Management There are several CPT codes used for sphenopalatine ganglion blocks in pain management, depending on the specific procedure performed and the number of levels treated. The most commonly used CPT codes for sphenopalatine ganglion blocks include: 64405 - Injection, anesthetic agent and/or steroid, sphenopalatine ganglion. 64999 - Unlisted procedure, nervous system. It is essential to consult with your healthcare provider and insurance carrier to determine the appropriate CPT code for your specific procedure, as the codes may vary depending on the specific procedure performed and the insurance carrier. CPT codes for sphenopalatine ganglion blocks in pain management are essential to ensure accurate medical billing and insurance coverage. The most commonly used CPT codes for sphenopalatine ganglion blocks include 64405 and 64999. Healthcare providers and insurance companies must be familiar with these codes to ensure that patients receive the care they need without financial burden. If you're experiencing chronic head or facial pain, talk to your healthcare provider to see if sphenopalatine ganglion blocks are a viable treatment option. And for healthcare providers, make sure that you use the proper CPT codes for pain management procedures to ensure proper billing and reimbursement. By following the proper guidelines for medical billing, we can ensure that patients receive the care they need while minimizing financial hardship. CPT Codes for Percutaneous Adhesiolysis in Pain Management: A Comprehensive Guide Pain management is a crucial aspect of healthcare, and percutaneous adhesiolysis is one of the interventions commonly used to alleviate chronic pain conditions. However, healthcare providers and insurance companies must understand the appropriate CPT codes for pain management procedures to ensure accurate billing and insurance coverage. In this article, we will provide a comprehensive guide to CPT codes for percutaneous adhesiolysis in pain management, including the most commonly used codes and their significance. What is Percutaneous Adhesiolysis? Percutaneous adhesiolysis is a minimally invasive procedure used in pain management to treat chronic pain conditions caused by scar tissue or adhesions. The procedure involves inserting a needle into the epidural space and injecting a solution to dissolve or break up adhesions causing pain. The procedure is often performed under fluoroscopy guidance to ensure accurate placement of the needle and avoid complications. Why are CPT Codes for Pain Management Procedures Important? CPT codes for pain management procedures are essential because they determine how healthcare providers are reimbursed for their services. Each CPT code represents a specific procedure or service and has a corresponding fee schedule that providers use to determine the cost of the service. Healthcare providers must use the appropriate CPT codes for pain management procedures to ensure accurate billing and insurance coverage. Most Common CPT Codes for Percutaneous Adhesiolysis in Pain Management There are several CPT codes used for percutaneous adhesiolysis in pain management, depending on the specific procedure performed and the number of levels treated. The most commonly used CPT codes for percutaneous adhesiolysis include: 62311 - Percutaneous injection of substance into the spinal canal of thoracic, lumbar, or sacral spine. 62318 - Injection(s), including indwelling catheter placement, continuous infusion or intermittent bolus, of diagnostic or therapeutic substance(s) (e.g., anesthetic, antispasmodic, opioid, steroid, other solution), not including neurolytic substances, including needle or catheter placement, interlaminar epidural or subarachnoid, cervical or thoracic; lumbar or sacral (caudal). 62287 - Injection(s), including indwelling catheter placement, continuous infusion or intermittent bolus, of neurolytic substance(s) (e.g., alcohol, phenol, 10% dextrose) including neuraxial facet joint nerve; lumbar or sacral (caudal). It is essential to consult with your healthcare provider and insurance carrier to determine the appropriate CPT code for your specific procedure, as the codes may vary depending on the specific procedure performed and the insurance carrier. CPT codes for percutaneous adhesiolysis in pain management are essential to ensure accurate medical billing and insurance coverage. The most commonly used CPT codes for percutaneous adhesiolysis include 62311, 62318, and 62287. Healthcare providers and insurance companies must be familiar with these codes to ensure that patients receive the care they need without financial burden. If you're experiencing chronic pain, talk to your healthcare provider to see if percutaneous adhesiolysis is a viable treatment option. And for healthcare providers, make sure that you use the proper CPT codes for pain management procedures to ensure proper billing and reimbursement. By following the proper guidelines for medical billing, we can ensure that patients receive the care they need while minimizing financial hardship. CPT Codes for Discography in Pain Management Discography is a diagnostic procedure commonly used in pain management to determine the source of back pain. It involves injecting a contrast dye into the discs of the spine and imaging the results. CPT codes are used to report medical procedures and services. In this article, we will discuss the CPT codes for discography in pain management. CPT Code 62290: CPT code 62290 is used to report discography performed on one to three spinal levels. This code is commonly used when performing lumbar discography. CPT Code 62291: CPT code 62291 is used to report discography performed on four or more spinal levels. This code is commonly used when performing thoracic or cervical discography. CPT Code 77002: CPT code 77002 is used to report fluoroscopic guidance for procedures performed in the spine. This code is often reported with discography procedures to provide guidance during the injection process. CPT Code 77003: CPT code 77003 is used to report radiological supervision and interpretation for procedures performed in the spine. This code is often reported with discography procedures to provide radiological interpretation of the results. CPT codes play a critical role in reporting medical procedures and services, including discography in pain management. CPT codes 62290 and 62291 are used to report discography procedures performed on one to three spinal levels and four or more spinal levels, respectively. CPT codes 77002 and 77003 are used to report fluoroscopic guidance and radiological supervision and interpretation for discography procedures. Healthcare providers should ensure accurate coding and documentation to ensure appropriate reimbursement and compliance with coding guidelines. By understanding the CPT codes for discography in pain management, healthcare providers can ensure accurate reporting and optimize their revenue cycle management. 5 Ways Medical Billing Software Can Help You Address Denials and Appeals Denials and appeals are common challenges in medical billing. They can be time-consuming and frustrating for healthcare providers and can have a significant impact on the financial performance of healthcare practices. Medical billing software can be a valuable tool in addressing denials and appeals. In this article, we will discuss five ways medical billing software can help you address denials and appeals. Automated Denial Management: Medical billing software can help healthcare providers automate the denial management process. This includes tracking denials, identifying trends, and generating reports to help healthcare providers address the root cause of denials and implement corrective actions. Real-Time Claim Tracking: Medical billing software provides real-time claim tracking, allowing healthcare providers to monitor the status of claims and identify potential issues before they become denials. This can help to improve the chances of first-pass claim acceptance and reduce the number of denials. Advanced Reporting: Medical billing software provides advanced reporting capabilities, allowing healthcare providers to generate custom reports on denial rates, claim rejections, and other key performance indicators. This can help to identify trends and areas for improvement, allowing healthcare providers to take corrective actions. Appeals Management: Medical billing software can help healthcare providers manage the appeals process by providing a centralized platform for tracking and managing appeals. This can help to improve the efficiency and effectiveness of the appeals process and reduce the time and resources required to address appeals. Integrated Analytics: Medical billing software can provide integrated analytics, allowing healthcare providers to identify patterns and trends in claim denials and appeals. This can help healthcare providers to develop proactive strategies for addressing denials and appeals and optimizing their revenue cycle management. Medical billing software can be a valuable tool in addressing denials and appeals in medical billing. By automating denial management, providing real-time claim tracking, offering advanced reporting, managing appeals, and providing integrated analytics, medical billing software can help healthcare providers improve their financial performance and streamline their operations. Healthcare providers should consider investing in medical billing software to optimize their revenue cycle management and improve their financial performance. The US Healthcare Consulting Services Market - A Comprehensive Guide for the Modern Healthcare Professional In today's rapidly evolving healthcare landscape, the US Healthcare Consulting Services Market is gaining significant traction. This market offers a wide range of services that cater to various healthcare professionals, including surgeons, physicians, medical billers, and even hospital CEOs. This blog post aims to provide a comprehensive overview of the US Healthcare Consulting Services Market, touching upon its key players, services offered, and the benefits it brings to the healthcare sector. By the end of this post, you'll have a better understanding of how the US Healthcare Consulting Services Market can positively impact your organization. Understanding the US Healthcare Consulting Services Market The US Healthcare Consulting Services Market consists of numerous consulting firms that provide a variety of services tailored to the unique needs of healthcare professionals. These services range from strategic planning and operational improvements to financial management and IT solutions. The main goal of the US Healthcare Consulting Services Market is to help healthcare organizations stay competitive and deliver high-quality patient care by optimizing their processes, cutting costs, and implementing innovative solutions. Key Players in the US Healthcare Consulting Services Market Several prominent firms dominate the US Healthcare Consulting Services Market, offering specialized services to healthcare professionals. Some of the key players include:
Services Offered in the US Healthcare Consulting Services Market The US Healthcare Consulting Services Market offers a diverse range of services to cater to various healthcare professionals. These include:
Benefits of Leveraging the US Healthcare Consulting Services Market By partnering with a consulting firm in the US Healthcare Consulting Services Market, healthcare organizations can reap several benefits:
The US Healthcare Consulting Services Market offers a valuable resource for healthcare professionals looking to optimize their organizations and stay competitive in today's fast-paced industry. By partnering with experienced consulting firms, healthcare organizations can benefit from specialized expertise, enhanced operational efficiency, and improved patient care. Don't hesitate to explore the US Healthcare Consulting Services Market and unlock your organization's full potential. Understanding CPT Codes for Implantable Pain Pumps in Pain Management Implantable pain pumps are a type of medical device used to manage chronic pain. These devices are implanted under the skin and deliver medication directly to the spinal cord. Proper coding of implantable pain pump procedures is essential for accurate reimbursement and revenue cycle management. In this article, we will discuss CPT codes for implantable pain pumps in pain management. CPT Code 62350: CPT code 62350 is used to report the implantation of an intrathecal catheter for drug delivery systems, including implantable pain pumps. This code covers the placement of a catheter into the spinal cord for medication delivery. CPT Code 62351: CPT code 62351 is used to report the implantation of a subcutaneous or submuscular drug delivery system, including implantable pain pumps. This code covers the placement of a device under the skin or muscle for medication delivery. CPT Code 62355: CPT code 62355 is used to report the replacement or revision of an intrathecal catheter for drug delivery systems, including implantable pain pumps. This code covers the replacement or revision of a catheter that has already been implanted. CPT Code 62362: CPT code 62362 is used to report the removal of an intrathecal catheter for drug delivery systems, including implantable pain pumps. This code covers the removal of a catheter from the spinal cord. Proper coding of implantable pain pump procedures is essential for accurate reimbursement and revenue cycle management in pain management practices. CPT codes 62350, 62351, 62355, and 62362 are used to report the implantation, replacement or revision, and removal of intrathecal catheters and drug delivery systems, including implantable pain pumps. Pain management practices should ensure they are using the correct CPT codes for implantable pain pumps to ensure accurate reimbursement and optimize their revenue cycle management. The Growing US Healthcare Consulting Services Market: Key Trends and Opportunities The US Healthcare Consulting Services Market has been experiencing significant growth in recent years. This is due, in part, to the increasing complexity of the healthcare landscape and the need for expert guidance to navigate the challenges faced by healthcare providers. In this blog post, we will explore the driving forces behind the expansion of the US Healthcare Consulting Services Market and discuss the opportunities this presents for Surgeons, Physicians, Medical Billers, Medical Coders, IT Healthcare Professionals, Hospital CEOs, Healthcare Executives, Nurse Case Managers, Office Managers, Revenue Cycle Management Directors, Hospital CEOs, Hospital CFOs, Office Administrators, Healthcare Consultants, IT Consultants, Chief Nursing Officers, Medical Office Staff, Clinicians, and Medical Directors. Increasing regulations and compliance requirements One of the primary drivers of growth in the US Healthcare Consulting Services Market is the ever-changing regulatory environment. As healthcare providers face new rules and regulations, they often require the expertise of healthcare consultants to ensure compliance and avoid costly penalties. This creates a continuous demand for consulting services, as providers need guidance on how to navigate these complex requirements. Shift towards value-based care The transition to value-based care models has led to significant changes in the US Healthcare Consulting Services Market. Healthcare providers are now seeking the assistance of consulting firms to optimize patient outcomes while reducing costs. This transformation has created a need for consulting services that can help providers adapt their practices to align with new payment models and performance metrics. Technological advancements and digitalization As technology continues to evolve, the US Healthcare Consulting Services Market has seen an increased demand for IT consulting services. Healthcare organizations require assistance in implementing new technologies, such as electronic health records (EHRs), telemedicine platforms, and data analytics tools. Additionally, there is a growing need for cybersecurity consulting as healthcare providers face an increasing number of cyber threats. Mergers and acquisitions The US Healthcare Consulting Services Market has also been impacted by the growing trend of mergers and acquisitions within the healthcare industry. As healthcare providers consolidate, they often require the services of healthcare consultants to assist with integration, financial planning, and operational efficiencies. Workforce challenges The US Healthcare Consulting Services Market is poised to benefit from the ongoing challenges faced by healthcare providers in managing their workforce. Issues such as clinician burnout, staff turnover, and the need for ongoing training and education create opportunities for healthcare consultants to offer valuable expertise and support. Revenue cycle management and financial optimization The US Healthcare Consulting Services Market continues to thrive as healthcare providers seek assistance with revenue cycle management and financial optimization. Consultants can offer guidance on improving billing and coding processes, negotiating payer contracts, and identifying new revenue streams, all of which contribute to financial stability and growth for healthcare organizations. The US Healthcare Consulting Services Market offers numerous opportunities for professionals within the healthcare industry. As the landscape continues to evolve, the demand for expert guidance and support will only continue to grow. By staying informed of these key trends and challenges, Surgeons, Physicians, Medical Billers, Medical Coders, IT Healthcare Professionals, Hospital CEOs, Healthcare Executives, Nurse Case Managers, Office Managers, Revenue Cycle Management Directors, Hospital CEOs, Hospital CFOs, Office Administrators, Healthcare Consultants, IT Consultants, Chief Nursing Officers, Medical Office Staff, Clinicians, and Medical Directors can position themselves to take advantage of the expanding US Healthcare Consulting Services Market and improve the overall quality of care for their patients.
CPT Codes for Psychological Testing in Pain Management: A Comprehensive Guide Psychological testing is a crucial aspect of pain management, especially when it comes to chronic pain conditions. It helps physicians understand the underlying psychological factors that contribute to pain and develop a comprehensive treatment plan. Proper coding of psychological testing procedures is important for accurate billing and reimbursement. In this article, we will discuss the CPT codes used for psychological testing in pain management. CPT Code 96130: CPT code 96130 is used for psychological testing evaluation services by a physician or other qualified healthcare professional. This code includes the administration and interpretation of standardized tests and measures, and the integration of the data into a diagnostic and treatment plan. CPT Code 96131: CPT code 96131 is used for psychological testing evaluation services by a technician or other qualified healthcare professional. This code includes the administration and scoring of standardized tests and measures, with subsequent communication of results and integration of data into a diagnostic and treatment plan by a physician or other qualified healthcare professional. CPT Code 96136: CPT code 96136 is used for psychological or neuropsychological testing administered by a computer with qualified healthcare professional interpretation and report. This code includes the administration of the test, the interpretation of the results, and the preparation of a report. CPT Code 96137: CPT code 96137 is used for psychological or neuropsychological testing administered by a technician with qualified healthcare professional interpretation and report. This code includes the administration of the test, the scoring of the results, and subsequent communication of results and integration of data into a diagnostic and treatment plan by a physician or other qualified healthcare professional. Proper coding of psychological testing procedures is critical for accurate billing and reimbursement in pain management. Healthcare providers should be familiar with the CPT codes used for psychological testing and ensure that they are coded accurately to avoid potential claim denials. By using the correct CPT codes, healthcare providers can ensure accurate billing and reimbursement for psychological testing procedures. It is important to note that these codes may vary depending on the type of psychological testing performed and the specific circumstances of the patient. Therefore, it is recommended that healthcare providers consult the latest coding guidelines and seek professional coding advice as needed to ensure accurate billing and reimbursement. The Benefits of Medical Billing Software for Solo Practitioners: A Comprehensive Guide Medical billing is a crucial aspect of any healthcare practice, including solo practitioners. However, the process can be time-consuming and prone to errors. Medical billing software can help streamline the process and improve efficiency, accuracy, and revenue. In this article, we will discuss the benefits of medical billing software for solo practitioners. Improved Efficiency: Medical billing software automates many of the tasks involved in the billing process, such as claim submissions, payment posting, and patient billing. This frees up time for solo practitioners to focus on patient care and other important tasks. Increased Accuracy: Medical billing software reduces the risk of errors in the billing process, such as coding mistakes, claim denials, and incorrect billing. This helps to ensure accurate and timely reimbursement, which is critical for the financial health of solo practices. Enhanced Revenue: Medical billing software can help solo practitioners increase their revenue by reducing the number of claim denials, improving collections, and optimizing reimbursement rates. This can have a significant impact on the bottom line of solo practices. Improved Patient Experience: Medical billing software can improve the patient experience by providing easy-to-understand billing statements and offering online payment options. This can help to reduce patient frustration and improve patient satisfaction, which is important for patient retention and practice growth. Medical billing software offers numerous benefits for solo practitioners, including improved efficiency, increased accuracy, enhanced revenue, and improved patient experience. Solo practitioners should consider investing in medical billing software to streamline their billing process, reduce errors, and improve financial performance. With the right medical billing software, solo practitioners can focus on providing quality patient care while ensuring accurate and timely reimbursement. 5 Steps for Effective Prior Authorization Appeals Prior authorization is a process used by insurance companies to determine whether they will cover a specific medical procedure, test, or medication. Unfortunately, prior authorization requests are often denied, which can be frustrating and time-consuming for both healthcare providers and patients. In this article, we will discuss five steps for effective prior authorization appeals. Understand the Denial Before appealing a prior authorization denial, it's essential to understand why the request was denied. This includes reviewing the insurance company's reason for denial and any documentation they provided. Gather Information To appeal a prior authorization denial, it's crucial to gather all relevant information. This includes the patient's medical records, the specific procedure or medication being requested, and any other relevant documentation. Submit a Detailed Appeal When submitting a prior authorization appeal, it's essential to provide a detailed explanation of why the procedure, test, or medication is necessary. This includes providing any relevant medical literature or studies that support the request. Follow Up After submitting a prior authorization appeal, it's essential to follow up with the insurance company regularly. This includes calling to check on the status of the appeal and providing any additional information they may request. Consider Outside Help If prior authorization appeals are becoming a significant issue for your medical practice, it may be worth considering outside help. This can include hiring a third-party vendor or consultant to manage prior authorization appeals on your behalf. Prior authorization denials can be frustrating and time-consuming for healthcare providers and patients. By following these five steps for effective prior authorization appeals, healthcare providers can increase their chances of receiving approval for necessary procedures, tests, and medications. Remember to understand the denial, gather information, submit a detailed appeal, follow up, and consider outside help if necessary. By doing so, you can ensure that your patients receive the care they need, while minimizing the administrative burden on your medical practice. Enhance Your Practice with Full-Spectrum RCM Services for Interventional Pain Management Interventional pain management is a growing field in healthcare, offering patients relief from chronic pain through minimally invasive procedures. However, managing the revenue cycle for an interventional pain management practice can be complex and time-consuming. Full-Spectrum RCM Services for Interventional Pain Management, like those offered by GoHealthcare Practice Solutions, are designed to help practices streamline their revenue cycle management, allowing physicians to focus on providing exceptional patient care. The Importance of Full-Spectrum RCM Services for Interventional Pain Management Full-Spectrum RCM Services for Interventional Pain Management are essential to the financial success and stability of a practice. These services encompass every aspect of the revenue cycle, from patient registration and eligibility verification to billing, coding, and collections. By utilizing Full-Spectrum RCM Services for Interventional Pain Management, practices can ensure that their revenue cycle is optimized for maximum efficiency and profitability. Key Components of Full-Spectrum RCM Services for Interventional Pain Management
In conclusion, Full-Spectrum RCM Services for Interventional Pain Management are essential to the success of any interventional pain management practice. GoHealthcare Practice Solutions offers comprehensive, tailored solutions to help practices navigate the complexities of the revenue cycle, allowing physicians to focus on providing exceptional patient care. By partnering with GoHealthcare Practice Solutions for your Full-Spectrum RCM Services for Interventional Pain Management needs, you can be confident that your practice is in capable hands, ensuring financial stability and success for years to come. Mastering Healthcare Financial Management for Orthopedic Surgeons: The Key to a Successful Practice3/22/2023 Mastering Healthcare Financial Management for Orthopedic Surgeons: The Key to a Successful Practice In today's competitive healthcare landscape, effective Healthcare Financial Management for Orthopedic Surgeons is more critical than ever. Balancing quality patient care with the complexities of medical billing, insurance navigation, and revenue cycle management can be challenging. This article explores the importance of Healthcare Financial Management for Orthopedic Surgeons and how GoHealthcare Practice Solutions can support your practice's financial success. The Importance of Healthcare Financial Management for Orthopedic Surgeons Healthcare Financial Management for Orthopedic Surgeons plays a significant role in the overall success of a practice. As an orthopedic surgeon, you are responsible for providing exceptional patient care while ensuring that your practice remains financially viable. Effective Healthcare Financial Management for Orthopedic Surgeons allows you to focus on what you do best—delivering outstanding care to your patients—while your practice remains profitable and compliant with ever-changing healthcare regulations. Challenges in Healthcare Financial Management for Orthopedic Surgeons Navigating the complexities of Healthcare Financial Management for Orthopedic Surgeons can be a daunting task. Some common challenges include managing billing and coding, coordinating insurance benefits, handling out-of-network and in-network providers, and staying compliant with HIPAA and other regulations. These challenges can be time-consuming and may detract from your primary focus: providing excellent patient care. The GoHealthcare Practice Solutions Advantage GoHealthcare Practice Solutions specializes in Healthcare Financial Management for Orthopedic Surgeons, offering comprehensive and customized solutions to help your practice thrive. Our experienced team understands the unique financial needs of orthopedic surgery practices and provides a wide range of services, including revenue cycle management, medical billing and coding, insurance navigation, and more. Customized Solutions for Healthcare Financial Management for Orthopedic Surgeons At GoHealthcare Practice Solutions, we know that no two practices are alike. That's why we tailor our Healthcare Financial Management for Orthopedic Surgeons services to meet your practice's specific needs. Our customized solutions help you optimize your revenue cycle, streamline your workflow, and ensure compliance with healthcare regulations. Expert Support for Healthcare Financial Management for Orthopedic Surgeons Partnering with GoHealthcare Practice Solutions means you'll have a team of experts by your side, dedicated to the success of your practice. Our knowledgeable staff has extensive experience in Healthcare Financial Management for Orthopedic Surgeons and is committed to helping you overcome the financial challenges that come with running a successful practice. A Comprehensive Approach to Healthcare Financial Management for Orthopedic Surgeons At GoHealthcare Practice Solutions, we believe that effective Healthcare Financial Management for Orthopedic Surgeons requires a comprehensive approach. We offer a wide range of services, from patient registration and eligibility verification to insurance benefit coordination and payment plan setup. Our commitment to comprehensive Healthcare Financial Management for Orthopedic Surgeons ensures that your practice is well-equipped to navigate the complex world of healthcare finance. In conclusion, effective Healthcare Financial Management for Orthopedic Surgeons is essential for the success of your practice. By partnering with GoHealthcare Practice Solutions, you can focus on providing exceptional patient care while we handle the financial complexities. Our customized solutions, expert support, and comprehensive approach to Healthcare Financial Management for Orthopedic Surgeons make us the ideal partner for your practice. To learn more about how GoHealthcare Practice Solutions can help you achieve financial success, visit our website at https://www.gohealthcarellc.com. Enhancing Patient Care with Interventional Pain Management Practice Support Interventional pain management has become a rapidly growing field, offering relief to millions of patients suffering from chronic pain. To effectively serve patients and streamline operations, practices need access to specialized Interventional Pain Management Practice Support. GoHealthcare Practice Solutions is at the forefront of providing comprehensive, tailored services designed to enhance patient care and optimize practice performance. Understanding the Need for Interventional Pain Management Practice Support In recent years, the demand for non-surgical, minimally invasive treatments for pain has skyrocketed, increasing the need for dedicated Interventional Pain Management Practice Support. GoHealthcare Practice Solutions understands that a well-functioning practice is essential to providing the best possible patient care. Our Interventional Pain Management Practice Support services cater to the unique needs of pain management clinics. We work closely with your practice to identify areas of improvement and implement strategies that streamline processes, reduce overhead, and optimize patient outcomes. Comprehensive Services Offered by GoHealthcare Practice Solutions GoHealthcare Practice Solutions' Interventional Pain Management Practice Support includes a wide array of services to enhance your practice's performance:
The GoHealthcare Practice Solutions Advantage Choosing GoHealthcare Practice Solutions for your Interventional Pain Management Practice Support means partnering with a team of experienced professionals who understand the intricacies of your field. Our specialized knowledge and commitment to innovation make us the ideal choice for Interventional Pain Management Practice Support. With our help, your practice can thrive and continue to provide exceptional patient care. In conclusion, GoHealthcare Practice Solutions is your one-stop solution for comprehensive Interventional Pain Management Practice Support. With a focus on enhancing patient care and optimizing practice performance, our team is dedicated to helping your practice achieve and maintain success. Experience the difference of working with industry experts by choosing GoHealthcare Practice Solutions for your Interventional Pain Management Practice Support needs. Best EHR Software for a Small Practice in 2023: Top Choices for Your Healthcare Team As a healthcare professional, finding the best EHR software for a small practice in 2023 is crucial to streamline your workflow and enhance the patient experience. At GoHealthcare Practice Solutions, we understand the challenges faced by small practices. With this comprehensive list, we aim to simplify your decision-making process and help you choose the best EHR software for small practices that meet your unique needs. AmazingCharts AmazingCharts is a user-friendly EHR system designed to cater to small practices. With its intuitive interface and robust features, it is an excellent choice for clinicians seeking the best EHR software for a small practice in 2023. AmazingCharts offers customizable templates, integrated practice management software, and secure patient communication portals to streamline your workflow. Kareo Kareo is another top contender for the best EHR software for small practices in 2023. This cloud-based platform offers a complete solution, combining EHR, practice management software, and medical billing services. Kareo's user-friendly interface and customizable features make it suitable for various medical specialties and staff roles, including office administrators and nurse case managers. Athenahealth Athenahealth is a popular choice for the best EHR software for a small practice in 2023, as it offers a comprehensive suite of cloud-based services, including EHR, practice management, and patient engagement tools. With its revenue cycle management capabilities, Athenahealth is well-suited for medical billers, coders, and revenue cycle management directors. eClinicalWorks As one of the best EHR software for small practices, eClinicalWorks provides a comprehensive suite of EHR and practice management solutions. Its robust features cater to various healthcare professionals, including office managers, healthcare consultants, and chief nursing officers. With its patient engagement tools and interoperability capabilities, eClinicalWorks can improve care coordination and patient satisfaction. Greenway Health Greenway Health's EHR, Intergy, is an excellent choice for the best EHR software for a small practice in 2023. With its intuitive interface and comprehensive features, Intergy is suitable for various medical specialties and roles, such as clinicians, surgery schedulers, and prior authorization experts. Additionally, Greenway Health offers revenue cycle management services and practice analytics to optimize your financial performance. Selecting the best EHR software for a small practice in 2023 can be a daunting task, but this list aims to make the decision easier for you and your team. By considering factors like ease of use, customization, and integration with other systems, you can find the best EHR software for small practices that fit your unique needs. At GoHealthcare Practice Solutions, we are committed to helping healthcare professionals succeed in their practice. Whether you're a physician, office administrator, or medical director, our goal is to provide you with the resources and support you need to thrive. You are going to love our amazing team! So visit our website at https://www.gohealthcarellc.com to learn more about our services and how we can help your practice reach new heights in 2023. |

ABOUT THE AUTHOR:
Ms. Pinky Maniri-Pescasio is the Founder of GoHealthcare Consulting. She is a National Speaker on Practice Reimbursement and a Physician Advocate. She has served the Medical Practice Industry for more than 25 years as a Professional Medical Practice Consultant. search hereArchives
March 2024
Categories
All
BROWSE HERE
All
|
- About
- What we do.
- FREE ASSESSMENT
- Testimonials
- READ OUR BLOG
-
Let's Meet in Person
- 2023 ORTHOPEDIC VALUE BASED CARE CONFERENCE
- 2023 AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
- 2023 ASIPP 25th Annual Meeting of the American Society of Interventional Pain Management
- 2023 Becker's 20th Annual Spine, Orthopedic & Pain Management-Driven ASC Conference
- 2023 FSIPP Annual Conference by FSIPP FSPMR Florida Society Of Interventional Pain Physicians
- 2023 New York and New Jersey Pain Medicine Symposium
- Frequently Asked Questions and Answers - GoHealthcare Practice Solutions
- Readers Questions
Photos from shixart1985 (CC BY 2.0), www.ilmicrofono.it, shixart1985





















































 RSS Feed
RSS Feed